What is the ICD 10 code for urinary incontinence?
Unspecified urinary incontinence 2016 2017 2018 2019 2020 2021 Billable/Specific Code R32 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2021 edition of ICD-10-CM R32 became effective on October 1, 2020.
What is the ICD 10 code for splitting of urinary stream?
Splitting of urinary stream. R39.13 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for urethral stricture?
Urethral stricture, unspecified 1 N35.9 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. 2 The 2021 edition of ICD-10-CM N35.9 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of N35.9 - other international versions of ICD-10 N35.9 may differ.
What is the ICD 10 code for involuntary passage of urine?
Involuntary passage of urine occurring soon after a strong sense of urgency to void ICD-10-CM N39.41 is grouped within Diagnostic Related Group (s) (MS-DRG v38.0): 695 Kidney and urinary tract signs and symptoms with mcc 696 Kidney and urinary tract signs and symptoms without mcc
What is the ICD-10 diagnosis code for urethral stricture?
ICD-10 code N35. 9 for Urethral stricture, unspecified is a medical classification as listed by WHO under the range - Diseases of the genitourinary system .
What is the ICD-10 code for bulbar urethral stricture?
Post-traumatic bulbous urethral stricture N35. 011 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM N35. 011 became effective on October 1, 2021.
What is urethral stricture?
Overview. A urethral (u-REE-thrul) stricture involves scarring that narrows the tube that carries urine out of your body (urethra). A stricture restricts the flow of urine from the bladder and can cause a variety of medical problems in the urinary tract, including inflammation or infection.
What is the code for stenosis of the urethra?
9: Urethral stricture, unspecified.
What is a bulbar urethral stricture?
What is bulbar urethral stricture? Bulbar (meaning “bulb shaped”) urethral stricture is an obstruction of urine flow through the urethra, which impedes the body's ability to pass urine.
What is Fossa Navicularis stricture?
Stricture of fossa navicularis is most often caused by lichen sclerosus et atrophicus and instrumentation. Direct visual internal urethrotomy is limited to selected cases in the management of pendulous urethral stricture.
Can a urethral stricture cause incontinence?
The symptoms of a urethral stricture are usually related to problems emptying the bladder. These include a slow or interrupted urinary stream, incomplete bladder emptying or inability to urinate. Sometimes these can be associated with urinary frequency, urgency, or urgency incontinence.
Does urethral dilation cause incontinence?
Urethral coitus usually causes severe urethral dilatation and urinary incontinence but in some cases urinary incontinence may not be seen. If severely dilated urethra is seen during the physical examination, physician must think about urethral sex and ask additional questions about sexual intercourse.
What is the most common cause of urethral stricture?
Trauma or injury. Injury to the urethra or pelvis is the most common cause of urethral stricture. A fall onto your scrotum or perineum, the space between your scrotum and anus, or a fracture in your pelvis can cause inflammation and scarring.
What is cystourethroscopy CPT code?
You would use CPT code 52000 cystourethroscopy.
How is a urethral stricture treated?
Treatments include: dilation – enlarging the stricture with gradual stretching. urethrotomy – cutting the stricture with a laser or knife through a scope. open surgery – surgical removal of the stricture with reconnection and reconstruction, possibly with grafts (urethroplasty)
What is the CPT code for urethral dilation?
CPT® Code 53600 in section: Dilation of urethral stricture by passage of sound or urethral dilator, male.
What is the most common type of incontinence?
Here’s a quick refresher of the most common types of incontinence: Stress urinary incontinence (N39.3) is an involuntary loss of urine with a sudden increase in abdominal pressure. These patients leak when they sneeze, laugh, cough, or exercise. It is the most common type of incontinence.
How long does it take for a woman to see a reduction in urine leaks?
After several weeks of treatment for 20–30 minutes per day, most women see a reduction in urine leaks. External e-stim devices achieve similar results but are much less invasive. E-stim is sent through the skin, without vaginal insertion.
What are the different types of incontinence?
Major types of incontinence include urinary urge incontinence and urinary stress incontinence. Urinary incontinence is loss of bladder control. Symptoms can range from mild leaking to uncontrollable wetting. It can happen to anyone, but it becomes more common with age.
What causes incontinence?
There are other causes of incontinence, such as prostate problems and nerve damage.treatment depends on the type of problem you have and what best fits your lifestyle. It may include simple exercises, medicines, special devices or procedures prescribed by your doctor, or surgery. Codes.
What does it mean when you can't hold your urine in your bladder?
