Full Answer
What does ICD 9 cm stand for in insurance?
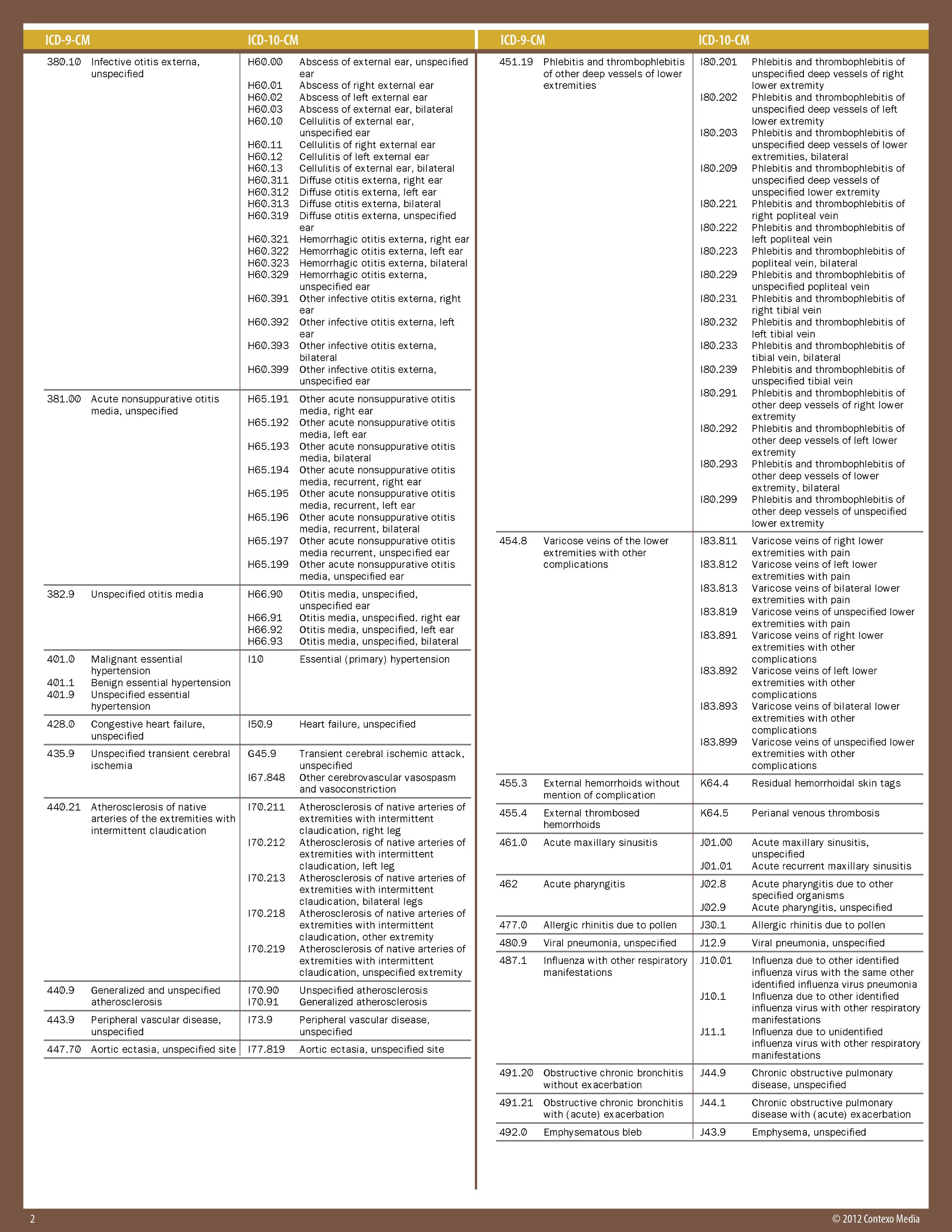
INTERNATIONAL CLASSIFICATION OF DISEASES, 9TH REVISION, CLINICAL MODIFICATION ICD-9-CM VOLUMES 1 & 2 (DIAGNOSES) is the code set used by Non-HIPAA covered entities (Workers’ Compensation and auto insurance companies) “that were not required to be converted to ICD-10.
What is the format for ICD 9 diagnosis codes?
The format for ICD-9 diagnoses codes is a decimal placed after the first three characters and two possible add-on characters following: xxx.xx. ICD-9 PCS were used to report procedures for inpatient hospital services from Volume 3, which represent procedures that were done at inpatient hospital facilities.
