What are the signs and symptoms of acute respiratory failure?
What are the signs and symptoms of Respiratory Failure?
- Difficulty breathing
- Rapid breathing
- Bluish colored skin, lips and fingernails (called cyanosis)
- Confusion
What is chronic hypoxemic respiratory failure?
In chronic respiratory failure, hypoxemia can be caused by one or more of the following basic mechanisms: Ventilation-perfusion mismatch is mismatched distribution of ventilation and perfusion, with some lung units receiving disproportionately high ventilation and others receiving disproportionately high perfusion.
What is acute respiratory failure with hypoxia?
Symptoms and Signs of Acute Hypoxemic Respiratory Failure Acute hypoxemia (see also Oxygen Desaturation ) may cause dyspnea, restlessness, and anxiety. Signs include confusion or alteration of consciousness, cyanosis, tachypnea, tachycardia, and diaphoresis. Cardiac arrhythmia and coma can result.
What causes chronic respiratory failure?
You might have a higher risk of respiratory failure if you:
- Have long-term respiratory problems like COPD or asthma
- Smoke
- Drink a lot of alcohol
- Have a family history of respiratory problems

What is the ICD-10 code for hypoxic respiratory failure?
ICD-10 Code for Acute respiratory failure with hypoxia- J96. 01- Codify by AAPC.
What is the ICD-9 code for hypoxia?
799.02Until now, the ICD-9 code for hypoxia was 799.0. That has changed to the following two new codes, which provide a higher level of specificity: 799.01: asphyxia. 799.02: hypoxemia.
What is the ICD-10 code for acute hypoxemia?
ICD-10-CM Code for Hypoxemia R09. 02.
What does acute hypoxic respiratory failure mean?
Hypoxemic respiratory failure means that you don't have enough oxygen in your blood, but your levels of carbon dioxide are close to normal.
Is hypoxia same as hypoxemia?
Hypoxemia (low oxygen in your blood) can cause hypoxia (low oxygen in your tissues) when your blood doesn't carry enough oxygen to your tissues to meet your body's needs. The word hypoxia is sometimes used to describe both problems.
What is the diagnosis for ICD 10 code r50 9?
9: Fever, unspecified.
How do you code hypoxia?
00 with hypercapnia code J96. 02 and hypoxia code J96. 01.
What is the ICD-10 code for acute on Chronic respiratory failure with hypoxia?
ICD-10 Code for Acute and chronic respiratory failure with hypoxia- J96. 21- Codify by AAPC.
How do you code Acute respiratory failure with hypoxia and hypercapnia?
J96.00 – Acute respiratory failure, unspecified whether with hypoxia or hypercapnia.J96.01 – Acute respiratory failure, with hypoxia.J96.02 – Acute respiratory failure, with hypercapnia.
Is acute hypoxic respiratory failure the same as ARDS?
Acute respiratory distress syndrome (ARDS) is a form of acute-onset hypoxemic respiratory failure caused by acute inflammatory edema of the lungs and not primarily due to left heart failure.
How is acute hypoxemic respiratory failure diagnosed?
One needs to document two of the three criteria to formally diagnose acute respiratory failure: pO2 less than 60 mm Hg (or room air oxygen saturation less than or equal to 90%), pCO2 greater than 50 mm Hg with pH less than 7.35, and signs/symptoms of respiratory distress.
What is the difference between respiratory distress and respiratory failure?
Respiratory distress happens when a person is unable to regulate gas exchange, causing them to either take in too little oxygen or expel too little carbon dioxide. Respiratory failure can follow respiratory distress, and causes more severe difficulties with gas exchange. Left untreated, it may be fatal.
What is the most common cause of hypoxemia?
Hypoxemia has many causes, but its most common cause is an underlying illness that affects blood flow or breathing (like heart or lung conditions). Certain medications can slow breathing and lead to hypoxemia.
What is nocturnal hypoxemia?
Nocturnal hypoxemia was defined as more than 10% of total sleep time below a SpO2 of 90% (Deflandre et al., 2018).
What is the pO2 level for hypoxemia?
The diagnostic criteria for hypoxemia would be a partial pressure of oxygen (pO2) level less than 60 millimeters of mercury (mmHg) (oxygen saturation of less than 91%) on room air, or pO2/fraction of inspired oxygen (P/F) ratio (pO2/FIO2) less than 300 (not used for patients with chronic respiratory failure on continuous home oxygen) or 10 mmHg increase in baseline pO2 (if known baseline, this is why baseline information on patients if available is so important).
What is respiratory failure?
