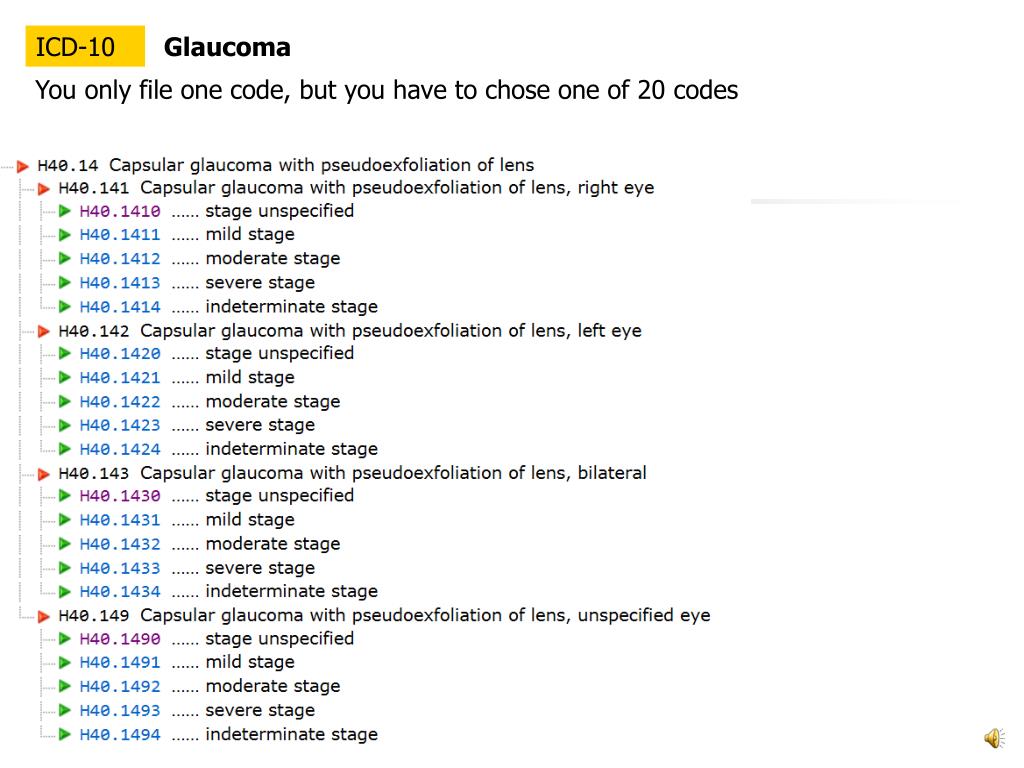
Some ICD-9 codes have a "V" or "E" in front of them. A "V" code is used for health services (usually preventive) that don't require a diagnosis. An "E" code describes an environmental cause of a health problem, such as an injury or poisoning. ICD-10 Codes The ICD-10 update completely overhauled the coding system.
Full Answer
What is the ICD 9 code for medical coding?
Feb 07, 2020 · Use the ICD-9-CM code that describes the patient's diagnosis, symptom, complaint, condition or problem. Do not code suspected diagnoses. Use the ICD-9-CM code that is the primary reason for the item or service provided. Assign codes to the highest level of specificity.
What is the ICD 10 code for no diagnosis?
The legacy ICD-9-CM system lacked the specificity needed to determine an exact diagnosis as the ICD-9 codes can be very broad and it became difficult to compare costs, treatments, and technologies. For that reason the ICD-9 code set was deprecated and replaced on September 30, 2015 by ICD-10 codes. The last version of ICD-9-CM had 14,567 diagnosis codes in 20 different …
What is the ICD 10 code for Z59 9?
Apr 16, 2022 · ICD-9-CM Medical Diagnosis Codes. The International Statistical Classification of Diseases and Related Health Problems (commonly known as the ICD) provides alpha-numeric codes to classify diseases and a wide variety of signs, symptoms, abnormal findings, complaints, social circumstances and external causes of injury or disease.
What happened to the ICD-9 code set?
Non-Billable On/After Oct 1/2015. ICD-9-CM V71.09 is a billable medical code that can be used to indicate a diagnosis on a reimbursement claim, however, V71.09 should only be used for claims with a date of service on or before September 30, 2015. For claims with a date of service on or after October 1, 2015, use an equivalent ICD-10-CM code (or codes).
Is there a diagnosis code for no diagnosis?
The DSM-5 Steering Committee subsequently approved the inclusion of this category, and its corresponding ICD-10-CM code, Z03. 89 "No diagnosis or condition," is available for immediate use.
What is the ICD-10 code for unknown diagnosis?
R69 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is non billable diagnosis code?
Non-Billable codes are used to capture and document activities that are not claimable to Medi- Cal. Certain activities are non-reimbursable procedures while certain service locations may block services from being claimed.
How many ICD-9 diagnosis codes are there?
