Exocrine pancreatic insufficiency. K86.81 is a valid billable ICD-10 diagnosis code for Exocrine pancreatic insufficiency. It is found in the 2019 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2018 - Sep 30, 2019.
Why is epi hard to diagnose?
• The symptoms of EPI can be a lot like other medical conditions that affect the stomach and bowels.1-4,7-11This can sometimes make EPI hard to diagnose. That’s why it’s important to be open and honest with your doctor about all of your stomach and bowel problems • Tell your doctor about:
How is exocrine pancreatic insufficiency (EPI) diagnosed?
You should remember to share the following information with your doctor:
- Any conditions you’ve been diagnosed with
- Your eating habits
- Any and all symptoms you’ve been experiencing and the severity of your symptoms
- When your symptoms started
- If you've had unexplained weight loss
- Any differences in your stools and bowel movements
- Any medications or herbals you may be taking
What diseases are caused by pancreas?
What causes pancreatitis?
- infections, such as viruses or parasites NIH external link
- injury to your abdomen
- pancreatic cancer NIH external link
- having a procedure called endoscopic retrograde cholangiopancreatography (ERCP) to treat another condition
- pancreas divisum NIH external link
What causes pancreas pain?
Pancreatitis is an inflammation of the pancreas ... If you have pleuritis, the layers rub against one another and cause pain. It also can cause shortness of breath and a cough.
What is the ICD-10 code for exocrine pancreatic insufficiency?
ICD-10 code K86. 81 for Exocrine pancreatic insufficiency is a medical classification as listed by WHO under the range - Diseases of the digestive system .
Is pancreatitis the same as pancreatic insufficiency?
Pancreatitis, cystic fibrosis and other conditions that affect the pancreas cause exocrine pancreatic insufficiency (EPI). People with EPI don't have enough pancreatic (digestive) enzymes to break down foods and absorb nutrients. It can lead to malnutrition. Pancreatic enzyme replacement therapy (PERT) can help.
Is exocrine pancreatic insufficiency an autoimmune disease?
Autoimmune pancreatitis can cause a variety of complications. Pancreatic exocrine insufficiency. AIP may affect the ability of your pancreas to make enough enzymes. Signs and symptoms may include diarrhea, weight loss, metabolic bone disease, and vitamin or mineral deficiency.
What is ICD-10 code for pancreatic duct stricture?
Congenital stenosis and stricture of bile ducts The 2022 edition of ICD-10-CM Q44. 3 became effective on October 1, 2021. This is the American ICD-10-CM version of Q44.
What does pancreatic insufficiency mean?
Pancreatic Insufficiency (EPI) is a condition which occurs when the pancreas does not make enough of a specific enzyme the body uses to digest food in the small intestine. The pancreas is a glandular organ. That means the pancreas secretes juices that maintain the proper function of the body.
What is the difference between EPI and IBS?
People with IBS will see mucus in their stool, says Dr. Anderson, rather than fat. (Fatty stools, or steatorrhea, are a telltale sign of EPI.) Like those of EPI, IBS symptoms tend to occur after eating, but IBS may also be triggered by stress, infection, and other factors.
What is the ICD 10 code for pancreatic lesion?
K86. 2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM K86.
Is the pancreatic duct a bile duct?
Biliary and Pancreatic Ducts The small tubes that carry bile between the liver, gallbladder and small intestine are called biliary or bile ducts. The pancreatic duct connects the pancreas to the common bile duct.
What is the ICD 10 code for fatty atrophy of the pancreas?
K86. 89 - Other specified diseases of pancreas | ICD-10-CM.
Self-Checks and At-Home Testing
There are no in-home tests or self-exams able to diagnose EPI. 2 However, knowing the signs and symptoms of EPI—and how to communicate them to your healthcare provider—can increase your chance of a correct diagnosis.
Diagnostic Questions
A diagnosis of EPI is made after other, more common causes of gastrointestinal symptoms have been ruled out, such as Crohn's disease or chronic gastritis. If your healthcare provider suspects you could have EPI, you may be asked questions and undergo tests to confirm a proper diagnosis. Topics may include: 3
Labs and Tests
Common tests that your healthcare provider may perform to determine EPI include: 4
Imaging
If you have EPI, your doctor may order computerized tomography scans (CT scans), ultrasounds, and magnetic resonance imaging (MRI) to see inside your abdomen and assess whether your pancreas is visibly damaged, obstructed, or inflamed.
