What is the ICD 10 code for bronchiolitis?
Bronchiolitis (acute) (infective) (subacute) J21.9. ICD-10-CM Diagnosis Code J68.0 ICD-10-CM Diagnosis Code J44.9 ICD-10-CM Diagnosis Code J21.1 ICD-10-CM Diagnosis Code J21.0 ICD-10-CM Diagnosis Code J21.8 ICD-10-CM Diagnosis Code J44.9 ICD-10-CM Diagnosis Code J84.89 ICD-10-CM Diagnosis Code J44.9...
What are the symptoms of bronchiolitis obliterans?
Bronchiolitis obliterans. Bronchiolitis obliterans (BO), also known as obliterative bronchiolitis, popcorn lung, and constrictive bronchiolitis, is a disease that results in obstruction of the smallest airways of the lungs (bronchioles) due to inflammation. Symptoms include a dry cough, shortness of breath, wheezing and feeling tired.
What is the abbreviation for bronchiolitis obliterans?
Bronchiolitis obliterans. Bronchiolitis obliterans (BO), also known as obliterative bronchiolitis and popcorn lung, is a disease that results in obstruction of the smallest airways of the lungs (bronchioles) due to inflammation.
Do I need a lung biopsy for bronchiolitis obliterans?
If the diagnosis is still unclear, a lung biopsy may be necessary. Bronchiolitis obliterans is an irreversible and chronic condition, with available treatments that can slow progression and reduce the severity of your symptoms.
What is the ICD 10 code for bronchiolitis obliterans syndrome?
J84. 115 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM J84. 115 became effective on October 1, 2021.
What is the icd9 code for COPD?
COPD not elsewhere classified (ICD-9-CM code 496) is a nonspecific code that should only be used when the documentation in the medical record does not specify the type of COPD being treated. A diagnosis of COPD and acute bronchitis is classified to code 491.22.
What is the ICD 10 code for acute bronchitis?
9 – Acute Bronchitis, Unspecified. Code J20. 9 is the diagnosis code used for Acute Bronchitis, Unspecified.
How do you code chronic bronchitis and COPD?
909 - Asthma NOS and J44. 1 - COPD with (acute) exacerbation. If the COPD exacerbation is in the setting of COPD with acute bronchitis, both code J44.
What is the ICD 10 code for COPD exacerbation?
1: Chronic obstructive pulmonary disease with acute exacerbation, unspecified.
What is diagnosis code R91 8?
Other nonspecific abnormal finding of lung fieldICD-10 code R91. 8 for Other nonspecific abnormal finding of lung field is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is R53 83?
ICD-9 Code Transition: 780.79 Code R53. 83 is the diagnosis code used for Other Fatigue. It is a condition marked by drowsiness and an unusual lack of energy and mental alertness. It can be caused by many things, including illness, injury, or drugs.
What is J20 9 an example of?
Acute bronchitis, unspecified9 Acute bronchitis, unspecified.
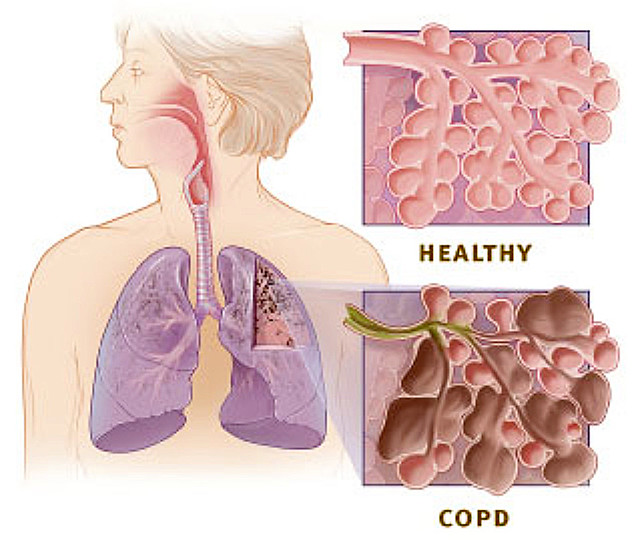
What is COPD unspecified?
