Full Answer
What is the CPT code for cervical disc arthroplasty?
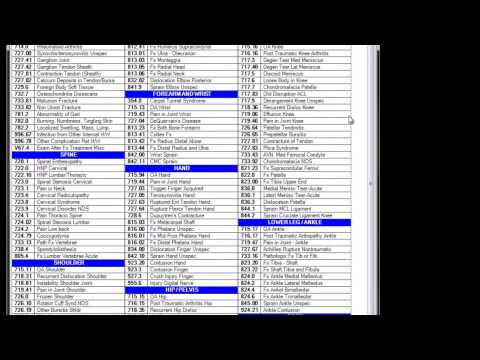
Single-level cervical disc arthroplasty procedures are currently described by CPT code 22856: Total disc arthroplasty (artificial disc), anterior approach, including discectomy with endplate preparation (includes osteophytectomy for nerve root or spinal cord decompression and microdissection), single interspace, cervical.
What is the ICD-9 code for cervical radiculopathy?
ICD-9 Code for Cervical Radiculopathy. You might know that ICD-9-CM codes are used in medical billing and coding to describe diseases, injuries, symptoms and conditions. ICD-9-CM 723.4 is used for Cervical Radiculopathy including Brachia neuritis or radiculitis; cervical radiculitis, radicular symdrome of upper limbs. It applies to:
What is the CPT code for cervical osteotomy?
Individual CPT Codes – Cervical. 22210 - osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment, this code is a primary code but -51 modifier should be used as other higher value codes would typically precede this code; 22216 - additional levels of osteotomies.
What is the ICD 10 code for cervical disc disorder?
ICD-10-CM Diagnosis Code M51.9. Unspecified thoracic, thoracolumbar and lumbosacral intervertebral disc disorder. 2016 2017 2018 2019 2020 2021 Billable/Specific Code. cervical M50.90. ICD-10-CM Diagnosis Code M50.90. Cervical disc disorder, unspecified, unspecified cervical region.
What is the ICD-9 code for cervical fusion?
Patients receiving ACDF (defined as anterior cervical fusion (ICD-0 code=81.02) + excision of intervertebral disc (80.51)) were extracted; those with three or more levels fused (ICD-9 codes 81.63-81.64), cancer (ICD-9 codes 140-239), or trauma (ICD-9 codes=805.0-806.9) were excluded.
What is the ICD-10 code for cervical fusion?
ICD-10 code M43. 22 for Fusion of spine, cervical region is a medical classification as listed by WHO under the range - Dorsopathies .
What are ICD-9 procedure codes?
ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started.
What is the difference between ICD-10 and 9?
ICD-9 uses mostly numeric codes with only occasional E and V alphanumeric codes. Plus, only three-, four- and five-digit codes are valid. ICD-10 uses entirely alphanumeric codes and has valid codes of up to seven digits.
What is the ICD-10 code for status post fusion?
Fusion of spine, site unspecified The 2022 edition of ICD-10-CM M43. 20 became effective on October 1, 2021.
What is the ICD-10 code for Acdf surgery?
Fusion of Cervical Vertebral Joint with Nonautologous Tissue Substitute, Anterior Approach, Anterior Column, Open Approach. ICD-10-PCS 0RG10K0 is a specific/billable code that can be used to indicate a procedure.
Are ICD-9 codes still used in 2021?
CMS will continue to maintain the ICD-9 code website with the posted files. These are the codes providers (physicians, hospitals, etc.) and suppliers must use when submitting claims to Medicare for payment.
What is the difference between a CPT code and an ICD-9 code?
In a concise statement, ICD-9 is the code used to describe the condition or disease being treated, also known as the diagnosis. CPT is the code used to describe the treatment and diagnostic services provided for that diagnosis.
What are ICD-9 10 and CPT codes?
ICD-10-CM diagnosis codes provide the reason for seeking health care; ICD-10-PCS procedure codes tell what inpatient treatment and services the patient got; CPT (HCPCS Level I) codes describe outpatient services and procedures; and providers generally use HCPCS (Level II) codes for equipment, drugs, and supplies for ...
