What is the ICD 9 code for diagnosis?
ICD-9-CM 275.49 is a billable medical code that can be used to indicate a diagnosis on a reimbursement claim, however, 275.49 should only be used for claims with a date of service on or before September 30, 2015.
What is the ICD 9 code for calcium metabolism?
ICD-9-CM Diagnosis Code 275.49 : Other disorders of calcium metabolism. Home > 2015 ICD-9-CM Diagnosis Codes > Endocrine, Nutritional And Metabolic Diseases, And Immunity Disorders 240-279 > Other Metabolic Disorders And Immunity Disorders 270-279 > Disorders of mineral metabolism 275-.
What is calcium deficiency?
A disorder characterized by laboratory test results that indicate a low concentration of calcium in the blood. Lower than normal levels of calcium in the circulating blood. Reduction of the blood calcium below normal.
Is calcium scoring covered by Medicare?
Quantitative calcium scoring is not a covered service and will be denied as not medically necessary. Calcium scoring reported in isolation is considered a screening service. When performed in association with CT angiography, there is neither separate nor additional included reimbursement for the calcium scoring.
What is the ICD-10 code for calcium?
E58 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM E58 became effective on October 1, 2021. This is the American ICD-10-CM version of E58 - other international versions of ICD-10 E58 may differ.
What is the ICD-9 code?
International Classification of Diseases,Ninth Revision (ICD-9) The International Classification of Diseases (ICD) is designed to promote international comparability in the collection, processing, classification, and presentation of mortality statistics.
What is an ICD-9 or 10 code?
ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started.
What are ICD-9 10 and CPT codes?
In a concise statement, ICD-9 is the code used to describe the condition or disease being treated, also known as the diagnosis. CPT is the code used to describe the treatment and diagnostic services provided for that diagnosis.
Where can I find ICD-9 codes?
ICD9Data.com takes the current ICD-9-CM and HCPCS medical billing codes and adds 5.3+ million links between them. Combine that with a Google-powered search engine, drill-down navigation system and instant coding notes and it's easier than ever to quickly find the medical coding information you need.
Are ICD-9 codes still used?
Currently, the U.S. is the only industrialized nation still utilizing ICD-9-CM codes for morbidity data, though we have already transitioned to ICD-10 for mortality.
How many ICD-9 codes are there?
13,000 codesThe current ICD-9-CM system consists of ∼13,000 codes and is running out of numbers.
What are two difference between ICD-10 and ICD-9 coding?
ICD-9 uses mostly numeric codes with only occasional E and V alphanumeric codes. Plus, only three-, four- and five-digit codes are valid. ICD-10 uses entirely alphanumeric codes and has valid codes of up to seven digits.
Why is ICD-10 better than ICD-9?
ICD-10 uses alphabet codes to be more specific than ICD-9 codes. The additional characters in ICD-10 will allow for more detailed information such as listing the body part, body system, device, approach, and other important qualifiers in a single code.
What is diagnosis code R53 83?
Code R53. 83 is the diagnosis code used for Other Fatigue. It is a condition marked by drowsiness and an unusual lack of energy and mental alertness. It can be caused by many things, including illness, injury, or drugs.
What is a CPT 9 code?
A Current Procedures Terminology (CPT) code is a procedure such as an ABR or reflex testing. The International Statistical Classification of Diseases and Related Health Problems (usually abbreviated as ICD) is in its 9th revision. The ICD-9 is a diagnostic code such as 388.30 for tinnitus, unspecified.
How do I find ICD codes?
If you need to look up the ICD code for a particular diagnosis or confirm what an ICD code stands for, visit the Centers for Disease Control and Prevention (CDC) website to use their free searchable database of current ICD-10 codes.
What is difference between ICD-9 and ICD-10?
ICD-9 uses mostly numeric codes with only occasional E and V alphanumeric codes. Plus, only three-, four- and five-digit codes are valid. ICD-10 uses entirely alphanumeric codes and has valid codes of up to seven digits.
How many ICD-9 codes are there?
13,000 codesThe current ICD-9-CM system consists of ∼13,000 codes and is running out of numbers.
Why did ICD-10 replace ICD-9?
ICD-9 follows an outdated 1970's medical coding system which fails to capture detailed health care data and is inconsistent with current medical practice. By transitioning to ICD-10, providers will have: Improved operational processes by classifying detail within codes to accurately process payments and reimbursements.
When did ICD-10 replace ICD-9?
