What is the ICD 9 code for prophylactic chemotherapy?
2012 ICD-9-CM Diagnosis Code V07.39 : Need for other prophylactic chemotherapy Free, official information about 2012 (and also 2013-2015) ICD-9-CM diagnosis code V07.39, including coding notes, detailed descriptions, index cross-references and ICD-10-CM conversion.
What is the CPT code for chemotherapy?
Although CPT code 99211 is ineligible for reporting with chemotherapy and non-chemotherapy drug/substance administration HCPCS/CPT codes, other non-facility-based E&M CPT codes (e.g., 99202-99205, 99212-99215) are individually reportable with modifier 25 if the physician contains a tremendous and separately identifiable E&M service.
What is the ICD 10 code for peritoneal chemotherapy?
96446 refers to chemotherapy administration into the peritoneal cavity via indwelling port or catheter. It is not time based. This single code covers all infusions into the peritoneal cavity for that day and does not include peritoneocentesis. What ICD code do you use for laboratory testing done on a day prior to chemotherapy administration?
Is the chemotherapy administration code supported in claims processing?
Claims processing of the chemotherapy administration code is supported by the billed, approved chemotherapy drug. If a drug is not billed along with the administration code, the administration will currently deny.

What is the ICD-10 code for chemotherapy?
1 for Encounter for antineoplastic chemotherapy and immunotherapy is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD-10 code for pre chemotherapy?
Report ICD-10 code Z01. 818, Encounter for other preprocedural examination (is defined as Encounter for preprocedural examination NOS and Encounter for examinations prior to antineoplastic chemotherapy), when the test is performed as a baseline study before chemotherapy. List Z01. 818 as your primary diagnosis code.
What is the ICD-9 code for cancer?
Comprehensive ICD-9-CM Casefinding Code List for Reportable Tumors (Effective Date 1/1/2014)ICD-9-CM Code*Explanation of ICD-9-CM Code140._ - 172._, 174._ - 209.36, 209.7_Malignant neoplasms (excluding category 173), stated or presumed to be primary (of specified sites) and certain specified histologies122 more rows
What diagnosis is V58 69?
V58. 69 - Long-term (current) use of other medications. ICD-10-CM. Centers for Medicare and Medicaid Services and the National Center for Health Statistics; 2018.
How do you code chemotherapy?
Code 96413 (chemotherapy administration, intravenous infusion technique; up to one hour, single or initial substance/drug) would be used to report the first 90 minutes of the infusion.
What is the ICD 10 code for long term use of chemotherapy?
ICD-10 Code for Other long term (current) drug therapy- Z79. 899- Codify by AAPC.
What is the ICD-10 code for cancer?
ICD-10-CM Code for Malignant (primary) neoplasm, unspecified C80. 1.
What is Malignant neoplasm unspecified?
A malignant neoplasm (NEE-oh-plaz-um) is another term for a cancerous tumor. The term “neoplasm” refers to an abnormal growth of tissue. The term “malignant” means the tumor is cancerous and is likely to spread (metastasize) beyond its point of origin.
What is the ICD-9 code for lymphoma?
ICD-9-CM Diagnosis Code 202.8 : Other malignant lymphomas.
What is diagnosis code Z51 81?
ICD-10 code Z51. 81 for Encounter for therapeutic drug level monitoring is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is diagnosis code for high risk medication?
ICD-10-CM Diagnosis Code Z79 Z79.
What does a diagnosis of high risk medication use mean?
A high-risk medicine is one that may cause serious health problems if not taken the right way, or taken with another drug or food item that it may interact with. Some examples include: Medicine that makes you drowsy, causes depression or confusion, or has other potentially dangerous side effects.
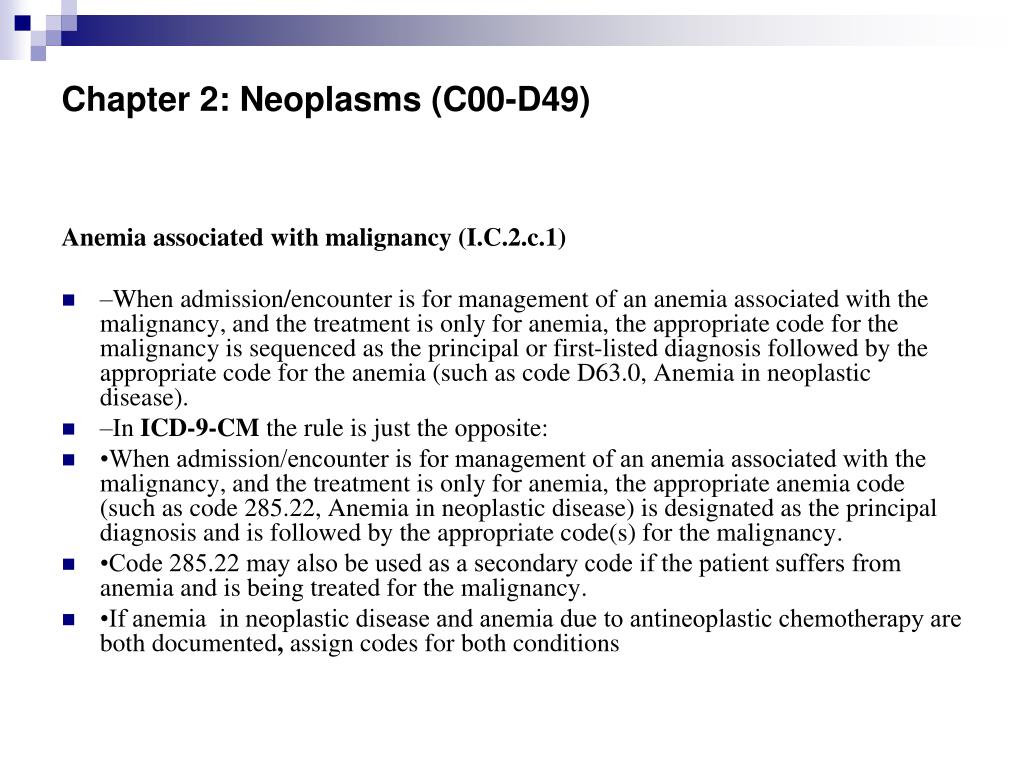
Can anemia be treated during chemotherapy?