What is included in the ICD-9-CM?
The ICD-9-CM consists of: a tabular list containing a numerical list of the disease code numbers in tabular form; a classification system for surgical, diagnostic, and therapeutic procedures (alphabetic index and tabular list).
What is an ICD 9 code with 3 digits?
ICD-9-CM diagnosis codes are composed of codes with 3, 4, or 5 digits. Codes with three digits are included in ICD-9-CM as the heading of a category of codes that may be further subdivided by the use of fourth and/or fifth digits, which provide greater detail.

How is ICD coding relevant to the long term care setting?
Diagnostic coding plays several important roles in every healthcare setting, including long-term care (LTC) nursing facilities. LTC facilities assign ICD-9-CM codes to capture a resident's clinical conditions. ICD-9-CM facilitates the collection and organization of healthcare statistics on the incidence of diseases.
Are ICD-9 codes still used in 2021?
CMS will continue to maintain the ICD-9 code website with the posted files. These are the codes providers (physicians, hospitals, etc.) and suppliers must use when submitting claims to Medicare for payment.
What are ICD-9 procedure codes?
ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started.
What are ICD-9 and 10 codes?
Code Structure: Comparing ICD-9 to ICD-10ICD-9-CMICD-10-CMFirst character is numeric or alpha ( E or V)First character is alphaSecond, Third, Fourth and Fifth digits are numericAll letters used except UAlways at least three digitsCharacter 2 always numeric; 3 through 7 can be alpha or numeric3 more rows•Aug 24, 2015
Why are ICD-9 codes no longer used?
The periodic revisions of ICD-9-CM mirror changes in the medical and health care field. The U.S. has been using ICD-9-CM since 1979, and it is not sufficiently robust to serve the health care needs of the future.
When was ICD-9 discontinued?
Therefore, CMS is to eliminating the 90-day grace period for billing discontinued ICD-9- CM diagnosis codes, effective October 1, 2004.
What is an example of an ICD-9 code?
Most ICD-9 codes are three digits to the left of a decimal point and one or two digits to the right of one. For example: 250.0 is diabetes with no complications. 530.81 is gastroesophageal reflux disease (GERD).
What is the difference between a CPT code and an ICD-9 code?
In a concise statement, ICD-9 is the code used to describe the condition or disease being treated, also known as the diagnosis. CPT is the code used to describe the treatment and diagnostic services provided for that diagnosis.
How many ICD-9 codes are there?
13,000 codesThe current ICD-9-CM system consists of ∼13,000 codes and is running out of numbers.
What does ICD-9 stand for?
International Classification of Diseases,Ninth RevisionInternational Classification of Diseases,Ninth Revision (ICD-9) Related Pages. The International Classification of Diseases (ICD) is designed to promote international comparability in the collection, processing, classification, and presentation of mortality statistics.
What does ICD-10 stand for?
A: ICD-10-CM (International Classification of Diseases -10th Version-Clinical Modification) is designed for classifying and reporting diseases in all healthcare settings.
What is an ICD-10 diagnosis code?
Used for medical claim reporting in all healthcare settings, ICD-10-CM is a standardized classification system of diagnosis codes that represent conditions and diseases, related health problems, abnormal findings, signs and symptoms, injuries, external causes of injuries and diseases, and social circumstances.
What is the ICd 9 code for symptoms?
Chapter 16 of ICD-9-CM, Symptoms, Signs, and Ill-defined conditions (codes 780.0 - 799.9) contain many, but not all codes for symptoms.
What are the conventions of ICd 9?
The conventions for the ICD-9-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the index and tabular of the ICD -9-CM as instructional notes. The conventions are as follows:
What is a category 250 code?
Codes under category 250, Diabetes mellitus, identify complications/manifestations associated with diabetes mellitus. A fifth-digit is required for all category 250 codes to identify the type of diabetes mellitus and whether the diabetes is controlled or uncontrolled.
What is the code for MRSA?
If a patient is documented as having both MRSA colonization and infection during a hospital admission, code V02.54, Carrier or suspected carrier, Methicillin resistant Staphylococcus aureus, and a code for the MRSA infection may both be assigned.
What are conventions and guidelines?
The conventions, general guidelines and chapter-specific guidelines are applicable to all health care settings unless otherwise indicated. The conventions and instructions of the classification take precedence over guidelines.
