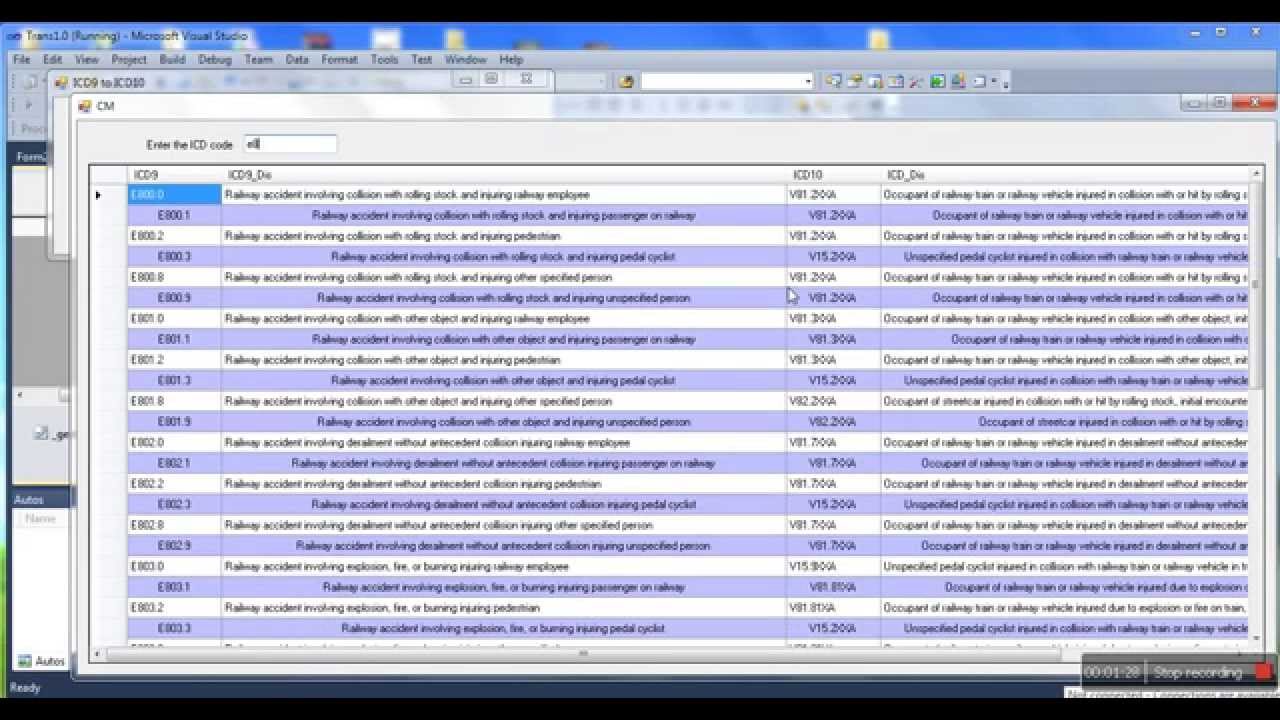
ER claims are defined as claims with CPT codes 99281, 99282, 99283, 99284, and 99285. ICD -9 and ICD -10 standard codes are reported. If multiple diagnostic codes are attached to a claim, primary diagnosis is used.
Full Answer
What is the ICD 10 code for emergency visit?
Emergency Visit Claims by Diagnosis Code and Recipient Age Group. ER claims are defined as claims with CPT codes 99281, 99282, 99283, 99284, and 99285. ICD -9 and ICD -10 standard codes are reported. If multiple diagnostic codes are attached to a claim, primary diagnosis is used. Providers are billing providers.
What is the ICD 10 code for encounter exam?
Encounter for administrative examinations, unspecified. Z02.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
Do you code for suspected diagnosis?
What those guidelines say is if you’re coding for the hospital outpatient department, you do not code for any diagnoses that is documented as “probable,” “suspected,” “questionable,” “rule out,” or “working diagnosis” or anything else that indicate uncertainty; so no “probable,” “likely,” “suspected,” anything like that.
What is diagnostic coding and report Guidelines for outpatient service?
Those are the guidelines for Diagnostic Coding and Report Guidelines for Outpatient Service. According to that, most facilities – just to give you an idea of what happens in most facilities – if a patient presents to the emergency room, those emergency room charges are entered into the system.

What is the ICD code for ER visit?
ER claims are defined as claims with CPT codes 99281, 99282, 99283, 99284, and 99285. ICD -9 and ICD -10 standard codes are reported.
What is the revenue code for emergency room?
0450-0459Claims in the Outpatient and Inpatient files are identified via Revenue Center Code values of 0450-0459 (Emergency room) or 0981 (Professional fees-Emergency room).
What does code 99284 mean?
Emergency department visit 99284 is used for the evaluation and management of a patient, which requires the following 3 components: A detailed history; A detailed examination ;and. Medical decision making of moderate complexity.
Can 99284 and 99285 be billed together?
E&M codes 99284 and 99285 are not reimbursable together or more than once to the same provider, for the same recipient and date of service. Instead, providers should use code 99283 to bill for second and subsequent recipient visits on the same date of service.
What is a Level 3 ER visit?
Level 3 - Urgent, not life-threatening (Example: patient has severe abdominal pain) Level 4 - Semi-urgent, not life-threatening (Example: patient with earache or minor cut requiring sutures) Level 5 - Non-urgent, needs treatment when time permits (Example: patient with minor symptoms or needing a prescription renewal)
What is the difference between 99283 and 99284?
