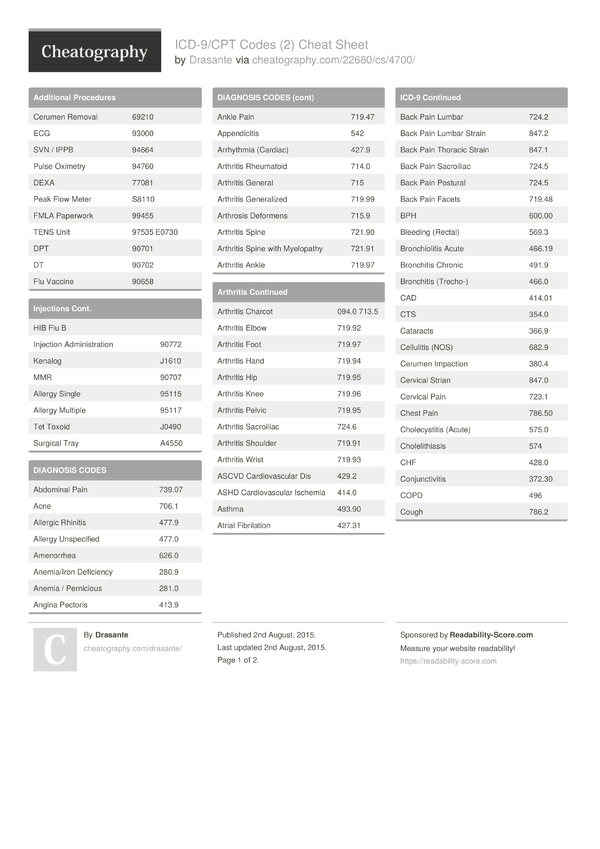
| Psychotherapy Codes | |
|---|---|
| CPT® Code | Descriptor |
| 90832 | Psychotherapy, 30 minutes with patient |
| 90834 | Psychotherapy, 45 minutes with patient |
| 90837 | Psychotherapy, 60 minutes with patient |
When to use the 90837 CPT code?
While some therapists are inclined to use the 90837 for any session over 45 minutes, the AMA has defined these codes using standard rounding practices, rounding down to the 90834 for a 52 minute session, and rounding up to a 90837 for a 53 minute session.
What does CPT code 90837 stand for?
What does CPT code 90837 mean? Both 90834 and 90837 are designed to bill for the same service – psychotherapy. The primary distinguishing factor between the two codes is time; 90834 is defined as 45 minutes of psychotherapy, while 90837 is defined as 60 minutes. Likewise, who can bill CPT code 90837? Individual therapy codes (90832-90837 ...
How do I look up diagnosis codes?
- Enter one or more ICD-10 codes along with other required inputs
- Click a button
- Get the resulting DRG and other important information (including the Relative Weight, Length of Stay, Procedure Type, Post-Acute Indication and other items)
What is Procedure Code 90837?
What is procedure code 90837? CPT Code 90837 is a procedure code that describes a 60 minute individual psychotherapy session performed by a licensed mental health provider. 90837 is considered a routine outpatient CPT Code and is one of the most common CPT codes used in mental health insurance claims coding and billing.
Can you bill 90837?
Both 90834 and 90837 are designed to bill for the same service – psychotherapy. The primary distinguishing factor between the two codes is time; 90834 is defined as 45 minutes of psychotherapy, while 90837 is defined as 60 minutes.
Is 90837 an add-on code?
Since it is an add-on code it must be billed with 90837 or 90847 (90791 and 90834 are not allowed). Services performed outside of business hours.
What is the CPT code for a 60 minute psychotherapy session?
9083790837 – Psychotherapy 60 minutes.
What is code 90837 used for?
CPT® code 90837: Psychotherapy, 1 | American Medical Association.
How do you code a 90 minute psychotherapy session?
Units vs Extended Session CPT Codes Rather, what is required to bill for 90 minutes is an add-on code on a new line in box 24 of your CMS1500 form. To bill an insurance claim for a 90 minute individual therapy session: bill 90837. with add-on code 99354.
How do you bill for a 2 hour therapy session?
