What is the ICD 10 diagnosis code for?
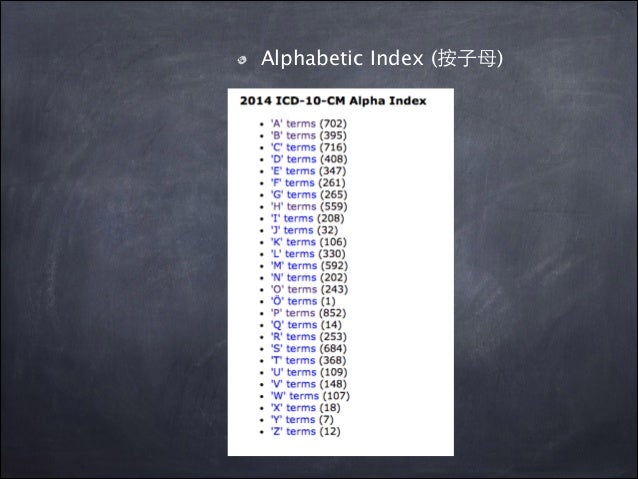
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.
What is ICD - 10 code for infected AV graft?
T82.898A is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2021 edition of ICD-10-CM T82.898A became effective on October 1, 2020. This is the American ICD-10-CM version of T82.898A - other international versions of ICD-10 T82.898A may differ.
What is the ICD 10 code for wound healing?
What is the ICD-10 code for drainage from wound? T81. 89XA is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2021 edition of ICD-10-CM T81. 89XA became effective on October 1, 2020.
What is the ICD 10 code for infected surgical wound?
- Application site infection
- Infected seroma after surgical procedure
- Infected seroma due to and following procedure
- Infection of tendon repair
- Infectious disorder of tendon
- Meningitis following procedure
- Organ surgical site infection
- Postoperative bacterial meningitis
- Postoperative infection
- Postoperative infection of thyroidectomy wound
What is the ICD-10 code for abdominal wound?
ICD-10-CM Code for Unspecified open wound of abdominal wall, unspecified quadrant without penetration into peritoneal cavity, initial encounter S31. 109A.
What is the ICD-10 code for wound infection?
ICD-10 Code for Local infection of the skin and subcutaneous tissue, unspecified- L08. 9- Codify by AAPC.
What is the ICD-10 code for intra-abdominal infection?
Intra-abdominal and pelvic swelling, mass and lump ICD-10-CM R19. 00 is grouped within Diagnostic Related Group(s) (MS-DRG v39.0): 391 Esophagitis, gastroenteritis and miscellaneous digestive disorders with mcc. 392 Esophagitis, gastroenteritis and miscellaneous digestive disorders without mcc.
How do you code a postoperative wound infection?
Postoperative wound infection is classified to ICD-9-CM code 998.59, Other postoperative infection. Code 998.59 also includes postoperative intra-abdominal abscess, postoperative stitch abscess, postoperative subphrenic abscess, postoperative wound abscess, and postoperative septicemia.
What is the ICD-10 code for surgical wound?
ICD-10 Code for Disruption of external operation (surgical) wound, not elsewhere classified, initial encounter- T81. 31XA- Codify by AAPC.
What is the ICD-10 code for non-healing wound?
998.83 - Non-healing surgical wound. ICD-10-CM.
What is a intra-abdominal infection?
Definitions. Intra-abdominal infection (IAI) describes a diverse set of diseases. It is broadly defined as peritoneal inflammation in response to microorganisms, resulting in purulence in the peritoneal cavity[1]. IAI are classified as uncomplicated or complicated based on the extent of infection[2].
What is abdomen infection?
Overview. Peritonitis is inflammation of the peritoneum — a silk-like membrane that lines your inner abdominal wall and covers the organs within your abdomen — that is usually due to a bacterial or fungal infection. There are two types of peritonitis: Spontaneous bacterial peritonitis.
How do you code an abdominal abscess?
ICD-10 code L02. 211 for Cutaneous abscess of abdominal wall is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
How do you code Post procedural sepsis?
Sepsis due to a postprocedural infection: For such cases, the postprocedural infection code should be coded first, such as: T80....2, severe sepsis.If the causal organism is not documented, code A41. ... An additional code should be assigned for the organ dysfunction severe sepsis is causing, such as, N17.More items...•
What is the ICD-10 code for postoperative abscess?
Postprocedural retroperitoneal abscess The 2022 edition of ICD-10-CM K68. 11 became effective on October 1, 2021.
What is the ICD-10 code for postoperative cellulitis of surgical wound?
4-, a post-procedural wound infection and post-procedural sepsis were assigned to the same ICD-10-CM code T81. 4-, Infection following a procedure with a code for the infection (sepsis, cellulitis, etc.)
What is the ICD-10 code for drainage from wound?
Z48. 0 - Encounter for attention to dressings, sutures and drains | ICD-10-CM.
Is cellulitis an infection?
Cellulitis is a common bacterial skin infection that causes redness, swelling, and pain in the infected area of the skin. If untreated, it can spread and cause serious health problems. Good wound care and hygiene are important for preventing cellulitis.
What qualifies as an open wound?
Unlike closed wounds, such as bruises or closed fractures, open wounds are injuries that involve a break in the skin and leave the internal tissue exposed. The skin has an important role in protecting the organs, tissues, and other structures inside the body, so a breach of the skin can potentially invite infection.
Is an abscess infectious?
A burst abscess can be very painful and cause the infection to spread. Treatment for tooth and other mouth abscesses is especially important. Untreated tooth abscesses can kill you. Untreated infections can spread to surrounding tissues in your body.
What is a type 1 exclude note?
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as S31. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
When is the ICd 10 code for S31 effective?
The 2021 edition of ICD-10-CM S31 became effective on October 1, 2020.
What is an open wound of the lower back and pelvis?
open wound of abdomen, lower back and pelvis ( S31 .-) Injuries to the spinal cord ( S34.0 and S34.1) refer to the cord level and not bone level injury, and can affect nerve roots at and below the level given.
What are the effects of foreign body in the genitourinary tract?
effects of foreign body in genitourinary tract ( T19.-) effects of foreign body in stomach, small intestine and colon ( T18.2- T18.4) frostbite ( T33-T34) insect bite or sting, venomous ( T63.4) Injuries to the abdomen, lower back, lumbar spine, pelvis and external genitals.
What is the ICd code for abdominal trauma?
The ICD code S31 is used to code Abdominal trauma. Abdominal trauma is an injury to the abdomen. It may be blunt or penetrating and may involve damage to the abdominal organs. Signs and symptoms include abdominal pain, tenderness, rigidity, and bruising of the external abdomen. Abdominal trauma presents a risk of severe blood loss and infection.
What is the ICD code for acute care?
Use a child code to capture more detail. ICD Code S31.1 is a non-billable code.
What is inclusion term?
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
Popular Posts:
- 1. icd 9 code for nerve damage
- 2. what is the icd 10 code for contractions at term pregnancy
- 3. icd 10 code for thyroid d/o
- 4. icd-10 code for schizophrenia
- 5. icd 10 code for gastrointestinal upset
- 6. icd 10 code for liver cirrhosis due to alcohol
- 7. icd 10 cm code for rectal burning,
- 8. icd 10 code for abnormal ct with spleen lesions
- 9. icd 10 code for sprain of left hand
- 10. icd 10 code for deaf left ear