If the patient has to go through any heart exam like CT heart, MRI chest, Ultrasound chest, then the ED level changes to code 99284, level 4. In ED level visit CPT code 99283, the patient will have a moderate severity problem. In some scenarios the patient may have to undergo some surgery procedures as well.
What is Level 4 ED visit?
Level 4 – A severe problem that requires urgent evaluation, but doesn't pose a threat to life or to physical function; without treatment there is a high chance of extreme impairment.
What is a Level 4 dr visit?
Level 4 Established Office Visit (99214) This code represents the second highest level of care for established office patients. This is the most frequently used code for these encounters. Internists selected this level of care for 55.38% of established office patients in 2019.
What is a Level 4 patient visit?
That means that for an outpatient E/M office visit to be coded as a level 4 (for new or established patients), you need at least two of the three elements to reach the “moderate” category — moderate number and complexity of problems addressed; moderate amount and/or complexity of data to be reviewed and analyzed; or ...
Does CPT 99284 require a modifier?
yes you will need a 25 modifier on the E&M any time there is a status S or T procedure performed in any session of the day. So if you have a 510 99213 and a 450 99284 with the 450 99372 on the same date of service then both E&Ms will need a 25 modifier.
When should I use 99285?
Per CPT definition, the codes 99281-99285 are for reporting evaluation and management services in the emergency department. An emergency department is defined as an organized hospital-based facility for the provision of unscheduled episodic services to patients who present for immediate medical attention.
Is 99285 An E&M code?
Emergency Department (ED) Evaluation and Management (E/M) codes are typically reported per day and do not differentiate between new or established patients. There are 5 levels of emergency department services represented by CPT codes 99281 – 99285.
What is the ICD-10 manual for outpatient services?
Those are the guidelines for Diagnostic Coding and Report Guidelines for Outpatient Service. According to that, most facilities – just to give you an idea of what happens in most facilities – if a patient presents to the emergency room, ...
Can you code for a probable diagnosis?
What those guidelines say is if you’re coding for the hospital outpatient department, you do not code for any diagnoses that is documented as “probable,” “suspected,” “questionable,” “rule out,” or “working diagnosis” or anything else that indicate uncertainty; so no “probable,” “likely,” “suspected,” anything like that.
What happens if secondary diagnoses are not reported?
If secondary diagnoses are not reported, then HCC’s are not captured for the claim. This may impact reimbursement and quality measure statistics. Below are several websites that are available and that go into great detail about what HCC’s are, how they are calculated, and why they are important.
When should chronic conditions be reported?
Chronic conditions should be reported on each visit when they are under treatment or are systemic medical conditions. Chronic systemic conditions should be reported even in the absence of intervention or further evaluation.
What is the final impression by the physician?
The final impression by the physician is COPD exacerbation. In this case, a code for the COPD exacerbation would be reported as well as “Z” codes for personal history of pneumonia, history of smoking, and family history of lung cancer and colon cancer.
Why do you report secondary diagnosis?
Another reason to report all secondary diagnosis, history and status codes is to confirm medical necessity. Some payors will deny tests done outpatient if the medical necessity is not met. Many times medical necessity is determined by the ICD-10-CM codes reported on the outpatient claim. For example, if an EKG is done on a patient in an encounter for outpatient fracture repair, and the chronic atrial fibrillation is not coded as a secondary diagnosis by the coder, the EKG charge/reimbursement could be denied by the payor. There are also many other examples, such as a patient getting extended laboratory tests because they are on long term anticoagulants such as Coumadin. It is very important that all secondary diagnosis/status/history codes be reported on the outpatient claim.
Can't describe HCC?
If you can’t describe what HCC’s are, it is recommended that you review some of the websites above and become familiar with these. If you know the why things are reported it is easier to remember to report them. Coders must review the entire outpatient encounter rather than only focusing on the reason for the visit.
Can a code be reported on a radiology report?
Coders may report confirmed diagnoses on radiology and pathology reports (except for incidental findings) “Z” codes help paint the entire health picture for the patient. If there is a specific code for a past or family condition, it will most likely always be reported. Code only confirmed diagnosis on outpatient encounters.
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
What does "type 1 excludes note" mean?
A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition. aftercare following medical care (.
What is the S96.012A?
10. S96.012A. Strain of muscle and tendon of long flexor muscle of toe at ankle and foot level, left foot, initial encounter .
What is the meaning of "s96.119s"?
10. S96.119S. Strain of muscle and tendon of long extensor muscle of toe at ankle and foot level, unspecified foot, sequela.
Can you play training games with ICD-9 codes?
You can play training games using common ICD-9/10 codes for Emergency Medicine! When you do, you can compete against other players for the high score for each game. As you progress, you'll unlock more difficult levels! Play games like...
Popular Posts:
- 1. icd 10 procedure code for pomeroy tubal ligation
- 2. icd 10 code for c1 anterior arch fracture
- 3. icd 10 code for lchf
- 4. icd 10 code for right knee medial plica
- 5. icd 10 code for abnormal radiologic in pelvis
- 6. icd 10 code for prehypertension
- 7. icd 10 code for carotid atherosclerosis
- 8. icd 10 code for left diabetic foot wound
- 9. icd 10 external cause code for fall from ladder
- 10. what is the icd 10 code for paroxysmal nocturnal dyspnea