What is the ICD 10 code for diabetic gastroparesis?
Applicable To Diabetes mellitus due to underlying condition with diabetic gastroparesis. E08.43, ICD-10-CM Diagnosis Code E09.43. Drug or chemical induced diabetes mellitus with neurological complications with diabetic autonomic (poly)neuropathy 2016 2017 2018 2019 Billable/Specific Code.
What is the CPT code for Type 1 diabetes mellitus?
Codes E08 Diabetes mellitus due to underlying condition E09 Drug or chemical induced diabetes mellitus E10 Type 1 diabetes mellitus E11 Type 2 diabetes mellitus E13 Other specified diabetes mellitus
What is the ICD 10 code for diabetes mellitus with coma?
ICD-10 Codes for Diabetes Due to an Underlying Condition Diabetes mellitus due to underlying condition: E08 Diabetes mellitus due to underlying condition with hyperosmolarity: E08.0 …… without nonketotic hyperglycemic-hyperosmolar coma (NKHHC): E08.00 …… with coma: E08.01
What is the ICD-10 code for diabetes mellitus due to underlying condition?
ICD-10 Codes for Diabetes Due to an Underlying Condition Diabetes mellitus due to underlying condition: E08 Diabetes mellitus due to underlying condition with hyperosmolarity: E08.0 …… without nonketotic hyperglycemic-hyperosmolar coma (NKHHC): E08.00

What is the ICD-10 code for diabetes with gastroparesis?
ICD-10 code K31. 84 for Gastroparesis is a medical classification as listed by WHO under the range - Diseases of the digestive system .
What is the code for a type 2 DM with gastroparesis?
ICD-10 code E11. 43 which has Type 2 diabetes with diabetic gastroparesis listed under this code, does not instruct to include code for gastroparesis. However K31. 84 instructs to code first underlying disease if known, such as: diabetes, (one of which listed is E11.
How do you code gastroparesis?
K31. 84 – is the ICD-10 diagnosis code to report gastroparesis. Also known as delayed gastric emptying, gastroparesis is a chronic condition that affects the motility in the stomach.
What is the ICD-10 for gastroparesis?
S3152 ICD-10 Coding for Gastroparesis: An Institutional Electronic Health Record Validation.
What is gastroparesis and diabetes?
Gastroparesis, also called delayed gastric emptying, is a disorder in which the stomach takes too long to empty its contents. It often occurs in people with type 1 diabetes or type 2 diabetes. Gastroparesis happens when nerves to the stomach are damaged or stop working.
What is DM with gastroparesis?
People with diabetes are at increased risk for gastroparesis—a digestive disorder that can cause severe symptoms and affect quality of life. Diabetes is the most common known cause of gastroparesis, a digestive disorder that may lead to poor nutrition, problems managing blood glucose, and a reduced quality of life.
What are the symptoms of diabetic gastroparesis?
Signs and symptoms of gastroparesis include:Vomiting.Nausea.Abdominal bloating.Abdominal pain.A feeling of fullness after eating just a few bites.Vomiting undigested food eaten a few hours earlier.Acid reflux.Changes in blood sugar levels.More items...•
What is the ICD-10 code for diabetes?
E08. 1 Diabetes mellitus due to underlying condition... E08. 10 Diabetes mellitus due to underlying condition...
What is the ICD-10 code for type 1 diabetes?
ICD-10 code E10. 9 for Type 1 diabetes mellitus without complications is a medical classification as listed by WHO under the range - Endocrine, nutritional and metabolic diseases .
What is the ICD-10 code for hyperglycemia?
ICD-10 code R73. 9 for Hyperglycemia, unspecified is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD-10 code for gastroenteritis?
ICD-10 code A09 for Infectious gastroenteritis and colitis, unspecified is a medical classification as listed by WHO under the range - Certain infectious and parasitic diseases .
What is the ICD-10 code for early satiety?
R68. 81 Early satiety - ICD-10-CM Diagnosis Codes.
When do you code E11 59?
ICD-10-CM Code for Type 2 diabetes mellitus with other circulatory complications E11. 59.
What is the ICD 10 code for type 2 diabetes?
ICD-Code E11* is a non-billable ICD-10 code used for healthcare diagnosis reimbursement of Type 2 Diabetes Mellitus. Its corresponding ICD-9 code is 250. Code I10 is the diagnosis code used for Type 2 Diabetes Mellitus.
When do you code E11 69?
ICD-10-CM Code for Type 2 diabetes mellitus with other specified complication E11. 69.
When do you use E11 59?
Type 2 diabetes mellitus with other circulatory complications. E11. 59 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the DCSI for diabetes?