You'll want to use your typical 90837 CPT code. Then you'll also want to use the Add On CPT code 99354 which declares an additional 30 to 74 minutes of therapy. So any time you do 90 to 2 hours and 14 minutes of therapy, make sure to use the combination of CPT Codes 90837 and +99354.
Is 90837 a timed code?
The Background Of The 90837 Each of these codes are timed and are well-known to many therapists, as they represent the majority of regularly billed codes, which are the 90832, 90834, and 90837. These, respectively, are described as providing individual psychotherapy for 30 minutes, 45 minutes, or 60 minutes.
Does CPT code 90837 require a modifier?
For Medicare, you can bill the traditional psychotherapy codes: 90832 (30 minutes); 90834 (45 minutes); and 90837 (60 minutes). You will also need to include the 95 modifier when submitting your bill.
How many times can you bill 90837?
CPT code 90837 is another one of the most common CPT codes used by mental health professionals along with 90834 and 90791. Its typical use is for a normal psychotherapy session with a client. Insurers will reimburse this code only once per day, and some only as frequently as twice per week.
What is the Medicare rate for 90837?
$132.69What is the difference between the “facility rate” and “nonfacility rate” for telehealth services?CodeService2021 Facility Rate90832Psychotherapy 30-minutes$68.7490837Psychotherapy 60-minutes$132.6996132Neuropsych Test Eval$106.0896158Hlth Bhvr Intrv Indvl$58.971 more row•Dec 10, 2021
What is the CPT code for telehealth psychotherapy?
Although Medicare reimburses for audio and video telehealth, audio-only reimbursement is currently covered only during the COVID-19 public health emergency....Audio-only or video telehealth.CategoryTeleheath CPT codes and HCPCS codesPsychotherapy90832, 90833, 90834, 90836, 90837, 90838Psychoanalysis9084523 more rows•May 4, 2022
Can I use 90837 for couples therapy?
You should use codes 90832, 90834 or 90837 for the IP. Doing so follows the protocol for an individual therapy session without guests. The CPT code 90846 is for family and couples therapy without your IP present.
How long is 90837 CPT?
The limitation of psychotherapy codes to only three codes with a cap at 60 minutes encapsulates the problem facing therapists today when coding their claims; the AMA defines these CPT codes based on the length of session, with the 90837 being used for any session over 53 minutes, with no way to account for sessions longer than an hour, which frequently can occur when conducting psychotherapy.
How long is a 90837 session?
While some therapists are inclined to use the 90837 for any session over 45 minutes, the AMA has defined these codes using standard rounding practices, rounding down to the 90834 for a 52 minute session, and rounding up to a 90837 for a 53 minute session.
What is a CPT code?
CPT Codes, or Current Procedural Terminology codes, are the procedure codes used for classifying medical services, and this code set is maintained by the AMA. CPT codes are used to describe all kinds of tests, surgeries, evaluations, and other medical procedures performed by healthcare providers, and number in the tens of thousands.
How many characters are CPT codes?
CPT codes are always 5 characters in length and describe the type of service provided, whereas the diagnosis describes the medical issues or diagnosis.
What is the billing code for therapy?
Many therapists have weekly or bi-weekly sessions with clients and are faced with scrutiny and uncertainty when utilizing the 90837 billing code.
What is the code for behavioral health?
While most procedure codes behavioral health providers utilize are numeric and in the 90000 series (e.g. 90834), it is also common to see codes beginning with an H, Q, or T , followed by four digits.
How many codes are there for psychotherapy?
Under the new protocols, there were only three codes available for individual psychotherapy. Each of these codes are timed and are well-known to many therapists, as they represent the majority of regularly billed codes, which are the 90832, 90834, and 90837. These, respectively, are described as providing individual psychotherapy for 30 minutes, ...
Overview
The clinical examples and their procedural descriptions, which reflect typical clinical situations found in the health care setting, are included in this text with many of the codes to provide practical situations for which the codes would be appropriately reported.
Typical patient description
An adult undergoes psychotherapy due to anxiety and depressive symptoms. Psychosocial stressors at work and home have increased anxiety and depression since a recent hospital discharge.
Care components
During the visit, face-to-face therapeutic communication is conducted with the patient and/or the patient's family. Objective information and an interval history are obtained.
