96360, Intravenous infusion, hydration; initial, 31 minutes to 1 hour, and 96361, Intravenous infusion, hydration; each additional hour. The purpose of hydration intravenous (IV) infusion is to hydrate. These codes were
What is the ICD 10 code for dehydration?
Oct 01, 2015 · Introduction of Insulin into Peripheral Artery, Percutaneous Approach. 2016 2017 2018 2019 2020 2021 2022 Billable/Specific Code. ICD-10-PCS 3E053VG is a specific/billable code that can be used to indicate a procedure. Code History. 2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-PCS) 2017 (effective 10/1/2016): No change.
What is ICD-10-PCS (procedure codes)?
Jul 11, 2019 · The following ICD-10 codes have undergone a descriptor change for Group 1 Codes: D57.411, D57.412, and D57.419. Minor formatting has been made throughout the coding section. 07/19/2019 R1 LCD revisied and published on 10/17/2019 effecive for dates of service on or after 07/19/2019 to add ICD-10-CM codes D57.00, D57.01, D57.02, D57.211, D57.212, …
What is the ICD 10 code for anhydremia?
Oct 01, 2015 · 2022 ICD-10-PCS Procedure Code 3E043GQ; 2022 ICD-10-PCS Procedure Code 3E043GQ Introduction of Glucarpidase into Central Vein, Percutaneous Approach. 2016 2017 2018 2019 2020 2021 2022 Billable/Specific Code. ICD-10-PCS 3E043GQ is a specific/billable code that can be used to indicate a procedure.
What is the ICD 10 code for peripheral arterial insulin injection?
ICD-10-CM Diagnosis Code E74.09 [convert to ICD-9-CM] Other glycogen storage disease. Glycogen storage disease type viii; Glycogen storage disease, type 4; Glycogen storage disease, type 6; Glycogen storage disease, type 7; Glycogen storage disease, type 8; Glycogen storage disease, type 9; Glycogen storage disease, type iv; Glycogen storage disease, type ix; Glycogen …

How do you code ICD-10-PCS?
1:551:30:47Introduction to ICD-10-PCS Coding for Beginners Part I - YouTubeYouTubeStart of suggested clipEnd of suggested clipWell now they have a health information systems him system and they in 1995 was contracted by centerMoreWell now they have a health information systems him system and they in 1995 was contracted by center for medicare medicaid services to develop pcs yes to design.
What is the ICD-10 code for IV antibiotics?
Long term (current) use of antibiotics Z79. 2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD-10 code for medication management?
GZ3ZZZZICD-10-PCS GZ3ZZZZ is a specific/billable code that can be used to indicate a procedure.
What is the ICD-10-PCS code for IVIG?
30233S1Transfusion of Nonautologous Globulin into Peripheral Vein, Percutaneous Approach. ICD-10-PCS 30233S1 is a specific/billable code that can be used to indicate a procedure.
What is diagnosis code Z51 81?
2022 ICD-10-CM Diagnosis Code Z51. 81: Encounter for therapeutic drug level monitoring.
What is an IV antibiotic?
Intravenous antibiotics are antibiotics that are administered directly into a vein so that they can enter the bloodstream immediately and bypass the absorption in the gut. It is estimated that more than 250,000 patients in the US receive outpatient IV antibiotics to treat bacterial infections.Mar 17, 2021
What is Z71 89 ICD-10?
Other specified counselingICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
How do you code for medication management?
The primary billing codes used are:90862 – Defined as pharmacological management including prescription use and review of medication with no more than minimal psychotherapy.90805 – Individual psychotherapy approximately 20 – 30 minutes face to face, with medical evaluation and management services.More items...•Jan 24, 2019
Can Z71 89 be used as a primary diagnosis?
The code Z71. 89 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
What does IVIG stand for in medical terms?
Intravenous immune globulin ("IVIG") is a product made up of antibodies that can be given intravenously (through a vein). Antibodies are proteins that your body makes to help you fight infections.Feb 25, 2021
Does Medicare cover j1561?
Medicare will provide coverage for intravenous immune globulin when it is used in treatment of the following conditions: Primary immunodeficiency....CPT Jcode – J0850, J1459, J1561, J1568, J2788 – Intravenous Immune Globulin (IVIG)042*Human Immunodeficiency Virus (HIV) disease078.5Cytomegaloviral disease35 more rows
Is immunoglobulin A blood product?
Intravenous immunoglobulin (IVIG) is a blood product prepared from the serum of between 1000 and 15 000 donors per batch. It is the treatment of choice for patients with antibody deficiencies.Apr 14, 2005
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L34960, Hydration Therapy. Please refer to the LCD for reasonable and necessary requirements.