Objective-On October 1, 2015, the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) replaced ICD-9-CM (Ninth Revision) as the diagnosis coding scheme for the U.S. health care system.
When is CTA indicated?
CTA of the coronary veins is indicated when imaging of the coronary venous anatomy is necessary for biventricular pacemaker lead insertion.
Is a cardiac angiography test considered medically necessary?
The test will be considered not medically necessary if pretest evaluation indicates that the patient would require invasive cardiac angiography for further diagnosis or for therapeutic intervention.
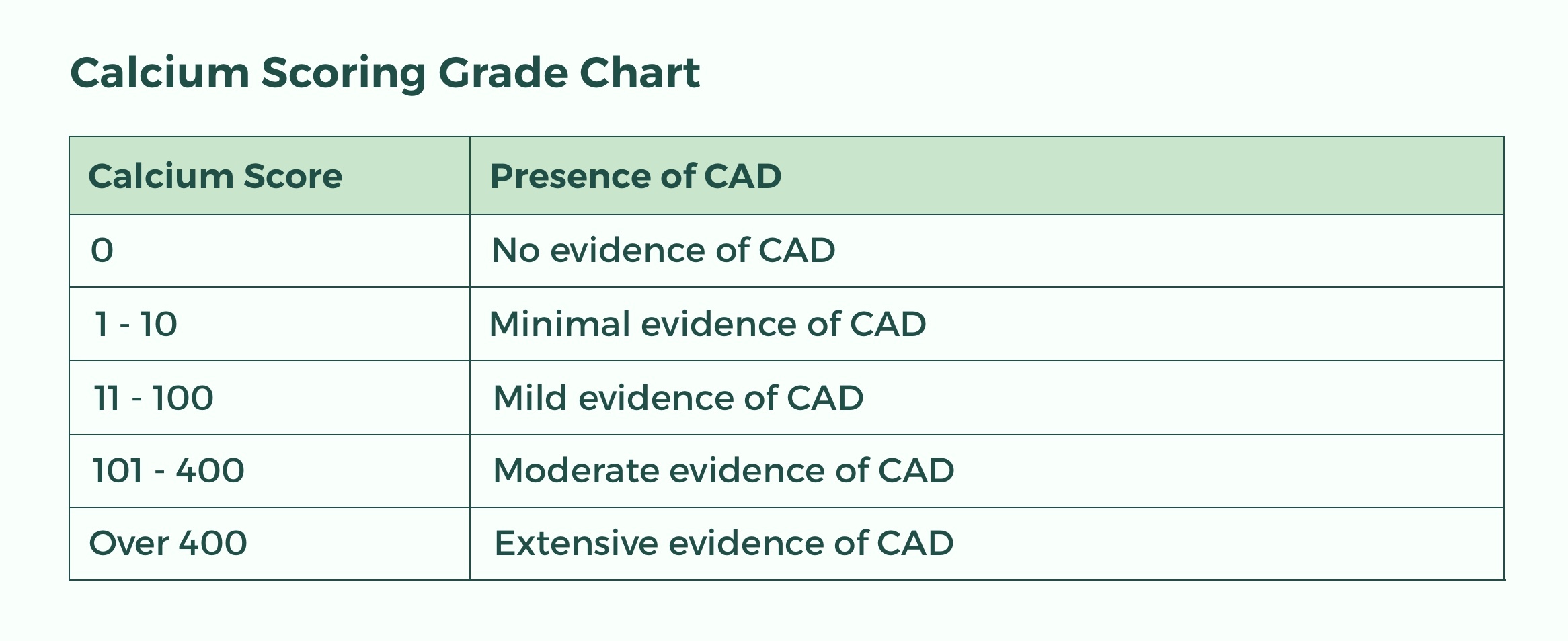
Does CCTA rule out CAD?
Current available body of evidence demonstrates that CCTA can reliably rule out the presence of significant coronary artery disease (CAD) in patients with a low to intermediate probability of having CAD and can reliably achieve a high degree of diagnostic accuracy and technical performance necessary to replace conventional angiography.

Popular Posts:
- 1. icd 9 code for pid
- 2. what is the icd 10 procedure code for insertion of dual chamber pacemaker
- 3. icd 10 code for feeding tube dysfunction
- 4. icd 10 code for dehiscence of surgical wound
- 5. icd 10 code for gait imbalance
- 6. icd 10 code for lr transverse process fracture
- 7. icd 9 code for cva kidney pain
- 8. icd 10 code for left quadrant pain
- 9. icd 10 code for all
- 10. icd 10 code for femoral neck fracture