About the CPT code set
Medical knowledge and science are constantly advancing, so the CPT Editorial Panel manages an extensive process to make sure the CPT code set advances with it.
What is CPT code 90837?
• Code 90837: Psychotherapy, 60 minutes with patient and/or family member In general, providers should select the code that most closely matches the actual time spentperforming psychotherapy . CPT® provides flexibility by identifying time ranges that may be associated with each of the three codes:
Is a psychotherapy code dependent on the location?
Psychotherapy codes are no longer dependent on the service location (i.e., office, hospital, residential setting, or other location is not a factor). However, effective January 1, 2014, when E&M services are paid under Medicare’s Partial Hospitalization Program (PHP) and not in the physician office setting, the CPT outpatient visit codes ...
What is the code for prolonged therapy?
For psychotherapy sessions lasting 90 minutes or longer, the appropriate prolonged service code should be used (99354-99357). The duration of a course of psychotherapy must be individualized for each patient. Prolonged treatment may be subject to medical necessity review.
What is the procedure code for psychoanalysis?
Description: Procedure code 90845 involves the practice of psychoanalysis using special techniques to gain insight into and treat a patient’s unconscious motivations and conflicts using the development and resolution of a therapeutic transference to achieve therapeutic effect. It is a different therapeutic modality than psychotherapy.
When should a psychotherapy code not be billed?
A psychotherapy code should not be billed when the service is not primarily a psychotherapy service, that is, when the service could be more accurately described by an evaluation and management or other code. The duration of a course of psychotherapy must be individualized for each patient.
How long is 90837?
The one being addressed in this blog, is 90837, which is 53 minutes or more.
Why is 90837 necessary?
your client may have a trauma history: “90837 is medically necessary because significant trauma hx necessitates taking time to create safe space for disclosure and then containment. ”. Or: “90837 is medically necessary to address complicated diagnosis and clinical presentation.”.
How much more is 90834 than the insurance company?
Though it is not allowed to give the actual amount of payment by an insurance company because doing so violates the Sherman Antitrust Law, it is safe to say that payment is up to $30 more than what is paid for 90834. Not billing for the time you spend leaves a lot of money on the table.
When were CPT codes revised for psychotherapy?
When CPT codes for psychotherapy were revised in 2017, it became possible to bill for longer therapy sessions. The one being addressed in this blog, is 90837, 53 minutes or more. June 23, 2019 by Beth Rontal 13 Comments.
Can you bill for 90834?
Theoretically, yes. But practically, no. The CPT code is based on face-to-face time, meaning you can only bill for the time actually spent with the client. If the client is late, you need to bill at 90834 (38 – 52 minutes). Otherwise, you risk insurance fraud.
Can you use 90837 for convenience?
According to BCBS, using 90837 “cannot be for the convenience of the provider.”. This means, though specific documentation is not required, play it safe by including justification on your progress note. For example, let’s say:
Does BCBS honor 90837?
Insurance companies have been reluctant to pay for 90837 and slow to get on board so it is best to check with the company. But BCBS does honor this code and so do many other insurance companies. According to Care Paths, the denial rate for BCBS in 2017 was 1.29%, which is a down from 3 to 4% in 2013 and 2015.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L33252 Psychiatric Diagnostic Evaluation and Psychotherapy Services.