Did ICD-10 replace ICD-9?
Objective-On October 1, 2015, the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) replaced ICD-9-CM (Ninth Revision) as the diagnosis coding scheme for the U.S. health care system.
Is ICD-9 still used in 2020?
Easier comparison of mortality and morbidity data Currently, the U.S. is the only industrialized nation still utilizing ICD-9-CM codes for morbidity data, though we have already transitioned to ICD-10 for mortality.
Why did ICD-9 change to ICD-10?
ICD-9 follows an outdated 1970's medical coding system which fails to capture detailed health care data and is inconsistent with current medical practice. By transitioning to ICD-10, providers will have: Improved operational processes by classifying detail within codes to accurately process payments and reimbursements.
What is the ICd 9 code for radiculopathy?
You might know that ICD-9-CM codes are used in medical billing and coding to describe diseases, injuries, symptoms and conditions. ICD-9-CM 723.4 is used for Cervical Radiculopathy including Brachia neuritis or radiculitis; cervical radiculitis, radicular symdrome of upper limbs. It applies to: 1 Cervical radiculitis 2 Radicular syndrome of upper limbs
How do you know if you have cervical radiculopathy?
Following are some symptoms which indicate that you might have Cervical Radiculopathy, such as : Pain that spreads into the arm, neck, chest, upper back and/or shoulders. Muscle weakness and/or numbness or tingling in fingers or hands.
What is the best treatment for cervical radiculopathy?
Important ones include: A combination of powerful anti-inflammatory drugs such as corticosteroids, Non-steroidal pain medication like ibuprofen or naproxen.
What is the best way to reduce pain in cervical spine?
Physical therapy, that might include gentle cervical traction and mobilization, exercises, and other modalities to reduce pain.
Is cervical artificial disc replacement necessary?
Cervical artificial disc replacement is proven and medically necessary for treatment of persons with symptoms of degenerative disc disease at one level even if they have radiological evidence of degenerative disc disease at multiple levels . Radiologic evidence of degenerative disc disease is common in persons who are middle aged and older and does not necessarily correlate with clinical symptoms. Cervical artificial total disc replacement is proven and medically necessary for the treatment of symptomatic contiguous two level degenerative disc disease in skeletally mature patients when used according to U.S. Food and Drug Administration (FDA) labeled indications. (Note: not all cervical artificial discs have FDA labeling for contiguous two level degenerative disc disease. Only cervical artificial discs FDA labeled for contiguous two level disease are proven and medically necessary for this indication.) Cervical artificial disc replacement at one level combined with cervical spinal fusion surgery at another level (adjacent or non-adjacent) performed at the same surgical setting is unproven and not medically necessary. This is commonly referred to as a hybrid surgery. There is insufficient published clinical evidence in peer-reviewed medical literature demonstrating the safety and efficacy of combination cervical spine surgery at multiple adjacent or non-adjacent levels.
Do you need a letter of medical necessity for cervical disc arthroplasty?
It is not always necessary to submit a Letter of Medical Necessity (LOMN). However, a letter from the treating physician may help to ensure approval for cervical disc arthroplasty using the PCM® device. The LOMN should contain the following elements:
Does Cigna cover cervical intervertebral disc surgery?