Inability to hold urine in the bladder. Involuntary discharge of urine after expected age of completed development of urinary control. This can happen during the daytime (diurnal enuresis) while one is awake or during sleep (nocturnal enuresis).
Is enuresis a symptom of incontinence?
Involuntary loss of urine, such as leaking of urine. It is a symptom of various underlying pathological processes. Major types of incontinence include urinary urge incontinence and urinary stress incontinence.
What is urinary incontinence?
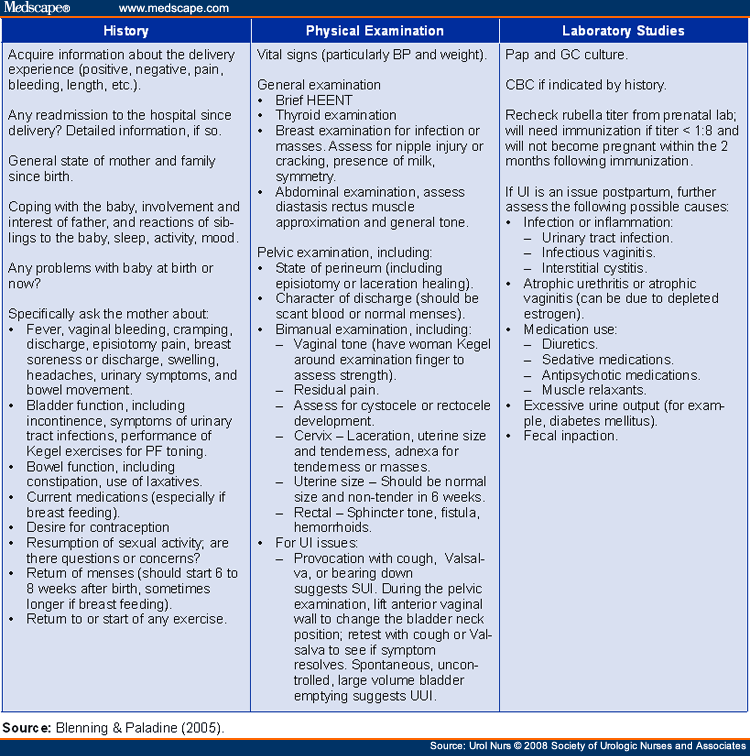
Urinary incontinence (UI) is defined by the International Continence Society as the complaint of any involuntary leakage of urine.3 One component of the ICS standardization divides pelvic floor muscle dysfunction symptoms into five groups: lower urinary tract symptoms, bowel symptoms, sexual function, prolapse, and pain.4 It is of note that many of these symptoms occur simultaneously and are relevant to each other. In this report, we will focus on lower urinary tract symptoms: urinary incontinence, urgency and frequency, slow or intermittent urine stream and straining, and feeling of incomplete emptying.
What is the best medication for urgency urinary incontinence?
Common medications to treat urgency or urgency urinary incontinence have historically included anticholinergics/antimuscarinic agents: oxybutynin, tolterodine, solifenacin, hyoscyamine, fesoterodine and darifenacin. These drugs are sold under the names of: Ditropan, Detrol, Vesicare, Enablex, Levbid, Cytospaz, Toviaz and Oxytrol. Anticholinergic/antispasmodic drugs are one of the first choices for OAB, as they have been proven to be the most effective agents in suppressing premature detrusor contractions, enhancing bladder storage, and relieving symptoms.9,10 Anticholinergic and antispasmodic agents act by antagonizing cholinergic muscarinic receptors, through which different parasympathetic nerve impulses evoke detrusor contraction Side effects of these medications can be bothersome and include dry mouth, headache, constipation, blurred vision, and confusion.1 Many patients do not continue medications beyond 9 months due to these bothersome side effects.11 A newer class of drugs, beta-3 adrenergic agonists, are mostly currently being used if anticholinergic agents are not effective. One medication, called mirabegron, sold under the name Myrbetriq, works differently than the anticholinergics, as it relaxes the bladder’s smooth muscle while it fills with urine, thereby increasing the bladder’s capacity to hold/store urine.12

Popular Posts:
- 1. icd 10 cm code for contusion of right forearm
- 2. icd 10 code for history of hypomagnesemia
- 3. icd 10 code for due to antineoplastic chemotherapy drug
- 4. icd 10 cm code for pseudoparathyroidism
- 5. icd 10 code for old cva non dominant weakness
- 6. icd 10 code for obverweeight
- 7. icd 10 code for thoracoabdominal coarctation of aorta
- 8. what is the correct icd 10 code for i50.23
- 9. icd 10 code for coronary angioplasty
- 10. icd 9 code for emmetropia