Anemia, a common side effect of chemotherapy, must be treated during the course of therapy. The provider should document the specific type of anemia to meet medical necessity requirements when billing for anemia drugs during the course of treatment.
Do you have to accurately document and code chemotherapy administration services?
You must accurately document and code chemotherapy administration services to properly bill for the resources and supplies consumed. To ensure that the practice is compensated for the services rendered, be sure to address the following documentation issues that can result in improper charge capture and billing.
What is the code for chemo in the peritoneal cavity?
96446 refers to chemotherapy administration into the peritoneal cavity via indwelling port or catheter. It is not time based. This single code covers all infusions into the peritoneal cavity for that day and does not include peritoneocentesis.
What is the E&M code for chemo?
If the doctor sees the patient at the hospital on the day of the chemo, they could bill the appropriate E&M code but could not bill for the administration (i.e., 96365-96379 or 96401-965 49). Chemotherapy administration codes reimburse primarily for the overhead/personnel costs of the infusion center. You can only bill for chemotherapy administration if you own the facility. If it is a hospital–based infusion center, you cannot collect for chemo administration. However, the amount of physician work associated with most chemo admin codes is only about 0.5 RVUs. You can charge for E&M codes if they are separately identifiable services. You then must document what was done and show medical justification for the visit. It should not be duplicative of clinic visits.
What is the diagnosis code for a port flush?
If the patient is seen only for a port flush, code 96523 should be used. If you use a de-clotting or thrombolytic agent, you should use code 36550. Also remember to use the J-code for the specific thrombolytic agent used. The diagnosis code should be the patient’s primary cancer and Z45.2 (encounter for adjustment and management ...
Can you bill for chemotherapy?
You can only bill for chemotherapy administration if you own the facility. If it is a hospital–based infusion center, you cannot collect for chemo administration. However, the amount of physician work associated with most chemo admin codes is only about 0.5 RVUs.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Language quoted from Centers for Medicare and Medicaid Services (CMS), National Coverage Determinations (NCDs) and coverage provisions in interpretive manuals is italicized throughout the policy.
Article Guidance
The Medicare Administrative Contractor has determined in review of submitted claims that there is inappropriate use of CPT codes 96401-96549 for chemotherapy and other highly complex drug or highly complex biologic agent administration.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What modifier is used for E/M?
If a significant separately identifiable E/M service is performed, the appropriate E/M code should be reported using modifier 25 in addition to the chemotherapy code. For an E/M service provided on the same day, a different diagnosis is not required.
Is the chemotherapy code billed?
Claims processing of the chemotherapy administration code is supported by the billed, approved chemotherapy drug. If a drug is not billed along with the administration code, the administration will currently deny. Effective October 15, 2018, the administration code will return to provider (RTP) if an approved chemotherapy drug is not billed on ...
Proper Documentation of Infusion Start/Stop Times
Documentation of Anemia
- Anemia, a common side effect of chemotherapy, must be treated during the course of therapy. The provider should document the specific type of anemia to meet medical necessity requirements when billing for anemia drugs during the course of treatment.
Charge Capture of Correct Units
- If chemotherapy drugs are hard-coded into a charge description master (CDM) or fee schedule, cross check the chemotherapy drug units administered against how that drug is set up in the office billing system. The maximum allowable fee per unit is based on the HCPCS Level II description of the chemotherapy drug. Errors are often made and drugs are frequently under-bill…
Popular Posts:
- 1. icd-10 code for clotted av fistula
- 2. icd 10 code for atv accident driver
- 3. icd 10 cm code for past smoker
- 4. icd 10 dx code for influenza b
- 5. icd 10 code for fuchs dystrophy bilateral
- 6. what is the icd 10 code for osteochondral patella fracture
- 7. icd 9 code for diabetic ulcer of foot
- 8. icd 10 code for separation of muscle
- 9. icd 10 cm code for uterine fibroid tumor in pregnancy week 14
- 10. icd 10 code for human papillomavirus