The Diabetes Complications Severity Index (DCSI) converts diagnostic codes and laboratory results into a 14-level metric quantifying the long-term effects of diabetes on seven body systems. Adoption of the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) necessitates translation from ICD-9-CM and creates refinement opportunities. ICD-9 codes for secondary and primary diabetes plus all five ICD-10 diabetes categories were incorporated into an updated tool. Additional modifications were made to improve the accuracy of severity assignments. In the type 2 subpopulation, prevalence steadily declined with increasing score according to the updated DCSI tool, whereas the original tool resulted in an aberrant local prevalence peak at DCSI = 2. In the type 1 subpopulation, score prevalence was greater in type 1 versus type 2 subpopulations (3 versus 0) according to both instruments. Both instruments predicted current-year inpatient admissions risk and near-future mortality, using either purely ICD-9 data or a mix of ICD-9 and ICD-10 data. While the performance of the tool with purely ICD-10 data has yet to be evaluated, this updated tool makes assessment of diabetes patient severity and complications possible in the interim. Fig. 2. Prevalence and change in current-year admission risk by DCSI score; type 1 diabetes. NOTE: The intercept value for the admissions risk model, which is equivalent to admissions per 1000 for individuals with DCSI = 0, was 73.8 per 1000 (Young), 73.6 (updated DCSI, October 2014–September 2015), and 65.6 (updated DCSI, February 2015–January 2016). Type 2 diabetes mellitus is the most common form of diabetes and is currently a major worldwide cause of morbidity and mortality. This is likely to worsen, given th Continue reading >>
What is the correct ICD-9 code for diabetes mellitus?
Most coders can quickly come up with 250.00. And if the physician only documented diabetes mellitus , that’s the correct ICD-9-CM code. If a physician doesn’t document complications or type of diabetes, coders default to code 250.00 (diabetes mellitus without mention of complications), says Jill Young, CPC, CEDC, CIMC, president of Young Medical Consulting, LLC, in East Lansing, MI. However, 250.00 is not necessarily the best code to describe the patient’s actual condition. Consider these two patients. Patient A is a type 2 diabetic with well controlled diabetes. Patient B is a type 2 diabetic with uncontrolled diabetes who also suffers from diabetes-related chronic kidney disease. If the physician documents “diabetes mellitus” for both patients, coders would report the same code, even though the patients have very different conditions. The physician loses reimbursement on Patient B, who is sicker and requires more care, Young says. Coding in ICD-9-CM When it comes to the code assignment for diabetes mellitus in ICD-9-CM (250 code series), coders identify whether the diabetes is type 1or 2 using a fifth digit, says Shannon E. McCall, RHIA, CCS, CCS-P, CPC, CPC-I, CEMC, CCDS, director of HIM/coding for HCPro, Inc., in Danvers, Mass, and an AHIMA-approved ICD-10-CM/PCS trainer. If the diabetes is secondary, coders choose from codes in the 249 series. Under series 250, coders will find 10 different subcategories that further define and refine the patient’s actual condition. All of those codes require a fifth digit to indicate whether the diabetes is controlled or uncontrolled, type 1or type 2. The fifth digit subclassifications are: Coders also need to note that codes 250.4, 250.5, 250.6, 250.7, and 250.8 all include instructions to use an additional code to ide Continue reading >>
Is there more than one type of diabetes?
I'm pretty sure all of you who made it thus far in this article are familiar with the fact that there are at least two major types of diabetes: type I, or juvenile, and type II, with usual (though not mandatory) adult onset. Just like ICD-9, ICD-10 has different chapters for the different types of diabetes. The table below presents the major types of diabetes, by chapters, in both ICD coding versions. Diabetes Coding Comparison ICD-9-CM ICD-10-CM 249._ - Secondary diabetes mellitus E08._ - Diabetes mellitus due to underlying condition E09._ - Drug or chemical induced diabetes mellitus E13._ - Other specified diabetes mellitus 250._ - Diabetes mellitus E10._ - Type 1 diabetes mellitus E11._ - Type 2 diabetes mellitus 648._ - Diabetes mellitus of mother, complicating pregnancy, childbirth, or the puerperium O24._ - Gestational diabetes mellitus in pregnancy 775.1 - Neonatal diabetes mellitus P70.2 - Neonatal diabetes mellitus This coding structure for diabetes in ICD-10 is very important to understand and remember, as it is virtually always the starting point in assigning codes for all patient encounters seen and treated for diabetes. How To Code in ICD-10 For Diabetes 1. Determine Diabetes Category Again, "category" here refers to the four major groups above (not just to type 1 or 2 diabetes): E08 - Diabetes mellitus due to underlying condition E09 - Drug or chemical induced diabetes mellitus E10 - Type 1 diabetes mellitus E11 - Type 2 diabetes mellitus E13 - Other specified diabetes mellitus Note that, for some reason, E12 has been skipped. Instructions on Diabetes Categories Here are some basic instructions on how to code for each of the diabetes categories above: E08 - Diabetes mellitus due to underlying condition. Here, it is Continue reading >>
Is postprandial blood glucose a predictor of cardiovascular events?