Chronic obstructive pulmonary disease, or COPD, refers to a group of diseases that cause airflow blockage and breathing-related problems. It includes emphysema and chronic bronchitis. COPD makes breathing difficult for the 16 million Americans who have this disease.
What is the ICD-10 code for COPD with asthma?
J44. 9, Chronic obstructive pulmonary disease, unspecified and J45. 40, Moderate persistent asthma, uncomplicated. Codes will be dependent upon the specificity of the COPD and asthma documented.
What is the ICD-10 code for end stage COPD?
ICD 10 Coding Patient has COPD with emphysema •J43. 9, Emphysema, unspecified - Note: There is an exclusion note under J44* (COPD) for emphysema without chronic bronchitis.
What is the ICD-9 code for asthma?
The ICD-CM codes for asthma have changed from 493.00 – 493.99 in ICD-9-CM to J45.
What is the name of the condition where the lungs are compressed and narrowed?
ALTERNATE NAMES. Bronchiolitis Obliterans; Constrictive Bronchiolitis. DESCRIPTION. Obliterative Bronchiolitis (OB) is a rare, irreversible, life-threatening form of lung disease that occurs when the small airway branches of the lungs (bronchioles) are compressed and narrowed by scar tissue (fibrosis) and inflammation.
What test is used to determine if you have OB?
Diagnostic testing: Although a definitive diagnosis of OB requires can only made by a lung biopsy, other diagnostic tests which aid in the diagnosis include:
Is OB the same as COP?
Symptoms of OB include coughing (usually without phlegm), shortness of breath on exertion, wheezing and fatigue, OB is not the same disorder as bronchiolitis obliterans organizing pneumonia (BOOP), now known as cryptogenic organizing pneumonia (COP), which is a treatable disorder with a favorable prognosis.
How to diagnose bronchiolitis obliterans?
Several tests are often needed to diagnose bronchiolitis obliterans, including spirometry, diffusing capacity of the lung tests ( DLCO ), lung volume tests, chest X-rays, high-resolution CT (HRCT), and lung biopsy .
What is bronchiolitis obliterans syndrome?
The disease is often termed bronchiolitis obliterans syndrome (BOS) in the setting of post lung transplantation and hematopoietic stem cell transplant (HSCT). Patients who develop BOS post lung transplant vary in disease latency and severity. Patients often initially have normal lung function on pulmonary function testing and have normal chest radiographs. As the disease progresses they begin to have symptoms of shortness of breath, cough, and wheezing as their lung function declines. The Journal of Heart and Lung Transplantation published updated guidelines in 2001 for grading the severity of BOS. The original guidelines and classification system were published in 1993 by the International Society for Heart and Lung Transplantation. Their scoring system is based on the changes in FEV 1 in patients from their baseline. When patients are first diagnosed with BOS they have their baseline lung function established by doing pulmonary function testing at the time of diagnosis. The BOS scoring system is as follows:
What are the risk factors for obliterative bronchiolitis?
Other risk factors post transplant including tobacco use, age of donor, age of recipient, lower baseline FEV1/FVC ratio, non-caucasian race, peripheral and lower circulating IgG levels. Studies have, however, shown mixed results regarding these other risk factors. There has been an association shown between the increased use of peripheral stem cells and the risk of developing obliterative bronchiolitis. Also, research has shown an increased risk for developing the disease within the first year of transplant if the person is infected with respiratory syncytial virus or parainfluenza virus within the first 100 days post transplant.
What is constrictive bronchiolitis?
A form of constrictive bronchiolitis is starting to present in Iraq and Afghanistan veterans. It has been attributed to veterans being exposed to trash burn pits . Veterans present with shortness of breath and other asthma-like symptoms. The only way to diagnose this condition is by doing a lung biopsy as chest X-rays and CT scans come back as normal. The government still denies that there is any correlation between burn pits and health problems but the government has started an "Airborne Hazards and Open Burn Pit Registry" to begin tracking the health of veterans who were exposed to burn pits to see if there is a connection.
How long does it take to die from bronchiolitis?
Outcomes are often poor, with most people dying in months to years. Obliterative bronchiolitis is rare in the general population. It, however, affects about 75% of people by ten years following a lung transplant and up to 10% of people who have received a bone marrow transplant from someone else.
