Peripheral neuropathy with diabetes should be coded as E11.42 (DM with polyneuropath), not e11.40 (DM with neuropathy). Coder needs to check signs and symptoms in the medical record, also, check the underlying cause if anything mentioned. Neuropathic pain should be coded as neuralgia M79.2, not neuropathy.
What is diagnosis code 10?
- Similar to the diagnosis code set, the alpha characters in ICD 10 code sets are not case-sensitive.
- The letters “O” and “I” are not in the code set. ...
- The 7 characters in the procedure code set help in providing very precise details. ...
- The fourth character identifies the part of the body. ...
What is diagnosis code DM?
Diabetes mellitus. There are 10 ICD-9-CM codes below 250 that define this diagnosis in greater detail. Do not use this code on a reimbursement claim. (dye-a-bee-teez) a disease in which the body does not properly control the amount of sugar in the blood. As a result, the level of sugar in the blood is too high.
Which treatment can improve diabetic nephropathy?
- Blood pressure control. Medications called angiotensin-converting enzyme (ACE) inhibitors and angiotensin 2 receptor blockers (ARBs) are used to treat high blood pressure.
- Blood sugar control. Medications can help control high blood sugar in people with diabetic nephropathy. ...
- High cholesterol. ...
- Kidney scarring. ...
What is the earliest sign of diabetic nephropathy?
They may include:
- Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema)
- A rise in potassium levels in your blood (hyperkalemia)
- Heart and blood vessel disease (cardiovascular disease), which could lead to stroke
What is the ICD-10 code for DM with nephropathy?
ICD-10 Code for Type 2 diabetes mellitus with diabetic nephropathy- E11. 21- Codify by AAPC.
What is nephropathy in diabetes mellitus?
Diabetic nephropathy is a common complication of type 1 and type 2 diabetes. Over time, poorly controlled diabetes can cause damage to blood vessel clusters in your kidneys that filter waste from your blood. This can lead to kidney damage and cause high blood pressure.
Is diabetic nephropathy the same as kidney failure?
What is diabetic nephropathy? Nephropathy is the deterioration of kidney function. The final stage of nephropathy is called kidney failure, end-stage renal disease, or ESRD. According to the CDC, diabetes is the most common cause of ESRD.
Is diabetic nephropathy the same as diabetic glomerulosclerosis?
Diabetic nephropathy is a common cause of end‐stage renal disease worldwide. It is characterised by diffuse or nodular glomerulosclerosis, afferent and efferent hyaline arteriolosclerosis, and tubulointerstitial fibrosis and atrophy.
What is the ICD 10 code for nephropathy?
Nephropathy induced by unspecified drug, medicament or biological substance. N14. 2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM N14.
How is diabetic nephropathy diagnosis?
Kidney biopsy The biopsy needle is inserted through your skin and is often directed using the guidance of an imaging device, such as ultrasound. Diabetic nephropathy is usually diagnosed during routine testing that's a part of your diabetes management.
What is Microalbuminuric diabetic nephropathy?
Microalbuminuria refers to a higher-than-normal amount of albumin in the urine. A high value of this urinary protein may indicate a problem with the kidneys. As people with diabetes have an increased risk of kidney complications, a doctor may request a microalbuminuria test to help detect early signs of kidney disease.
What is the meaning of nephropathy?
kidney diseaseNephropathy is a medical term for kidney disease. The type of kidney disease caused by diabetes is called diabetic nephropathy.
What is incipient diabetic nephropathy?
Diagnosis of Diabetes with Renal Manifestations Diabetic nephropathy presents in its earliest stage with low levels of albumin (microalbuminuria) in the urine. This often is referred to as incipient nephropathy.
Does diabetes cause nephrotic syndrome?
In adults, approximately 30 percent of people with nephrotic syndrome have an underlying medical problem, such as diabetes or lupus; the remaining cases are due to kidney disorders such as minimal change disease, focal segmental glomerulosclerosis (FSGS), or membranous nephropathy.
Can Type 2 diabetes cause nephrotic syndrome?
On the other hand, specific treatment of non-diabetic renal disease in known diabetic patients is seldom applied. But when a patient with type 2 diabetes without retinopathy or autonomic neuropathy has a nephrotic syndrome then there is no doubt that kidney biopsy should be performed.
What is the most common type of diabetic neuropathy?