Cigna®(effective December 2015) Reference link to Cigna (Policy #0104): https://cignaforhcp.cigna.com/public/content/pdf/coveragePolicies/medical/mm_0104_ coveragepositioncriteria_intervebral_disc_prosthesis.pdf Cigna covers surgical implantation of FDA–approved cervical intervertebral disc (IVD) prosthesis for degenerative cervical disc disease with intractable radiculopathy and/or myelopathy as medically necessary in a skeletally mature individual when ALL of the following criteria are met: • Unremitting neck and arm pain, resulting in disability and/or neurological deficit that are refractory to at least six weeks of standard medical and surgical management (e.g., reduced activities, exercise, analgesics, physical therapy). • Single-level disc degeneration has been confirmed on complex imaging studies (i.e., computerized tomography [CT] scan, magnetic resonance imaging [MRI]). • The planned implant will be used in the reconstruction of a cervical disc at C3-C7, following single-level discectomy. • The individual is a candidate for single-level anterior cervical decompression and interbody fusion. Cigna does not cover the surgical implantation of a cervical intervertebral disc (IVD) prosthesis for ANY other indication, including the following because each is considered experimental, investigational or unproven: • The planned procedure includes the combined use of a prosthesis and spinal fusion (i.e., hybrid surgery) • Simultaneous multilevel implantation is planned • The individual had prior fusion at an adjacent cervical level • The individual had prior surgery at the treated level • Osteopenia, osteomalacia, or osteoporosis (T-score of -3.5, or -2.5, with vertebral crush fracture) • Neck or arm pain of unknown etiology • Absence of neck and/or arm pain • Progressive neurological deficit or deterioration • Infection, systemic or local • Rheumatoid arthritis or other autoimmune disease • Paget’s disease, osteomalacia, or any other metabolic bone disease • There is radiological evidence of ANY of the following: - Clinically significant cervical instability, such as kyphotic deformity or spondylolisthesis (e.g., > 3.5mm subluxation or > 11° angulation) - Significant cervical anatomical deformity or compromised vertebral bodies at the index level (e.g., ankylosing spondylitis, rheumatoid arthritis, or compromise due to current or past trauma) - Multilevel degenerative disc - Spinal metastases • Non FDA–approved cervical disc prosthesis
Does Medicare cover cervical CAD?
The payor coverage landscape for cervical artificial disc replacement (CAD) is a fluid and increasingly positive one. Medicare does not have a national coverage decision. Therefore, coverage is determined by the local Medicare Administrative Contractors (MACs). Most MACs are silent regarding cervical disc arthroplasty. However, it is always wise to research the current MACs’ coverage position, as it may change at any time. Aetna,®Cigna,®and UnitedHealthcare,®as well as many BlueCross®BlueShield®plans, provide cervical disc arthroplasty coverage. It is always wise to be familiar with the coverage requirements and restrictions for the relevant contracted payors. For your reference, the current cervical disc arthroplasty-PCM®coverage requirements for various large, national commercial payors include the following (as these coverage policies are subject to change when updated by the payors). Providers should verify coverage with particular patient’s health plan.
Does Medicare require prior authorization for cervical disc arthroplasty?
Many commercial payors require prior authorization (sometimes called pre-certification) for cervical disc arthroplasty. Medicare does not provide or require “prior authorization” for services. The steps in the prior authorization process typically are as follows:
Can Humana members get intervertebral disc replacement?
Humana members may NOT be eligible under the Plan for cervical artificial intervertebral disc replacement for any indications other than those listed above including, but may not be limited to: • Multilevel cervical disc replacement; OR • Partial cervical disc replacement; OR • Planned procedure including a combined use of a cervical artificial intervertebral disc replacement and spinal fusion; OR • Prior fusion at an adjacent cervical level; OR • Prior surgery at the treated level
When will the ICD-10 Z96.698 be released?
The 2022 edition of ICD-10-CM Z96.698 became effective on October 1, 2021.
What is a Z77-Z99?
Z77-Z99 Persons with potential health hazards related to family and personal history and certain conditions influencing health status
Popular Posts:
- 1. icd-10 code for neck mass
- 2. icd 9 code for cardiac rehab
- 3. 2018 icd 10 code for fracture left proximal radius radial head
- 4. icd 10 code for vasomotor flushing
- 5. icd 10 cm code for drainage from the ear
- 6. icd 9 code for n92.0
- 7. icd-10-cm code for malignant embryoma, right kidney (primary malignancy)
- 8. icd 10 code for factor 5 leiden mutation
- 9. icd 10 code for post op cholecystectomy
- 10. icd 10 cm code for alcohol use