Slowness and poor responsiveness
- R46.4 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM R46.4 became effective on October 1, 2021.
- This is the American ICD-10-CM version of R46.4 - other international versions of ICD-10 R46.4 may differ.
What is the ICD 10 code for unresponsive?
Unspecified coma
- Tabular List of Diseases and Injuries. The Tabular List of Diseases and Injuries is a list of ICD-10 codes, organized "head to toe" into chapters and sections with coding notes ...
- Index to Diseases and Injuries. ...
- Approximate Synonyms
- Clinical Information. ...
- Convert R40.20 to ICD-9 Code. ...
What are the common ICD 10 codes?
ICD-10-CM CATEGORY CODE RANGE SPECIFIC CONDITION ICD-10 CODE Diseases of the Circulatory System I00 –I99 Essential hypertension I10 Unspecified atrial fibrillation I48.91 Diseases of the Respiratory System J00 –J99 Acute pharyngitis, NOS J02.9 Acute upper respiratory infection J06._ Acute bronchitis, *,unspecified J20.9 Vasomotor rhinitis J30.0
What is a valid ICD 10 code?
The following 72,752 ICD-10-CM codes are billable/specific and can be used to indicate a diagnosis for reimbursement purposes as there are no codes with a greater level of specificity under each code. Displaying codes 1-100 of 72,752: A00.0 Cholera due to Vibrio cholerae 01, biovar cholerae. A00.1 Cholera due to Vibrio cholerae 01, biovar eltor. A00.9 Cholera, unspecified.
What are the new ICD 10 codes?
The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code XW023X7), and the infusion of other new technology monoclonal antibody (code XW023Y7).
What is ICD-10 for loss of consciousness?
Syncope is in the ICD-10 coding system coded as R55. 9 (syncope and collapse).
What is DX code R46 89?
R46. 89 - Other Symptoms and Signs Involving Appearance and Behavior [Internet]. In: ICD-10-CM.
What is the ICD 10 code for comatose?
ICD-10-CM Code for Coma R40. 2.
What is R41 89?
ICD-10 code R41. 89 for Other symptoms and signs involving cognitive functions and awareness is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is R45 89?
R45. 89 - Other symptoms and signs involving emotional state. ICD-10-CM.
What is the ICD-10 code for stupor?
R40.1ICD-10 code R40. 1 for Stupor is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD-10 code for CVA?
ICD-10 | Cerebral infarction, unspecified (I63. 9)
What is an Obtunded patient?
Obtundation is a state similar to lethargy in which the patient has a lessened interest in the environment, slowed responses to stimulation, and tends to sleep more than normal with drowsiness in between sleep states.
What is the purpose of the ICD-10 code for external cause?
ICD-10 external cause codes provide details explaining the events surrounding an injury, which are especially useful in collecting statistics for policy decisions concerning public health . These ICD-10 codes also play an important role in workers’ compensation claims.
What is the ICd 10?
ICD-10 refers to the tenth edition of the International Classification of Diseases, which is a medical coding system chiefly designed by the World Health Organization (WHO) to catalog health conditions by categories of similar diseases under which more specific conditions are listed, thus mapping nuanced diseases to broader morbidities.
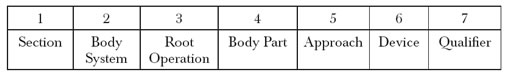
How many characters are in ICd 10?
ICD-10-CM codes consist of three to seven characters. Every code begins with an alpha character, which is indicative of the chapter to which the code is classified. The second and third characters are numbers. The fourth, fifth, sixth, and seventh characters can be numbers or letters.
What does the first 3 characters of an ICD-10 code mean?
The first 3 characters refer to the code category. As such, they represent common traits, a disease or group of related diseases and conditions.
What are the four parts of the ICD-10 index?
This four-part index encompasses the Index of Diseases and Injury, the Index of External Causes of Injury, the Table of Neoplasms, and the Table of Drugs and Chemicals, all of which are designed to streamline the process of locating the necessary diagnosis codes and ICD-10 coding instructions.
What is the ICD-10 code for outpatient?
Sections II – IV Conventions outline rules and principles for the selection of primary diagnoses, reporting additional diagnoses, and diagnostic coding and report ing of outpatient services.
When was the ICd 9 released?
Shortly after the release of ICD-9 in 1979, the US created its own version, known as the International Classification of Diseases, Ninth Revision, Clinical Modification—or, ICD-9-CM. The development of ICD-9-CM was a tremendous boon.
What is the code for sepsis?
Sepsis due to a procedural complication, Infection following a procedure ( T81.4-) or following incomplete spontaneous abortion (O03.37) should be coded first, followed by the specific infection. Remember, there is no code for a diagnosis of “urosepsis”. Newborn sepsis has its own unique code (P36).
What is the coma scale used for?
The coma scale may also be used to assess the status of the central nervous system for other non-trauma conditions. The coma scale codes should be sequenced after the diagnosis code (s). Three codes, one from each subcategory, are needed to complete the scale. The 7th character indicates when the scale was recorded.
Do you need multiple diagnoses?
Frequently multiple diagnoses are required. Very important. And notice the emphasis on diagnoses. The final diagnoses should reflect how difficult the case was, meaning the complexity of all the medical decision making including laboratory tests, EKG’s, x-rays, CT’s and treatment that was medically necessary.
Do you need to list symptoms separately?
For example, a patient who presents with chest pain and is found to have an NSTEMI should be coded as an NSTEMI. There is no need to list the symptom of chest pain as a diagnosis. Answer.
Can an emergency physician code a rule out?
As discussed in FAQ 4, Emergency physicians may not code “rule out” diagnoses, coding guidelines for inconclusive diagnoses (probable, suspected, rule out, etc.) were developed for inpatient reporting and do not apply to outpatients. Answer.
Is ACEP responsible for the Pearls?
ACEP, its committee members, authors or editors assume no responsibility for, and expressly disclaim liability for, damages of any kind arising out of or relating to any use, non-use, interpretation of, or reliance on information contained or not contained in the FAQs and Pearls.
Is chest pain a diagnosis?
There is no need to list the symptom of chest pain as a diagnosis. Answer. The final diagnosis should always be as specific as possible. However, if at the end of an encounter, no clear diagnosis can be established, it is acceptable to code sign (s) and/or symptom (s) instead of a diagnosis.

Popular Posts:
- 1. icd 10 surgery code for ommaya placement
- 2. icd 10 cm code for demyelinating sensorimotor polyneuropathy bilateral
- 3. icd 9 code for mental illness
- 4. icd 9 code for hepatic cyst
- 5. icd 10 code for congenital rubella pneumonitis
- 6. icd-10 code for s/p stress fracture
- 7. icd 10 code for swelling right 5th finger
- 8. icd 10 code for female infertility
- 9. icd 10 code for history of 3rd degree burn
- 10. icd 10 code for status post right knee replacement