What is the ICD 10 code for vestibular neuronitis?
Vestibular neuronitis 1 H81.2 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. 2 The 2021 edition of ICD-10-CM H81.2 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of H81.2 - other international versions of ICD-10 H81.2 may differ.
What is the new ICD 10 for Vertigo?
The 2022 edition of ICD-10-CM H81.2 became effective on October 1, 2021. This is the American ICD-10-CM version of H81.2 - other international versions of ICD-10 H81.2 may differ. Idiopathic inflammation of the vestibular nerve, characterized clinically by the acute or subacute onset of vertigo; nausea; and imbalance.
What is the ICD 10 code for Neurologic diagnosis?
G58.8 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2018/2019 edition of ICD-10-CM G58.8 became effective on October 1, 2018. This is the American ICD-10-CM version of G58.8 - other international versions of ICD-10 G58.8 may differ.
What is the ICD 10 code for excluded note?
M79.2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M79.2 became effective on October 1, 2021. This is the American ICD-10-CM version of M79.2 - other international versions of ICD-10 M79.2 may differ. A type 1 excludes note is a pure excludes.
What is the ICD 10 code for vestibular disorder?
ICD-10-CM Code for Unspecified disorder of vestibular function, unspecified ear H81. 90.
What is peripheral vestibular loss?
Produced by. Fact Sheet. Peripheral Vestibular Disorders. Peripheral Vestibular Disorders (PVD) include pathology of inner ear vestibular structures as well as the vestibular portion of the eighth cranial nerve. 1 Such pathology diminishes available sensory information regarding head position and movement.
What is a neuro vestibular disorder?
Vestibular neuritis is a disorder that affects the nerve of the inner ear called the vestibulocochlear nerve. This nerve sends balance and head position information from the inner ear to the brain.
What is unspecified disorder of vestibular function?
Unspecified disorder of vestibular function A disorder characterized by dizziness, imbalance, nausea, and vision problems. Pathological processes of the vestibular labyrinth which contains part of the balancing apparatus. Patients with vestibular diseases show instability and are at risk of frequent falls.
Is vestibular nerve central or peripheral?
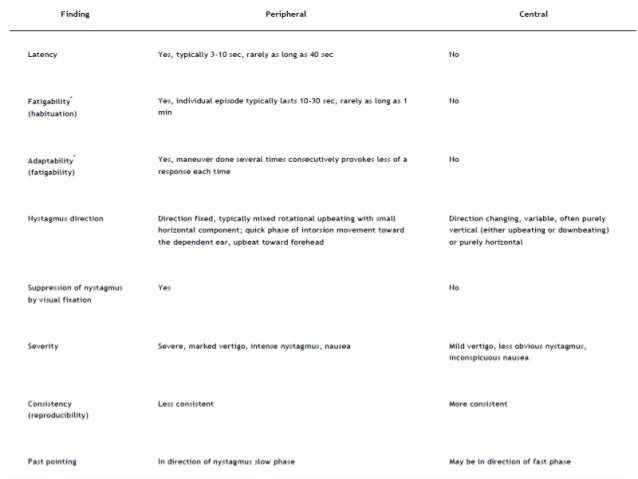
Neuroanatomically and functionally, the vestibular system can be divided into peripheral and central components. The membranous labyrinth and the vestibular portion of the vestibulocochlear nerve are the peripheral vestibular components in the inner ear.
Where is the vestibular nerve?
Assorted References. Vestibular receptors are located in the semicircular canals of the ear, which provide input on rotatory movements (angular acceleration), and in the utricle and saccule, which generate information on linear acceleration and the influence of gravitational pull.
What is the difference between vertigo and vestibular disorder?
Dizziness and vertigo are symptoms of a vestibular balance disorder. Balance disorders can strike at any age, but are most common as you get older. Your ear is a complex system of bone and cartilage. Within it is a network of canals.
What is the most common vestibular disorder?