Where is bronchiolitis most common?
Post-infectious obliterative bronchiolitis is most common in the southern hemisphere particularly in countries such as Brazil, Argentina, Australia, Chile and New Zealand. There was a large prevalence of the disease in these areas during the 1990s and early 2000s.
Can bronchiolitis cause shortness of breath?
Obliterative bronchiolitis results in worsening shortness of breath, wheezing, and a dry cough. The symptoms can start gradually, or severe symptoms can occur suddenly. These symptoms represent an obstructive pattern that is non-reversible with bronchodilator therapy, and need to be related to various lung insults.

Overview
Bronchiolitis obliterans (BO), also known as obliterative bronchiolitis, constrictive bronchiolitis and popcorn lung, is a disease that results in obstruction of the smallest airways of the lungs (bronchioles) due to inflammation. Symptoms include a dry cough, shortness of breath, wheezing and feeling tired. These symptoms generally get worse over weeks to months. It is …
Signs and symptoms
Bronchiolitis obliterans results in worsening shortness of breath, wheezing, and a dry cough. The symptoms can start gradually, or severe symptoms can occur suddenly. These symptoms represent an obstructive pattern that is non-reversible with bronchodilator therapy, and need to be related to various lung insults. These insults include inhalation damage, post transplant auto-immune injury, post-infectious disease, drug reactions, and several auto-immune diseases.
Cause
Bronchiolitis obliterans has many possible causes, including collagen vascular disease, transplant rejection in organ transplant patients, viral infection (adenovirus, respiratory syncytial virus, influenza, HIV, cytomegalovirus), Stevens–Johnson syndrome, Pneumocystis pneumonia, drug reaction, aspiration and complications of prematurity (bronchopulmonary dysplasia), an…
Mechanism
The underlying mechanism involves injury and inflammation of epithelial and sub-epithelial cells. These cells then lose the ability to repair the tissue, in particular they lose the ability to regenerate the epithelial or outermost layer, leading to the excess growth of cells that cause scarring. There are multiple pathways of the disease including fibrotic, lymphocytic, and antibody-mediated that have been described. However, while each pathway has a more unique starting point and cause, …
Diagnosis
Bronchiolitis obliterans is often diagnosed based on the symptoms of obstructive lung disease following lung injury. The definitive diagnosis is through biopsy, but due to the variable distribution of lesions, leading to falsely negative tests, and invasive nature of this procedure it is often not performed. Several tests are often needed to diagnose bronchiolitis obliterans, including s…
Prevention
Disease caused by exposure to industrial inhalants and burn pits can be prevented with the use of engineering controls (e.g., exhaust hoods or closed systems), personal protective equipment, monitoring of potentially affected personnel, worker education and training.
The primary prevention of bronchiolitis obliterans in people who have received either lung transplant or HSCT therapy is immunosuppression. In regards to post lung transplantation, the c…
Treatment
While the disease is not reversible, treatments can slow further worsening. This may include the use of corticosteroids or immunosuppressive medication which may have an effect on the ability to receive a lung transplant if offered. If patients have difficulty breathing (hypoxemia) oxygen can be supplemented. Routine vaccinations are recommended for patients with chronic lung disease to prevent complications from secondary infections due to pneumonia and influenza.
Terminology
"Bronchiolitis obliterans" was originally a term used by pathologists to describe two patterns of airway disease, the other was bronchiolitis obliterans organizing pneumonia (BOOP), now known as cryptogenic organizing pneumonia. The name cryptogenic bronchiolitis obliterans is used when a cause is unknown.
Bronchiolitis obliterans when it occurs following a lung transplant is known as bronchiolitis oblit…
Popular Posts:
- 1. icd 10 code for mild esophagitis with stenosis
- 2. icd 10 code for lada
- 3. icd 10 code for meckel's diverticulum
- 4. icd-10 code for abnormal stress test
- 5. icd 10 code for cervical or vaginal cancer screening
- 6. icd 10 code for tinea unguium
- 7. icd 10 code for a15.0
- 8. icd 10 code for too many periods
- 9. icd 10 cm code for arteriosclerosis of autologous vein bypass graft
- 10. icd 10 procedure code for insertion of intraluminal device into inferior vena cava endoscopic