Where can one find ICD 10 diagnosis codes?
Search the full ICD-10 catalog by:
- Code
- Code Descriptions
- Clinical Terms or Synonyms
How many codes in ICD 10?
- ICD-10 codes were developed by the World Health Organization (WHO) External file_external .
- ICD-10-CM codes were developed and are maintained by CDC’s National Center for Health Statistics under authorization by the WHO.
- ICD-10-PCS codes External file_external were developed and are maintained by Centers for Medicare and Medicaid Services. ...
What are the common ICD 10 codes?
ICD-10-CM CATEGORY CODE RANGE SPECIFIC CONDITION ICD-10 CODE Diseases of the Circulatory System I00 –I99 Essential hypertension I10 Unspecified atrial fibrillation I48.91 Diseases of the Respiratory System J00 –J99 Acute pharyngitis, NOS J02.9 Acute upper respiratory infection J06._ Acute bronchitis, *,unspecified J20.9 Vasomotor rhinitis J30.0
What is the ICD 10 diagnosis code for?
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.

What is the ICD-10 code for bronchitis not specified as acute or chronic?
ICD-10 code: J40 Bronchitis, not specified as acute or chronic.
What is the ICD-10 code for acute bacterial bronchitis?
ICD-10-CM Code for Acute bronchitis due to other specified organisms J20. 8.
What is the diagnosis for acute bronchitis?
Acute bronchitis is a clinical diagnosis characterized by cough due to acute inflammation of the trachea and large airways without evidence of pneumonia. Pneumonia should be suspected in patients with tachypnea, tachycardia, dyspnea, or lung findings suggestive of pneumonia, and radiography is warranted.
What is the ICD-10 code for acute bronchitis with bronchospasm?
J98. 01 - Acute bronchospasm | ICD-10-CM.
What is acute bacterial bronchitis?
Acute bronchitis is inflammation of the windpipe (trachea) and the airways that branch off the trachea (bronchi) caused by infection. Acute bronchitis is usually caused by a viral upper respiratory tract infection. Symptoms are a cough that may or may not produce mucus (sputum).
What is the diagnosis code for a patient with bronchitis and the flu?
ICD-10-CM Diagnosis Code J20 J20. 1 Acute bronchitis due to Hemophilus influenzae... J20. 5 Acute bronchitis due to respiratory syncytial...
How is bronchitis diagnosed in adults?
Bronchitis Diagnosis Your doctor usually can tell whether you have bronchitis based on a physical exam and your symptoms. They'll ask about your cough, such as how long you've had it and what kind of mucus comes up with it. They'll also listen to your lungs to see whether anything sounds wrong, like wheezing.
What are 3 symptoms of bronchitis?
For either acute bronchitis or chronic bronchitis, signs and symptoms may include:Cough.Production of mucus (sputum), which can be clear, white, yellowish-gray or green in color — rarely, it may be streaked with blood.Fatigue.Shortness of breath.Slight fever and chills.Chest discomfort.
Is acute bronchitis a viral infection?
Usually, acute bronchitis is brought on by a viral infection, though it may also be caused by a bacterial infection. The flu and colds are examples of viral infections. Chronic bronchitis is usually, but not always, caused by smoking tobacco.
Is bronchospasm the same as bronchitis?
Definition. Bronchospasm is an abnormal contraction of the smooth muscle of the bronchi, resulting in an acute narrowing and obstruction of the respiratory airway. A cough with generalized wheezing usually indicates this condition. Bronchospasm is a chief characteristic of asthma and bronchitis.
What is the diagnosis for ICD-10 code r50 9?
9: Fever, unspecified.
