What is the diagnosis code for depression?
Oct 01, 2021 · Encounter for screening for depression Z13.31 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z13.31 became effective on October 1, 2021. This is the American ICD-10-CM version of Z13.31 - other international ...
What is the ICD 10 code for moderate depression?
Z13.31 is a billable diagnosis code used to specify a medical diagnosis of encounter for screening for depression. The code Z13.31 is valid during the fiscal year 2022 from October 01, 2021 through September 30, 2022 for the submission of HIPAA-covered transactions. The ICD-10-CM code Z13.31 might also be used to specify conditions or terms like depression screening …
What is the ICD 10 diagnosis code for?
Oct 01, 2021 · Encounter for screening for maternal depression Z13.32 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z13.32 became effective on October 1, 2021. This is the American ICD-10-CM version of Z13.32 - other ...
What is the CPT code for a depression screening?
Oct 01, 2021 · 2019 - New Code 2020 2021 2022 Billable/Specific Code POA Exempt. Z13.39 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Encntr screen exam for other mental hlth and behavrl disord.
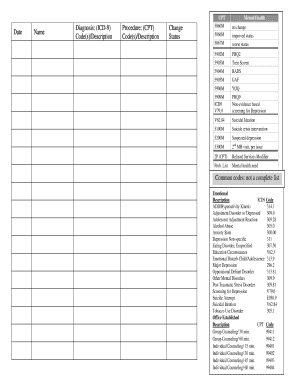
How do you code depression screening?
What is the ICD-10 code for screening?
What diagnosis should be used with G0444?
Can you bill for depression screening?
What is an encounter for screening?
Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.
What is the ICD 10 code for wellness visit?
What is the difference between CPT 96127 and G0444?
What is a annual depression screening?
When should modifier 33 be used?
What is ICD code for depression?
As stated above, F32. 9 describes major depressive disorder, single episode, unspecified.Jun 4, 2021
What is the difference between 96127 and 96160?
What is the CPT code for major depression?
Several codes can be used for reporting acute depression, including 296.2, “Major depressive disorder, single episode,” and 296.3, “Major depressive disorder, recurrent episode.” (Note that both of these codes require a fifth digit.)
What is the code for depression screening?
Code G0444 may be reported for an annual depression screening up to 15 minutes using any standardized instrument (e.g., PHQ-9) in a primary care setting with clinical staff who can advise the physician of screening results and who can facilitate and coordinate referrals to mental health treatment as necessary.
What is the HCPCS level 2 code for depression?
The CMS bulletin for this stated:#N#The provider must have in place staff-assisted depression care supports who can advise the physician of screening results and who can facilitate and coordinate referrals to mental health treatment. HCPCS Level II code is G0444 Annual depression screening, 15 minutes.#N#At a minimum level, staff-assisted depression care supports consist of clinical staff (e.g., nurse, Physician Assistant) in the primary care office who can advise the physician of screening results and who can facilitate and coordinate referrals to mental health treatment.#N#More comprehensive care supports include a case manager working with the primary care physician; planned collaborative care between the primary care provider and mental health clinicians; patient education and support for patient self management; plus attention to patient preferences regarding counseling, medications, and referral to mental health professionals with or without continuing involvement by the patient’s primary care physician.#N#Note: Coverage is limited to screening services and does not include treatment options for depression or any diseases, complications, or chronic conditions resulting from depression, nor does it address therapeutic interventions such as pharmacotherapy, combination therapy (counseling and#N#medications), or other interventions for depression. Self-help materials, telephone calls, and web-based counseling are not separately reimbursable by Medicare and are not part of this NCD.#N#Screening for depression is non-covered when performed more than one time in a 12-month period. Eleven full months must elapse following the month in which the last annual depression screening took place. Medicare coinsurance and Part B deductible are waived for this preventive service.
Can depression screen be billed with IPPE?
Depression Screen#N#G0444 is NOT able to be billed with G0402 (IPPE), but it can be billed with G0438 and G0439 as part of the the annual wellness visit. It cannot be performed with the IPPE, as it is a part of the IPPE and cannot be billed separately. You must perform the PHQ-9 not the PHQ-2 in order to bill the code. What's 7 more questions really? It will be covered and not applied to the patients deductible when performed during the annual wellness visit.
What is the code for depression screening?
For instance, Aetna has a long-standing policy to cover depression screening in primary care when the service is performed using the Patient Health Questionnaire-9 (PHQ-9) tool and is reported with code 96127.
What is the cost of a 96110?
Developmental screening reported with code 96110 is paid for by 45 state Medicaid programs with rates varying from approximately $5 to $60. 1 Many private insurers also provide preventive benefits for code 96110 for developmental screening at nine months, 18 months, and 30 months, and autism screening at 18 months and 24 months in addition to the recommended preventive medicine E/M services (e.g., well-child visits). Developmental surveillance without use of a structured screening instrument is included in the preventive medicine service and not separately reported. Most payers allow two “units” (i.e., instruments) per date of service for code 96110.
Is fee for service for screening and assessment small?
Although the fee-for-service payment for screening and assessments may be small, it can add up to significant income across a patient panel. In addition, most are recommended preventive services, and some may also be factored into performance ratings and quality initiatives.

Popular Posts:
- 1. icd 9 code for rheumatic valvular heart disease
- 2. icd 10 code for molestation
- 3. icd code 10 for tb screening
- 4. icd 10 code for warts on toes
- 5. icd 10 code for kub
- 6. icd 10 code for young male erectile disorder
- 7. what is the icd 10 code for collision with deer
- 8. icd 10 cm code for phlegm
- 9. icd 10 code for c-section incision check
- 10. icd-10-cm code for third-degree burn lower back