Peripheral neuropathy is the most common form of diabetic neuropathy. Your feet and legs are often affected first, followed by your hands and arms. Possible signs and symptoms of peripheral neuropathy include: Numbness or reduced ability to feel pain or temperature changes, especially in your feet and toes.
What is the meaning of nephropathy?
kidney diseaseNephropathy is a medical term for kidney disease. The type of kidney disease caused by diabetes is called diabetic nephropathy.
Why does neuropathy occur in diabetes?
Researchers think that over time, uncontrolled high blood sugar damages nerves and interferes with their ability to send signals, leading to diabetic neuropathy. High blood sugar also weakens the walls of the small blood vessels (capillaries) that supply the nerves with oxygen and nutrients.
What causes diabetic neuropathy?
Diabetic neuropathy is nerve damage that is caused by diabetes. Over time, high blood glucose levels, also called blood sugar, and high levels of fats, such as triglycerides, in the blood from diabetes can damage your nerves. Symptoms depend on which type of diabetic neuropathy you have.
How does hyperglycemia cause nephropathy?
Having high blood glucose levels due to diabetes can damage the part of the kidneys that filters your blood. The damaged filter becomes 'leaky' and lets protein into your urine. For some people, diabetic nephropathy can progress to chronic kidney disease and kidney failure.
What is the code for diabetic nephropathy?
When you look up "diabetic nephropathy" in the index the code listed is 250.4 (583.81) . The 250.4 needs an extra digit. When you go to 250.4 in the tabular, it tells you what fifth digit to assign in the box. Also, after 250.4, it says "use addition code to identify manifestation" which in this case, it would be nephropathy (583.81) . When you look up 583.81 in the tabular, it directs you to "code first underlying disease" (which is diabetes with renal manifestations.)
What is the ICd 9 code for diabetes mellitus?
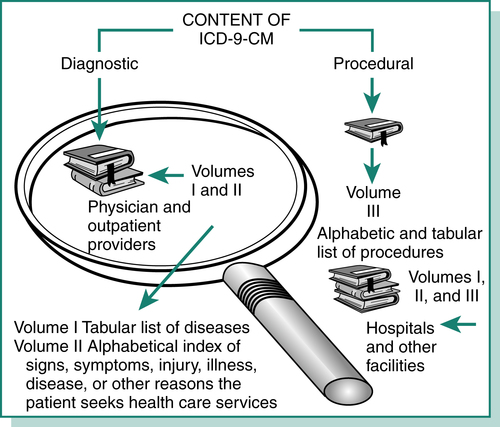
Assign code 250.40, Diabetes with renal manifestations, type II [non-insulin dependent type] [NIDDM type] [adult-onset type] or unspecified type, not stated as uncontrolled, and code 403.91, Hypertensive renal disease, with renal failure, for diabetic nephropathy with chronic renal failure and hypertension. Diabetes mellitus is one of several disease categories in ICD-9-CM where one code classifies both the disease and its manifestations. Additional codes may be assigned to further describe the manifestations. The following diagnoses: diabetic renal failure, diabetic uremia, diabetic intercapillary glomerulosclerosis and chronic renal failure, diabetic nephropathy with chronic renal failure, or diabetic nephrosis with chronic renal failure provide a cause-and-effect relationship, requiring that code 250.4X, Diabetes with renal manifestations, be sequenced first.
What is the ICd 9 code for CKD?
If you look at 585 category in the tabular, it says "code first, hypertensive CKD if applicable" and directs you to 403.00-403.91.
What is the ICD-9-CM for hypertension?
ICD-9-CM assumes a cause-and-effect relationship and classifies chronic renal failure with hypertension as hypertensive renal disease. At category 403, the note reads "any condition classifiable to 585, 586, 587 with any condition classifiable to 401." This wording indicates that the linkage is so compelling when both conditions are present (hypertension and chronic or unspecified renal failure) that hypertensive renal disease is coded. Therefore, if the physician has not indicated "CRF not due to hypertension," code 403.91, Hypertensive renal disease, unspecified, with renal failure, would be assigned.
What is the appropriate code for chronic kidney disease?
The appropriate code from category 585, chronic kidney disease should be used as a secondary code with a code from category 403 to identify the stage of chronic kidney disease.?
What chapter is neoplasms classified in?
Note: All neoplasms, whether functionally active or not, are classified in Chapter 2. Appropriate codes in this chapter (i.e. E05.8, E07.0, E16-E31, E34.-) may be used as additional codes to indicate either functional activity by neoplasms and ectopic endocrine tissue or hyperfunction and hypofunction of endocrine glands associated with neoplasms and other conditions classified elsewhere.