It is defined as abnormal arterial oxygenation and/or carbon dioxide accumulation, signs and symptoms can range from shortness of breath, dyspnea, tachycardia, respiratory rate greater than 20 cyanosis or labored breathing, just to name a few.
What is the pH of hypercapnic blood gas?
Hypercapnic diagnostic criteria would be pCO2 >50 mmHg with pH <7.35, or 10 mmHg increase in baseline pCO2 (again if known). Although not required, you can see why arterial blood gas results can be extremely helpful when dealing with the differentiation of hypoxemic versus hypercapnic respiratory failure.
Is J96 a DRG?
Now, when you turn to the DRG Expert you will find both of these codes bring us to the same DRG which is found in MDC 4 Diseases and Disorders of the Respiratory System. You may see the code J96* Respiratory failure, not elsewhere classified (NEC). The asterisk lets us know that there is a range of codes that would be found under this one code, but because this is not a code book, not all are listed individually.
What is acute hypoxemia?
Acute hypoxemic respiratory failure is severe arterial hypoxemia that is refractory to supplemental oxygen. It is caused by intrapulmonary shunting of blood resulting from airspace filling or collapse (eg, pulmonary edema due to left ventricular failure, acute respiratory distress syndrome) or by intracardiac shunting of blood from ...
How to diagnose hypoxemia?
Hypoxemia is usually first recognized using pulse oximetry. Patients with low oxygen saturation should have a chest x-ray and ABGs and be treated with supplemental oxygen while awaiting test results.
What is the maximum pressure support level for PEEP?
Typically, a pressure support level of 10 to 20 cm H2O over PEEP is required.
What causes ARDS in the lung?
Causes of ARDS may involve direct or indirect lung injury.
How much oxygen is needed for AHRF?
Underlying conditions must be addressed as discussed elsewhere. AHRF is initially treated with high flows of 70 to 100% oxygen by a nonrebreather face mask. If oxygen saturation > 90% is not obtained, mechanical ventilation probably should be instituted. Specific management varies by condition.
How high is the mortality rate in ARDS?
Overall, mortality in ARDS was very high (40 to 60%) but has declined in recent years to 25 to 40%, probably because of improvements in mechanical ventilation and in treatment of sepsis. However, mortality remains very high (> 40%) for patients with severe ARDS (ie, those with a PaO2:FIO2 < 100 mm Hg). Most often, death is not caused by respiratory dysfunction but by sepsis and multiorgan failure. Persistence of neutrophils and high cytokine levels in bronchoalveolar lavage fluid predict a poor prognosis. Mortality otherwise increases with age, presence of sepsis, and severity of preexisting organ insufficiency or coexisting organ dysfunction.
What pH is good for ventilator-associated lung injury?
On occasion, however, respiratory acidosis develops, some degree of which is accepted for the greater good of limiting ventilator-associated lung injury and is generally well tolerated, particularly when pH is ≥ 7.15. If pH drops below 7.15, bicarbonate infusion or tromethamine may be helpful.
Known As
Respiratory failure is also known as acute hypercapnic respiratory failure, acute hypercapnic respiratory failure due to obstructive sleep apnea, acute hypercarbic respiratory failure secondary to obstuctive sleep apnea, acute hypoxemic respiratory failure, acute respiratory failure from obstuctive sleep apnea, alveolar hypoventilation, hypercapnic respiratory failure, hypoxemic respiratory failure, postprocedural respiratory failure,and respiratory failure.
Respiratory Failure Definition and Symptoms
Respiratory failure is when there is an inadequate gas exchange from the respiratory system, which causes oxygen and carbon dioxide levels to go out of their normal ranges. Symptoms include being very sleepy, arrhythmias, sepsis, and a bluish color of the skin or lips.
When is acute respiratory failure a principal diagnosis?
OFFICIAL CODING GUIDELINE Acute or acute on chronic respiratory failure may be reported as principal diagnosis when it is the condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care. Refer to Section II of the ICD-10-CM Official Guidelines for Coding and Reporting on “Selection of Principal Diagnosis”.
What to do if documentation is not clear as to whether acute respiratory failure and another condition are equally responsible for occasioning?
If the documentation is not clear as to whether Acute Respiratory Failure and another condition are equally responsible for occasioning the admission, query the provider for clarification.
What are the symptoms of respiratory failure?
Look for documented signs / symptoms of: SOB (shortness of breath) Delirium and/or anxiety. Syncope. Use of accessory muscles / poor air movement.
Is respiratory failure a cut and dry diagnosis?
Very seldom is it a simple cut and dry diagnosis. There always seems to be just enough gray to give coders on any given day some doubt. It’s not only important for a coder to be familiar with the guidelines associated with respiratory failure but they should also be aware of the basic clinical indicators as well.