Postprandial Blood Glucose Is a Stronger Predictor of Cardiovascular Events Than Fasting Blood Glucose in Type 2 Diabetes Mellitus, Particularly in Women: Lessons from the San Luigi Gonzaga Diabetes Study
What is the ICD-10 code for gastroparesis?
ICD-10 code E11.43 which has Type 2 diabetes with diabetic gastroparesis listed under this code, does not instruct to include code for gastroparesis. However K31.84 instructs to code first underlying disease if known, such as: diabetes, (one of which listed is E11.43). So, for diabetes with gastroparesis....require 2 codes or 1??
What is the code for diabetic gastroparesis?
Although "diabetes mellitus with diabetic gastroparesis" is listed as an inclusion term under the appropriate diabetes codes (E08.43, E09.43, E10.43, E11.43, and E13.43) , the code titles are not specific for this condition.
What is chapter 4 of the endocrine, nutritional, and metabolic diseases?
Chapter 4: Endocrine, Nutritional, and Metabolic Diseases (E00-E89) a. Diabetes mellitus . The diabetes mellitus codes are combination codes that include the type of diabetes mellitus, the body system affected, and the complications affecting that body system. So code only one code.
When should multiple coding not be used?
Multiple coding should not be used when the classification provides a combination code that clearly identifies all of the elements documented in the diagnosis. When the combination code lacks necessary specificity in describing the manifestation or complication, an additional code should be used as a secondary code.
Do you have to code both codes?
Yes both the codes must be coded !!
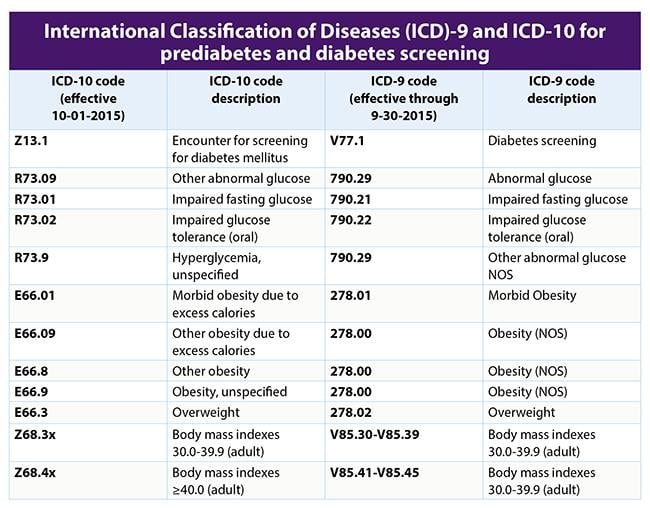
What Are ICD-10 Codes?
ICD-10 codes refer to the codes from the 10th Revision of the classification system. ICD-10 officially replaced ICD-9 in the US in October of 2015.
What is the ICD-10 code for diabetes?
For gestational diabetes (diabetes that occurs during pregnancy) women should be assigned a code under the 024.4 subheading and not any other codes under the 024 category.
What type of diabetes code should be used for long term use?
The code for long-term use of insulin, Z79.4, should also be used in these cases (unless insulin was just given to the patient as a one-time fix to bring blood sugar under control).
Why did doctors switch to ICd 10?
The switch to ICD-10 was a response to the need for doctors to record more specific and accurate diagnoses based on the most recent advancements in medicine. For this reason, there are five times more ICD-10 codes than there were ICD-9 codes. The ICD-10 codes consist of three to seven characters that may contain both letters and numbers.
When to use unspecified ICD-10?
The “unspecified” codes can be used when not enough information is known to give a more specific diagnosis; in that case, “unspecified” is technically more accurate than a more specific but as yet unconfirmed diagnosis. For more guidelines on using ICD-10 codes for diabetes mellitus, you can consult this document.
Can diabetes be a ICd 9?
Here's a conversion table that translates the old ICD-9 codes for diabetes to ICD-10 codes. There weren’t as many codes to describe different conditions in the ICD-9, so you’ll notice that some of them have more than one possible corresponding ICD-10 code. Some are also translated into a combination of two ICD-10 codes (note the use of the word "and").