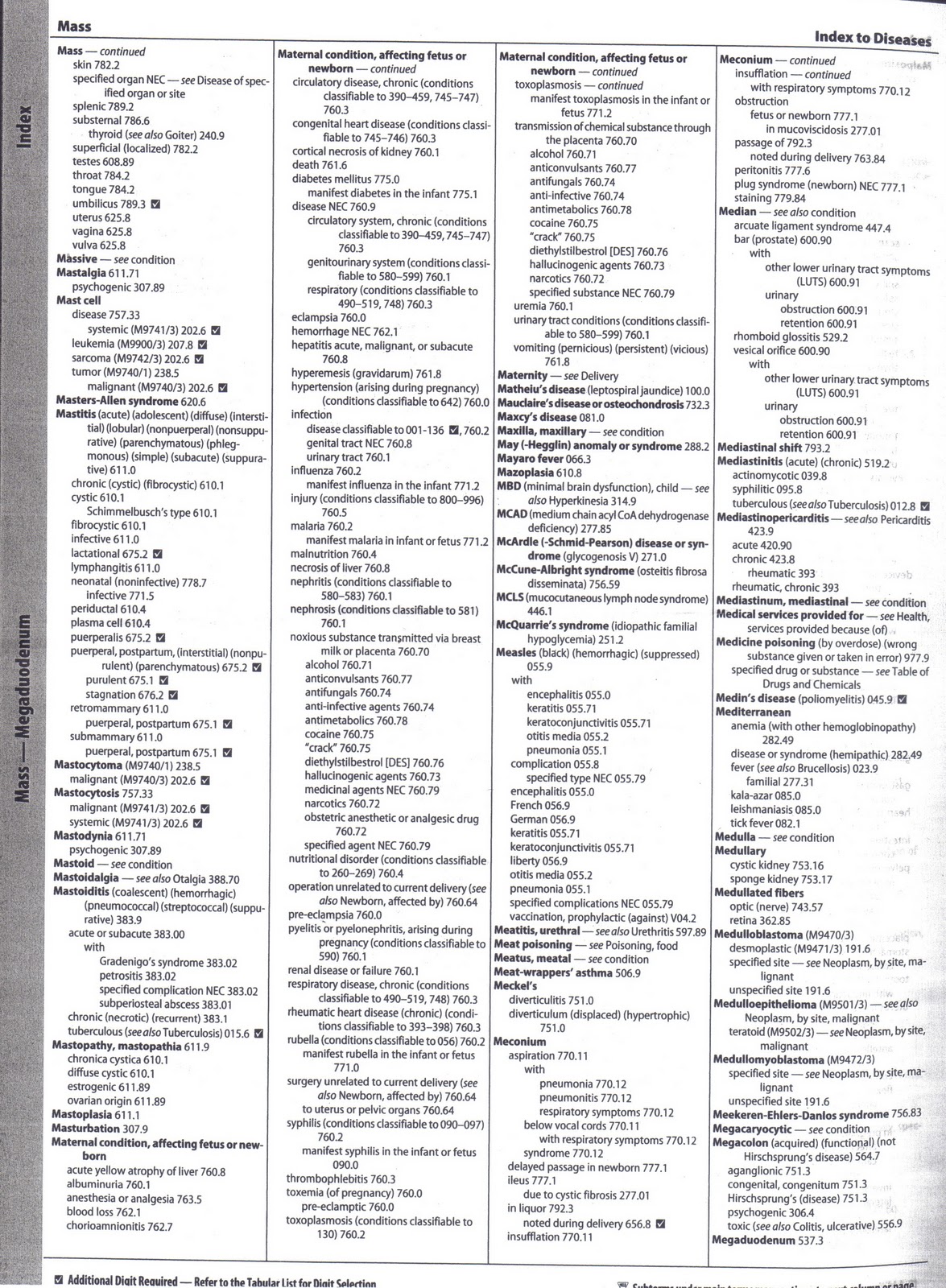
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
This LCD supplements but does not replace, modify or supersede existing Medicare applicable National Coverage Determinations (NCDs) or payment policy rules and regulations for psychiatric codes. Federal statute and subsequent Medicare regulations regarding provision and payment for medical services are lengthy. They are not repeated in this LCD.
Coverage Guidance
Compliance with the provisions in this policy may be monitored and addressed through post payment data analysis and subsequent medical review audits. History/Background and/or General Information This LCD provides guidelines for many psychiatric services. However, this LCD does not address all services, including BUT NOT LIMITED TO:
Popular Posts:
- 1. icd 10 code for fetal heart check
- 2. principal icd-10-cm code for iron deficiency anemia secondary to blood loss → poa yes
- 3. icd 10 code for cellulitis of left lower extremity
- 4. icd 10 code for personal history of esophageal stricture
- 5. icd 1o code for dm 2
- 6. icd 10 code for joint pain\
- 7. icd 10 code for history of recurrent spontaneous abortion
- 8. icd 10 code for hx of prostatectomy
- 9. icd 10 code for respiratory distress escalated to respiratory failure
- 10. icd 10 code for breast cancer right