Does a condition on admission qualify for principal diagnosis?
With any record, keep in mind that because a condition may be present on admission does not necessarily mean it qualifies for principal diagnosis. You have to ask yourself these questions:
Can COPD cause ABG?
A patient with a chronic lung disease such as COPD may have an abnormal ABG level that could actually be considered that particular patient’s baseline.
Why is acute respiratory failure not validated?
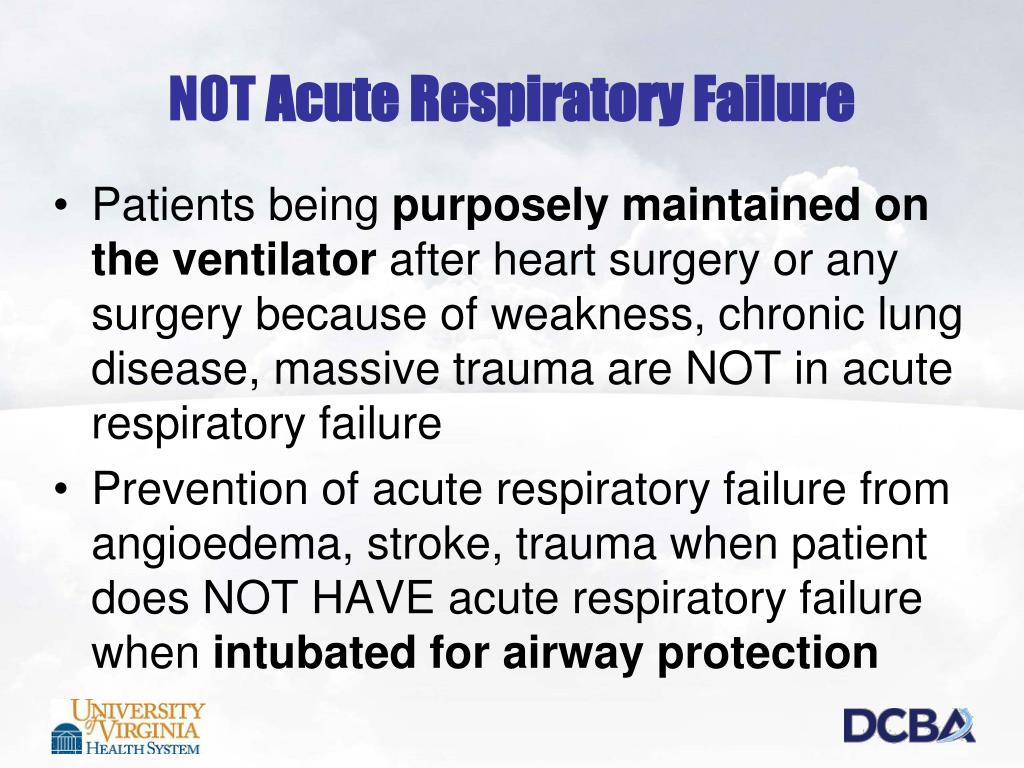
Acute respiratory failure with hypoxia is not validated and has been removed as a diagnosis code assignment consistent with documentation received, for the following reasons: No need for assistive ventilation devices such as bi-level positive airway pressure support or mechanical ventilation.
Does respiratory failure show up on a record review?
Based on your own findings, it appears that your record review supports the diagnosis of respiratory failure, although if no signs of distress ( e.g., respiratory rate greater than 20, shortness of breath, tripod breathing, speaking in short sentences, signs of cyan osis such as loss of color in the nailbeds and lips, confusion, use of accessory muscles, etc.) the diagnosis may not be supported.
Is ABG necessary for acute respiratory failure?
First of all, an ABG is not necessary for the diagnosis of acute respiratory failure, supplemental oxygen is the primary treatment for respiratory failure, and assistive ventilatory devices such as BiPAP or mechanical ventilation are not required to establish the diagnosis. According to the 2018 CDI Pocket Guide:
Popular Posts:
- 1. icd 10 code for shingles polyneuropathy
- 2. 2019 icd 10 code for centrilobular emphysema cerebral
- 3. icd 10 code for exposure to drugs in utero
- 4. icd 10 code for contact with table saw
- 5. icd 9 code for cervical spine muscle spasm
- 6. icd 10 code for post op surgical wound infection
- 7. icd 10 code for history of septic shock with acute renal failure
- 8. icd 10 code for influenza a
- 9. icd 10 cm code for elevated potassium
- 10. icd 10 code for throombocy