When writing a medical code on a medical record, should you give the longest code possible?
The more characters in the code, the more specific the diagnosis, so when writing a code on a medical record you should give the longest code possible while retaining accuracy.
Overview
- Parenteral feeding refers to the implantation of a small, thin tube (catheter) into a vein so that nutrients and fluids can be delivered directly into the bloodstream.
- Gastroparesis is a condition that affects the normal spontaneous movement of the muscles (motility) in your stomach. Ordinarily, strong muscular contractions propel food through your digestive tract. But if you have gastroparesis, your stomach's motility is slowed down or doesn't work at all, preventing your stomach from emptying properly.Certain medications, such as opioi…
- A gastric neurostimulator is a surgically implanted battery-operated device that releases mild electrical pulses to help control nausea and vomiting associated with gastroparesis. This option is available to people whose nausea and vomiting do not improve with medications. Further studies will help determine who will benefit most from this procedure, which is available in a fe…
Diagnosis
- So far, there is no consensus on how to classify histopathological findings. A diagnosis of gastroparesis is made based upon a thorough clinical evaluation, a detailed patient history, and a variety of specialized tests. Tests may first be performed to rule out other causes of delayed gastric emptying such as obstruction of the gastrointestinal tract. Additional tests are then perf…
- Doctors use several tests to help diagnose gastroparesis and rule out conditions that may cause similar symptoms. Tests may include: 1. Gastric emptying study. This is the most important test used in making a diagnosis of gastroparesis. It involves eating a light meal, such as eggs and toast, that contains a small amount of radioactive material. A scanner that detects the moveme…
- After performing a full physical exam and taking your medical history, your doctor may order several blood tests to check blood counts and chemical and electrolyte levels. To rule out an obstruction or other conditions, the doctor may perform the following tests: Once other causes have been ruled out, the doctor will perform one of the following gastric emptying tests to confir…
- Gastroparesis is diagnosed by assessing the movement of food through the stomach. This may be done with investigations like a gastric emptying study where a small amount of radiocontrast dye is ingested with food. The movement of this food can then be monitored with a scanner that tracks the radioactive material. Other methods to track the movement through the gut and highli…
Signs And Symptoms
- The digestive symptom profile of nausea, vomiting, abdominal pain, reflux, bloating, a feeling of fullness after a few bites of food (early satiety), and anorexia can vary in patients both in combination and severity. A small percentage of patients who live with poorly managed symptoms despite numerous treatment interventions, and an inability to meet their nutritional n…
- Signs and symptoms of gastroparesis include: 1. Vomiting 2. Nausea 3. A feeling of fullness after eating just a few bites 4. Vomiting undigested food eaten a few hours earlier 5. Acid reflux 6. Abdominal bloating 7. Abdominal pain 8. Changes in blood sugar levels 9. Lack of appetite 10. Weight loss and malnutritionMany people with gastroparesis don't have any noticeable signs an…
- Gastroparesis is a disorder in which the stomach takes too long to empty its contents. Normally, the stomach has regular contractions to move food down into the small intestine for digestion. Gastroparesis results from damage to the vagus nerve that controls this movement. When the nervous system is compromised, the muscles of the stomach and intestines dont work normally…
Treatment
- Treatment Treating the underlying cause of gastroparesis (such as tightening up blood glucose control in diabetes) is usually the first step in treating individuals with gastroparesis. The specific therapeutic techniques used depend upon several factors, including the severity of the disorder. Therapies that are used to treat individuals with gastroparesis include non-pharmacological ste…
- Treating gastroparesis begins with identifying and treating the underlying condition. If diabetes is causing your gastroparesis, your doctor can work with you to help you control it.
- I discussed your question with Gerard Mullin, M.D., associate professor of medicine and an integrative gastroenterologist at Johns Hopkins Hospital. He told me that acupuncture and electroacupuncture have been shown in randomized trials to be effective for gastroparesis, and that a study published in the European Journal of Gastroenterology & Hepatology in May, 2008, f…
- Treatment of gastroparesis depends on the severity of the symptoms. In most cases, treatment does not cure gastroparesis-it is usually a chronic condition. Treatment helps you manage the condition so you can be as healthy and comfortable as possible. Several medications are used to treat gastroparesis. Your doctor may try different medications or combinations to find the most …
Causes
- The etiologies (causes) for gastroparesis are extensive and varied. Reports from one tertiary referral center found that out of their 146 patients with gastroparesis: 36% were idiopathic (unknown causes), 29% were diabetic, 13% were post-surgical, 7.5% had Parkinsons disease and 4.8% had collagen diseases. Any disease of metabolic, neurological (psychiatric, brainstem, aut…
- It's not always clear what leads to gastroparesis. But in many cases, gastroparesis is believed to be caused by damage to a nerve that controls the stomach muscles (vagus nerve).The vagus nerve helps manage the complex processes in your digestive tract, including signaling the muscles in your stomach to contract and push food into the small intestine. A damaged vagus n…
- The most common cause of gastroparesis is diabetes. Here, high blood sugar affects the health of nerves throughout the body and can damage the vagus nerve. Other causes include surgery on the stomach, viral infections, eating disorders (anorexia nervosa or bulimia), medications that slow contractions in the intestine, and gastroesophageal reflux disease (GERD).