Summary
Knowing the signs and symptoms of EPI—and how to communicate them to your healthcare provider—can increase your chance of getting a correct diagnosis.
A Word From Verywell
While EPI is considered rare in the general population, it may also be underdiagnosed, as mild forms of EPI may not warrant an immediate visit to see a doctor. Among those who do seek treatment, they may not be correctly diagnosed with EPI until the condition has become more advanced.
What is the test for exocrine pancreatic function?
Exocrine pancreatic function can be measured by so-called direct pancreatic function tests . In these tests, pancreatic secretion is stimulated by secretin and/or cerulein[45] or by the ingestion of a standard test meal[46].
How many lipase units are needed for pancreatic enzyme replacement?
The dose should be in proportion to the fat content of the meal, usually 40-50000 lipase units per main meal, and half the dose is required for a snack.
What is the role of pancreatic juice?
The pancreatic juice plays a pivotal role in the digestion and absorption of nutrients [5]. Pancreatic enzyme secretion is stimulated during the cephalic[6] and gastric[7] phases to a certain degree, but the most important stimulation occurs during the intestinal phase, when chyme enters the duodenum.
Does smoking cause pancreatitis?
Smoking is a risk factor for pancreatic cancer, acute pancreatitis and CP[53], and is also associated with an increased probability of reduced pancreatic exocrine function based on the endoscopic pancreatic function test in cases with CP[54].

Self-Checks and At-Home Testing
- There are no in-home tests or self-exams able to diagnose EPI.2However, knowing the signs and symptoms of EPI—and how to communicate them to your healthcare provider—can increase your chance of a correct diagnosis.
Diagnostic Questions
- A diagnosis of EPI is made after other, more common causes of gastrointestinal symptoms have been ruled out, such as Crohn's disease or chronic gastritis. If your healthcare provider suspects you could have EPI, you may be asked questions and undergo tests to confirm a proper diagnosis. Topics may include:3 1. Your symptoms: This includes how long you've had them, and if there is …
Labs and Tests
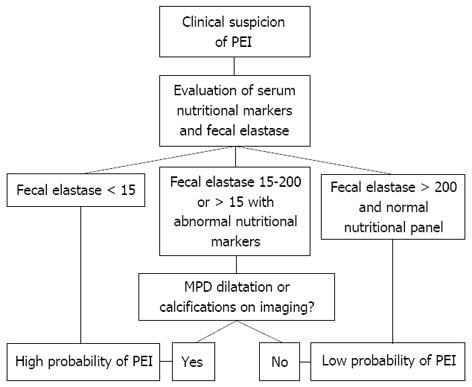
- Common tests that your healthcare provider may perform to determine EPI include:4 1. Fecal elastase test (FE-1): This test is done to look for an enzyme called elastase that is released from the pancreas during digestion.3Normally, this enzyme will be found in stool. If little or none is found, it can be a sign of EPI. For this test, you will be as...
Imaging
- If you have EPI, your doctor may order computerized tomography scans (CT scans), ultrasounds, and magnetic resonance imaging (MRI) to see inside your abdomen and assess whether your pancreas is visibly damaged, obstructed, or inflamed.2While there are a few highly specialized diagnostic imaging tests that can assess pancreatic function, these tests are mostly used to rul…
Summary
- Knowing the signs and symptoms of EPI—and how to communicate them to your healthcare provider—can increase your chance of getting a correct diagnosis. A diagnosis of EPI is usually made by a gastroenterologist after more common causes of gastrointestinal symptoms have been ruled out, such as Crohn's disease or chronic gastritis. Several diagnostic tests, including f…
A Word from Verywell
- While EPI is considered rare in the general population, it may also be underdiagnosed, as mild forms of EPI may not warrant an immediate visit to see a doctor. Among those who do seek treatment, they may not be correctly diagnosed with EPI until the condition has become more advanced. It is important that you see your healthcare provider if you have any symptoms relate…
Popular Posts:
- 1. icd 10 code for parkinson's dementia without behavioral disturbance
- 2. icd-10-cm code for pcos
- 3. icd 10 code for bilateral shoulder replacement
- 4. icd 10 code genital exam for penile sores
- 5. 2019 icd 10 code for over overexertion
- 6. icd 10 code for corneal abrasion left eye
- 7. icd 10 code for fissured tongue
- 8. 2017 icd 10 code for group
- 9. icd 10 code for fall with left knee contusion
- 10. icd 10 code for m47.812