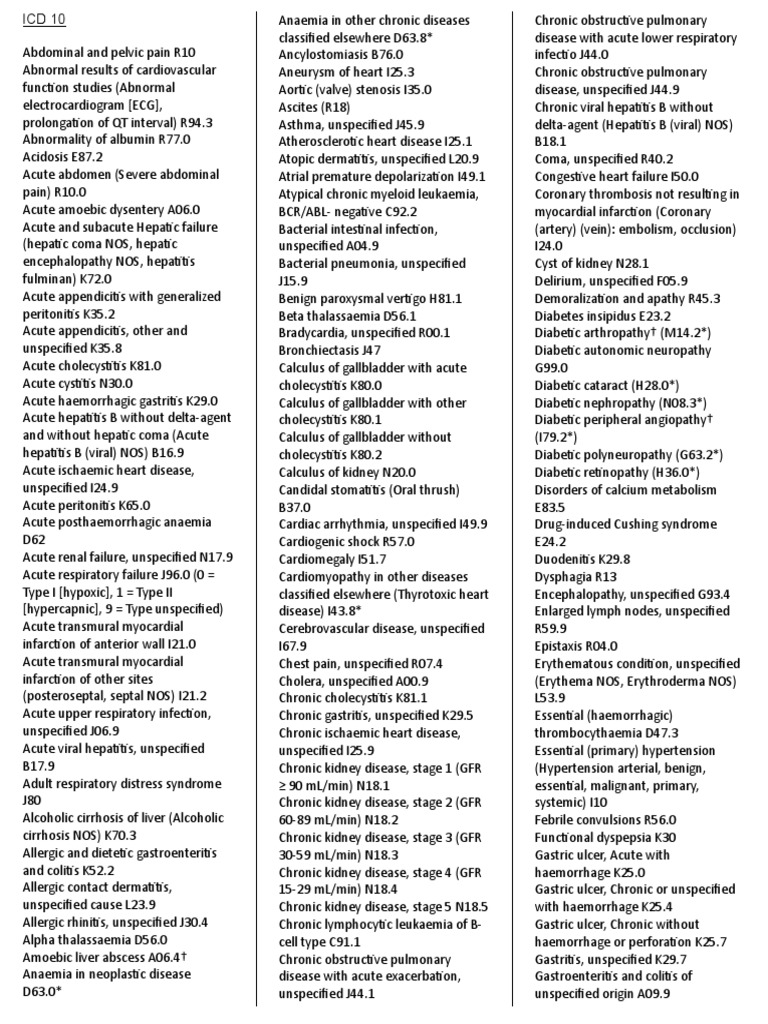
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted. The following ICD-10-CM codes support medical necessity and provide coverage for CPT/HCPCS codes 96360, 96361, J7030, J7040, J7042, J7050, J7060, J7070, J7120 and J7121:.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is the code for extracorporeal therapy?
6 - Extracorporeal or Systemic Therapies. In extracorporeal therapy, equipment outside the body is used for a therapeutic purpose that does not involve the assistance or performance of a physiological function. Extracorporeal therapy procedure codes have a first character value of “6”.
What is section code 3?
3 - Administration. Administration section codes represent procedures for putting in or on a therapeutic, prophylactic, protective, diagnostic, nutritional or physiological substance. Administration procedure codes have a first character value of “3”.
What is the first character value of extracorporeal assistance and performance procedure codes?
Extracorporeal assistance and performance procedure codes have a first character value of “5”. The second character value for body system is physiological systems.
What is nuclear medicine?
Nuclear medicine section codes represent procedures that introduce radioactive material into the body in order to create an image, to diagnose and treat pathologic conditions, or to assess metabolic functions. The nuclear medicine section does not include the introduction of encapsulated radioactive material for the treatment of cancer. These procedures are included in the radiation oncology section. Nuclear medicine procedure codes have a first character value of “C”. The second character specifies the body system on which the nuclear medicine procedure is performed. The third character root type indicates the type of nuclear medicine procedure (e.g., planar imaging or non-imaging uptake).
What is the first character value of a measurement and monitoring procedure code?
Measurement and monitoring procedure codes have a first character value of “4”. The second character value for body system is either physiological systems or physiological devices.
What is a placement section code?
Placement section codes represent procedures for putting an externally placed device in or on a body region for the purpose of protection, immobilization, stretching, compression or packing. Placement procedure codes have a first character value of “2”.
What is the medical section code?
The Medical and Surgical section codes represent the vast majority of procedures reported in an inpatient setting. Medical and surgical procedure codes have a first character value of "0". The 2nd character indicates the general body system (e.g., gastrointestinal). The first through fifth characters are always assigned a specific value, ...
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
Palmetto GBA has received inquiries related to the billing and documentation of infusions, injections and hydration fluids. Documentation, medical necessity, and code assignment are very important.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Popular Posts:
- 1. what is the correct icd 10 code for otois media
- 2. icd 10 code for traumatic arthrotomy right knee
- 3. icd 9 code for personal history of gunshot wound
- 4. icd 10 code for mass of the forehead
- 5. icd 10 code for right scleral abrasion
- 6. icd 9 code for abdominal mass
- 7. icd-9 code for 272.2
- 8. icd 10 code for hairy cell leukemia
- 9. icd-10 code for inability to ejaculate
- 10. icd 10 code for cervical ddd