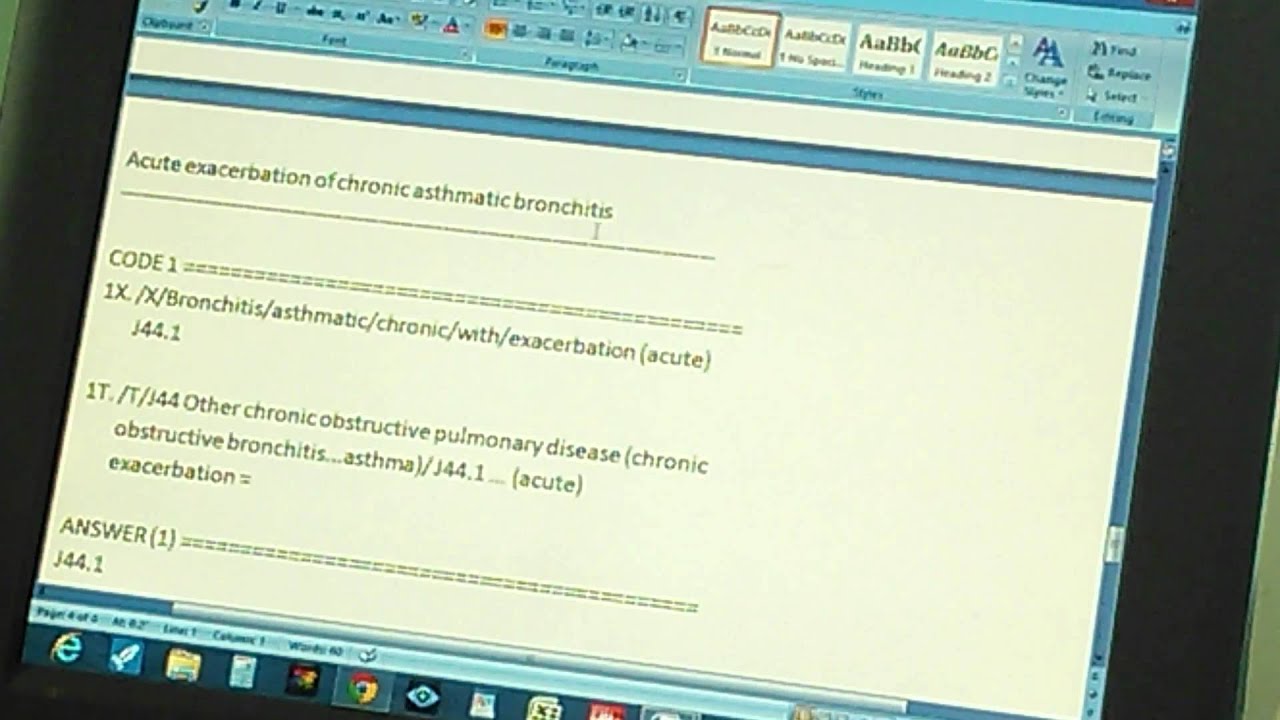
How do you code acute bronchitis with asthma?
ICD-10-CM J45. 901 is grouped within Diagnostic Related Group(s) (MS-DRG v39.0): 202 Bronchitis and asthma with cc/mcc. 203 Bronchitis and asthma without cc/mcc.
What is a type 1 exclude note?
A type 1 excludes note indicates that the code excluded should never be used at the same time as J20. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition. acute bronchitis ( J20.-)
What is J44.0 in pulmonary disease?
chronic obstructive pulmonary disease with acute lower respiratory infection ( J44.0) Other acute lower respiratory infections. Clinical Information. Bronchitis is an inflammation of the bronchial tubes, the airways that carry air to your lungs.
Can a virus cause bronchitis?
The same viruses that cause colds and the flu often cause acute bronchitis. These viruses spread through the air when people cough, or through physical contact (for example, on unwashed hands). Being exposed to tobacco smoke, air pollution, dusts, vapors, and fumes can also cause acute bronchitis.
Do you need antibiotics for bronchitis?
You may need inhaled medicine to open your airways if you are wheezing. You probably do not need antibiotics. They don't work against viruses - the most common cause of acute bronchitis. If your healthcare provider thinks you have a bacterial infection, he or she may prescribe antibiotics.
What is A00-B99?
Chapter 1: Certain Infectious and Parasitic Diseases (A00-B99) g. Coronavirus Infections. Code only a confirmed diagnosis of the 2019 novel coronavirus disease (COVID-19) as documented by the provider, documentation of a positive COVID-19 test result, or a presumptive positive COVID-19 test result.
What is the code for puerperium?
During pregnancy, childbirth or the puerperium, a patient admitted (or presenting for a health care encounter) because of COVID-19 should receive a principal diagnosis code of O98.5- , Other viral diseases complicating pregnancy, childbirth and the puerperium, followed by code U07.1, COVID-19, and the appropriate codes for associated manifestation (s). Codes from Chapter 15 always take sequencing priority
Does confirmation require documentation?
In this context, “confirmation” does not require documentation of the type of test performed; the provider’s documentation that the individual has COVID-19 is sufficient. Presumptive positive COVID-19 test results should be coded as confirmed.
Popular Posts:
- 1. icd 10 diagnosis code for ambulatory dysfunction
- 2. icd-10-pcs code for stapes mobilization, left ear for otosclerotic deafness
- 3. icd 10 code for allergy status
- 4. icd 10 dx code for septic shock
- 5. icd-10 code for lumbar strain
- 6. icd 10 code for dry eye syndrome
- 7. icd code for eucrisa
- 8. icd 10 code for pressure ulcer of upper leg
- 9. icd 10 code for less than 8 weeks gestation of pregnancy
- 10. what is the icd-10 code for hiatal hernia