What is code assignment?
Code assignment is based on the provider’s documentation of the relationship between the condition and the care or procedure. The guideline extends to any complications of care, regardless of the chapter the code is located in. It is important to note that not all conditions that occur during or following medical care or surgery are classified as complications. There must be a cause-and-effect relationship between the care provided and the condition, and an indication in the documentation that it is a complication. Query the provider for clarification, if the complication is not clearly documented.
When are 760-763 codes assigned?
Codes from categories 760-763, Maternal causes of perinatal morbidity and mortality, are assigned only when the maternal condition has actually affected the fetus or newborn. The fact that the mother has an associated medical condition or experiences some complication of pregnancy, labor or delivery does not justify the routine assignment of codes from these categories to the newborn record.
What is the ICd-9 GEM?
The GEMs are the raw material from which providers, health information vendors and payers can derive specific applied mappings to meet their needs.
What is the ICd 10 code for alcohol dependence?
303.91 is a legacy non-billable code used to specify a medical diagnosis of other and unspecified alcohol dependence, continuous. This code was replaced on September 30, 2015 by its ICD-10 equivalent.
What is continuous home care?
Continuous home care is to be provided only during periods of crisis to maintain the beneficiary at home. Continuous care cannot be provided in a skilled nursing facility (SNF), inpatient hospital, inpatient hospice facility, a long term care hospital (LTCH), or an inpatient psychiatric facility. A period of crisis is a period of time ...
When aide hours exceed the nursing hours, routine home care must be billed?
When aide hours exceed the nursing hours, routine home care must be billed. Examples of counting continuous home care hours are as follows: If less than 8 hours of care was given or if death occurs before 8 hours, do not count the hours as continuous care; bill the day as a routine home care day. Medical social workers, counselors, pastoral ...
How many hours of hospice care is considered continuous care?
If within a 24 hour period, 6 hours of care is provided by a hospice aide, and 4 hours of care is provided by a skilled nurse, do not count the hours as continuous care since at least 50 percent of the total care provided was not provided by a nurse. This would be billed as routine.
What time does skilled nursing care end?
Care that spans midnight (e.g., 4 hours of skilled nursing care is provided from 8:00 p.m. to 12:00 a.m. and from 12:00 a.m. to 4:00 a.m.) cannot be billed as continuous care hours. Supportive Documentation for Continuous Home Care.
How often should I do supportive documentation for CHC?
Although CHC is billed in 15-minute increments, the supportive documentation is not required to be every 15 minutes. Supportive documentation should be as frequent as necessary to support continued CHC, and is suggested at least hourly. Updated: 07.25.12.
How long is a period of crisis?
A period of crisis is a period of time when the beneficiary requires the higher level of “continuous care” for at least 8 hours in a 24-hour period (midnight to midnight) to achieve palliation or management of acute medical symptoms.
Can medical social workers be counted as continuous care hours?
Medical social workers, counselors, pastoral care, and bereavement counseling by any staff member certainly may be appropriate and valuable in the home during a crisis; however, those hours may not be counted in the continuous care hours.
What is the CPT code for transitional care management?
The CPT® guidelines for transitional care management (TCM) codes 99495 and 99496 seem straightforward, initially, but the details are trickier than is commonly recognized. Here’s what you need to know to report these services appropriately.
What is the TCM number for medication management?
Medication therapy management services (99487-99489) Medication management therapy services (99605-99607) Lastly, if a provider performs a procedure with a global period, then the same provider may not bill TCM services during the global period.
How long does a TCM provider have to bill for E/M?
Although TCM codes require continuous provider access from the moment of discharge through 29 days post discharge, the provider may bill separately for additional evaluation and management (E/M) services provided within the month if performed on a date after the initial face-to-face visit.
Popular Posts:
- 1. icd 10 code for test anxiety recurrent
- 2. icd 10 code for pt with diabetes, cva, and hypertension
- 3. icd 9 code for mvc
- 4. icd 9 code for cad with stent placement
- 5. icd 9 code for strain of muscle, facia & tendon of abdomin
- 6. icd 10 code for hypotension with shock
- 7. icd-10 code for venoud dysdid lymphrfrms
- 8. icd 10 code for tear at the posterior root attachment of the medial meniscus
- 9. icd 10 code for left soleal vein thrombosis
- 10. icd 10 code for hemorrhoids internal