13,000 codesThe current ICD-9-CM system consists of ∼13,000 codes and is running out of numbers.
Where do I find a diagnosis code?
If you need to look up the ICD code for a particular diagnosis or confirm what an ICD code stands for, visit the Centers for Disease Control and Prevention (CDC) website to use their searchable database of the current ICD-10 codes.9 Jan 2022
What is diagnosis code Z03 89?
Encounter for observation for other suspected diseases and conditions ruled out. Z03. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What are unspecified diagnosis codes?
An “unspecified” code means that the condition is unknown at the time of coding. An “unspecified” diagnosis may be coded more specifically later, if more information is obtained about the patient's condition. Example: There are multiple codes for hypothyroidism.
What does Provider non-billable mean?
PROVIDER CHARGES – the amount the provider actually charged for the services. NON-BILLABLE TO MEMBER – amount that the provider discounts for being in-network.
Does Medicare pay for unspecified diagnosis codes?
The Centers for Medicare and Medicaid Services (CMS) reminds providers that flexibilities surrounding unspecified codes ended as of October 1, 2016.5 Oct 2016
What is an example of a diagnosis code?
A diagnosis code is a combination of letters and/or numbers assigned to a particular diagnosis, symptom, or procedure. For example, let's say Cheryl comes into the doctor's office complaining of pain when urinating.6 Jan 2022
What is the difference between ICD-9 and ICD-10 codes?
The biggest difference between the two code structures is that ICD-9 had 14,4000 codes, while ICD-10 contains over 69,823. ICD-10 codes consists of three to seven characters, while ICD-9 contained three to five digits.24 Aug 2015
Is ICD-9 still used in 2020?
Currently, the U.S. is the only industrialized nation still utilizing ICD-9-CM codes for morbidity data, though we have already transitioned to ICD-10 for mortality.
What is the ICD-10 code for a nonspecific condition?
ICD-10 guidelines offer clear specifications on billing codes even when a nonspecific condition presents itself and no diagnosis is forthcoming. While the process of arriving at the correct code may be confusing, getting the coding correct will lead to accurate billing, which translates into timelier payments, happier patients, and avoidance of underpayments. As such, every effort should be made to research and apply the appropriate codes, even in cases where the physician cannot make a diagnosis.
Why is there no diagnosis in medical billing?
In many cases, patients come in with symptoms that prompt them to seek medical treatment, yet the physician can make no diagnosis. These cases often result in errors in medical billing coding due to confusion about how to handle the situation. However, in every case, a method exists for proper coding and billing for treatment.
Is preventive care covered by insurance?
Preventive care services are often covered by a patient’s insurance and can be billed under the appropriate code for the visit. These can include instances where the patient is being evaluated due to a personal history that makes a disease more likely in their case.
Can a doctor visit not result in diagnosis?
There are several circumstances that may arise for a doctor/patient visit that does not result in a diagnosis being reached. For many of these circumstances, there are clear guidelines for medical claims processing on how to code and bill for these services.
Three guidelines, four notes
There are three general guidelines to follow for reporting signs and symptoms in ICD-10:
Common codes in family medicine
Now that you understand the basic ICD-10 guidance regarding symptoms, signs, and test results, take a look at some of the codes you're most likely to use in family medicine. The list includes ICD-10 codes for the signs and symptoms included on FPM 's ICD-9 “short list” with a bit more specificity where sites are included.

Common Circumstances Where No Diagnosis May Be Reached
- There are several circumstances that may arise for a doctor/patient visit that does not result in a diagnosis being reached. For many of these circumstances, there are clear guidelines for medical claims processing on how to code and bill for these services. Preventive care services are often covered by a patient’s insurance and can be billed under the appropriate code for the visit. Thes…
Cases Where An Ill Patient Does Not Receive A Diagnosis
- In many cases, patients come in with symptoms that prompt them to seek medical treatment, yet the physician can make no diagnosis. These cases often result in errors in medical billing coding due to confusion about how to handle the situation. However, in every case, a method exists for proper coding and billingfor treatment. In many cases, where a diagnosis is not immediately abl…
Avoiding Overbilling For Nonspecific Conditions
- ICD-10 guidelines offer clear specifications on billing codes even when a nonspecific condition presents itself and no diagnosis is forthcoming. While the process of arriving at the correct code may be confusing, getting the coding correct will lead to accurate billing, which translates into timelier payments, happier patients, and avoidance of underpayments. As such, every effort sho…
Popular Posts:
- 1. icd 10 code for diaper
- 2. icd 10 code for elevated tbili
- 3. what is the icd 10 code for tinnitus
- 4. icd 10 cm code for osteoporosis
- 5. icd 10 code for excisional debridement right upper arm
- 6. icd 10 code for left gastrocnemius strain
- 7. icd 10 code for pelvic brown discharge
- 8. icd-10 code for chronic uti
- 9. icd 10 code for pretibial myxedema
- 10. icd-9-cm code for bmi 40