Do you need a 585 code for CKD?
The coding clinic does not state to not code the 585.- code it is clarifying that you do use the the 250.40 and the 403.91 together. The code categories 403 and 250.6 specify to add the additional codes therefore you do need the nephropathy and the CKD codes.
What is the ICD-10 code for diabetes?
For gestational diabetes (diabetes that occurs during pregnancy) women should be assigned a code under the 024.4 subheading and not any other codes under the 024 category.
When to use unspecified ICD-10?
The “unspecified” codes can be used when not enough information is known to give a more specific diagnosis; in that case, “unspecified” is technically more accurate than a more specific but as yet unconfirmed diagnosis. For more guidelines on using ICD-10 codes for diabetes mellitus, you can consult this document.
What Are ICD-10 Codes?
ICD-10 codes refer to the codes from the 10th Revision of the classification system. ICD-10 officially replaced ICD-9 in the US in October of 2015.
What type of diabetes code should be used for long term use?
The code for long-term use of insulin, Z79.4, should also be used in these cases (unless insulin was just given to the patient as a one-time fix to bring blood sugar under control).
Why did doctors switch to ICd 10?
The switch to ICD-10 was a response to the need for doctors to record more specific and accurate diagnoses based on the most recent advancements in medicine. For this reason, there are five times more ICD-10 codes than there were ICD-9 codes. The ICD-10 codes consist of three to seven characters that may contain both letters and numbers.
When writing a medical code on a medical record, should you give the longest code possible?
The more characters in the code, the more specific the diagnosis, so when writing a code on a medical record you should give the longest code possible while retaining accuracy.
Can diabetes be a ICd 9?
Here's a conversion table that translates the old ICD-9 codes for diabetes to ICD-10 codes. There weren’t as many codes to describe different conditions in the ICD-9, so you’ll notice that some of them have more than one possible corresponding ICD-10 code. Some are also translated into a combination of two ICD-10 codes (note the use of the word "and").
Where is the ICd 10 code for neuropathy?
Most of the neuropathy ICD 10 codes are located in Chapter-6 of ICD-10-CM manual which is “diseases of the nervous system”, code range G00-G 99
What is the code for neuropathy?
Neuropathic pain should be coded as neuralgia M79.2, not neuropathy.
What is the code for peripheral neuropathy?
Peripheral neuropathy with diabetes should be coded as E11.42 (DM with polyneuropath), not e11.40 (DM with neuropathy).
What are the symptoms of autonomic neuropathy?
Autonomic neuropathy symptoms can be heart intolerance, excess sweat or no sweat, blood pressure changes, bladder, bowel or digestive problems. Physician does a thorough physical examination including extremity neurological exam and noting vitals.
What tests are used to diagnose neuropathy?
Detailed history of the patient like symptoms, lifestyle and exposure to toxins may also help to diagnose neuropathy. Blood tests, CT, MRI, electromyography, nerve biopsy and skin biopsy are the tests used to confirm neuropathy.
Can peripheral neuropathy cause tingling?
Symptoms can vary in both peripheral and autonomic neuropathy because the nerves affected are different. Peripheral neuropathy symptoms can be tingling, sharp throbbing pain, lack of coordination, paralysis if motor nerves are affected. Autonomic neuropathy symptoms can be heart intolerance, excess sweat or no sweat, blood pressure changes, bladder, bowel or digestive problems.
Can neuropathy be transferred from parent to child?
There is hereditary neuropathy also which get transferred from parent to child. Neuropathy can occur in any nerve of the body, but peripheral neuropathy is the common type seen in most of the people. As the name says peripheral neuropathy affects peripheral nerves usually extremities (hands and feet).

Popular Posts:
- 1. 2016 icd 10 code for periapical lesion
- 2. icd 10 code for brain tumor unspecified
- 3. icd 10 code for encounter for depo provera injection
- 4. icd 10 code for dacryostenosis both eyes
- 5. icd 10 code for humeral fracture
- 6. icd 10 code for chf with exacerbation
- 7. screening colonoscopy for colon cancer. icd-10-cm code
- 8. icd 9 code for contusion ofleg
- 9. icd 10 code for hypoadrenalism
- 10. give 2 examples for when an ”external cause” icd code is required