- Normally, the vagus nerve in the stomach controls muscle contractility and peristalsis of food into the small intestine. In patients with gastroparesis, this nerve is believed to be damaged, leading to decreased signaling of stomach muscles, yielding a slowed emptying time and perhaps abnormal digestion. This condition may be idiopathic in nature, but is commonly seen in patients with diab…
Diet
- Dietary changes include eating five to six small meals each day and avoiding high-insoluble fiber and high-fat foods, both of which can slow down stomach emptying. Lactose intolerance is common in gastroparesis, so avoidance of dairy is helpful, but fermented milk (yogurt) is fine. Some individuals do better with liquid or pureed foods while avoiding difficult-to-digest solid foo…
- Eating solid foods, high-fiber foods such as raw fruits and vegetables, fatty foods, or drinks high in fat or carbonation may contribute to these symptoms.
Pathophysiology
- Gastroparesis has been documented to occur as a sequel to viral gastroenteritis, slowly resolving over one to two years. However, any upper-gut infection of bacterial, parasitic or viral origin has the potential to disrupt, for prolonged periods of time, gastric motility. In gastroparesis patients, and others with unexplained chronic nausea and vomiting, one recent study reported up to 80% …
- Gastroparesis literally means stomach (gastro-) paralysis (paresis). It is a partial rather than complete paralysis. The vagus nerve which is a cranial nerve (CN X), meaning that it emanates directly from the brain, supplies the muscles in the stomach. With parasympathetic stimulation by impulses via the vagus nerve, the movement within the stomach (peristalsis) increases and the …
- Normal gastric emptying is due to a complex interaction between various regions of the stomach and duodenum. These include a coordinated series of events starting with fundic accommodation of ingested food, antral contractions, pyloric relaxation, and antroduodenal coordination.[1] Interruption of this pathway may lead to altered gastric empting and subsequent disease or sym…
Prognosis
- The use of GES in diabetics has a high rate of success for reducing symptoms of nausea and vomiting. However, success in the idiopathic patients is less predictable. Therefore, following the clinical practice for other neurostimulating devices (examples: spinal cord stimulation, sacral nerve stimulation, deep brain stimulation) whereby a short-term trial of stimulation is used to hel…
- Conclusion: We conclude that post-infectious gastroparesis is an uncommon and often over looked condition. It is self-limiting in most cases. EGG is pathological in most patients.
Management
- Abdominal pain is best managed by a pain specialty clinic where a selection of analgesics with the least impact on slowing the GI tract can be made. Other clinical management issues to consider are metabolic bone disease (all gastroparetic patients are at risk) and routine monitoring for small bowel bacterial overgrowth (SBBO). SBBO commonly occurs in gastroparesis and may …
- Following the diagnosis of gastroparesis, clinicians must determine the degree of symptomatology in order to formulate an appropriate treatment plan. Mild gastroparesis may be managed by proper nutrition and weight maintenance, while moderate to severe symptoms may require medication therapy in addition to dietary and lifestyle modifications. In refractory patient…
Complications
- Gastroparesis can cause several complications, such as: 1. Severe dehydration. Ongoing vomiting can cause dehydration. 2. Malnutrition. Poor appetite can mean you don't take in enough calories, or you may be unable to absorb enough nutrients due to vomiting. 3. Undigested food that hardens and remains in your stomach. Undigested food in your stomach can harden into a solid …
Popular Posts:
- 1. icd 10 code for microangiopathic hemolytic anemia
- 2. icd 10 dx code for fall syncope unspecified
- 3. icd 10 code for left displaced femoral neck fracture
- 4. billable icd 10 code for asthma
- 5. icd 10 cm code for for upper lid swelling
- 6. icd 10 code for ckd-3
- 7. icd 10 code for hx of cerebral aneurysm
- 8. icd 10 code for left big toe pain
- 9. icd code 10 for high cholesterol
- 10. icd 10 code for std screening cotact