Benign paroxysmal positional vertigo (BPPV) is considered the most common peripheral vestibular disorder, affecting 64 of every 100,000 Americans.
What happens if the vestibular system is damaged?
Disorders of the vestibular system result from damage to either the peripheral or central system that regulate and control our ability to balance. These disorders can lead to symptoms like dizziness, decreased balance, proprioception problems, vision changes, vertigo or hearing changes.
What are common vestibular disorders?
Common vestibular disorders include:Acoustic neuroma.Barotrauma.Benign paroxysmal positional vertigo (BPPV)Inner ear malformations.Labyrinthitis or vestibular neuritis.Mal de débarquement.Ménière's disease.Migraine-associated dizziness.More items...•
What is the ICD 10 code for neuropathy?
Hereditary and idiopathic neuropathy, unspecified G60. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM G60. 9 became effective on October 1, 2021.
What causes peripheral vestibular disorder?
Vestibular dysfunction is most commonly caused by head injury, aging, and viral infection. Other illnesses, as well as genetic and environmental factors, may also cause or contribute to vestibular disorders. Disequilibrium: Unsteadiness, imbalance, or loss of equilibrium; often accompanied by spatial disorientation.
What causes peripheral vestibular dysfunction?
Infections. Inner ear problems, such as poor circulation in the ear. Calcium debris in your semicircular canals. Problems rooted in your brain, such as traumatic brain injury.
What are the symptoms of peripheral vestibular disease?
The symptoms of peripheral and central vestibular dysfunction can overlap, and a proper physical exam can often help differentiate between the two. The patient's symptoms typically consist of vertigo, nausea, vomiting, intolerance to head motion, nystagmus, unsteady gait, and postural instability.
What is the most common symptom of vestibular dysfunction?
Dizziness and trouble with your balance are the most common symptoms, but you also can have problems with your hearing and vision.
How is peripheral vestibular disorder diagnosed?
MAGNETIC RESONANCE IMAGING (MRI) An MRI of the brain can reveal the presence of tumors, stroke damage, and other soft-tissue abnormalities that might cause dizziness or vertigo. MRIs of structures in and around the inner ear can be helpful in diagnosing vestibular disorders in some instances.
What is the ICd 10 code for vestibular dysfunction?
Disorders of vestibular function 1 H81 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. 2 The 2021 edition of ICD-10-CM H81 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of H81 - other international versions of ICD-10 H81 may differ.
What is vestibular labyrinth?
A disorder characterized by dizziness, imbalance, nausea, and vision problems. Pathological processes of the vestibular labyrinth which contains part of the balancing apparatus. Patients with vestibular diseases show instability and are at risk of frequent falls. Code History.
What are the symptoms of autonomic neuropathy?
Autonomic neuropathy symptoms can be heart intolerance, excess sweat or no sweat, blood pressure changes, bladder, bowel or digestive problems. Physician does a thorough physical examination including extremity neurological exam and noting vitals.
What is the term for two or more nerves in different areas?
Polyneuropathy – Two or more nerves in different areas get affected. Autonomic neuropathy – Affects the nerves which control blood pressure, sweating, digestion, heart rate, bowel and bladder emptying.
What tests are used to diagnose neuropathy?
Detailed history of the patient like symptoms, lifestyle and exposure to toxins may also help to diagnose neuropathy. Blood tests, CT, MRI, electromyography, nerve biopsy and skin biopsy are the tests used to confirm neuropathy.

Popular Posts:
- 1. 2015 icd 10 code for scalp hematoma rectal bleed
- 2. icd 9 code for pre ulcerative callus
- 3. icd 10 code for aggressive behavior
- 4. 2018 icd 10 code for status post hysterectomy
- 5. 2017 icd 10 code for history renal cell cancer
- 6. icd 9 code for pancreatic adenoma
- 7. icd 10 code for labial fusion
- 8. icd 9 code for lung ca
- 9. icd 10 code for need for influenza vaccination
- 10. icd 10 code for anticoagulated