Full Answer
What are unspecified codes in ICD-9?
The ICD-9 manual lists several types of unspecified codes, including “unspecified,” “NEC” (not elsewhere classifiable,” and “NOS” (not otherwise specified). Providing the most specific ICD-9 codes is important for several reasons. For one, many hospitals use these codes to keep track of their utilization management.
What is the ICD 10 code for treatment not carried out?
Procedure and treatment not carried out, unspecified reason. Z53.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2018/2019 edition of ICD-10-CM Z53.9 became effective on October 1, 2018.
What is the ICD 10 code for left without being seen?
Left against medical advice Left without being seen Personal condition, left against medical advice ICD-10-CM Z53.21 is grouped within Diagnostic Related Group (s) (MS-DRG v38.0):
What is the ICD 9 code for diabetes mellitus not otherwise specified?
When the medical record doesn’t contain this type of information, the coder must default to ICD-9 250.00. This code indicates only diabetes mellitus with no mention of complication, not stated as uncontrolled. This code is also known as diabetes mellitus not otherwise specified (NOS).

What is the ICD-10 code for left without being seen?
Z53.21Z53. 21 - Procedure and treatment not carried out due to patient leaving prior to being seen by health care provider | ICD-10-CM.
What is the ICD-10 code for no show?
Z53. 20 - Procedure and treatment not carried out because of patient's decision for unspecified reasons | ICD-10-CM.
How do you code a procedure not carried out?
ICD-10-CM Code for Procedure and treatment not carried out because of other contraindication Z53. 09.
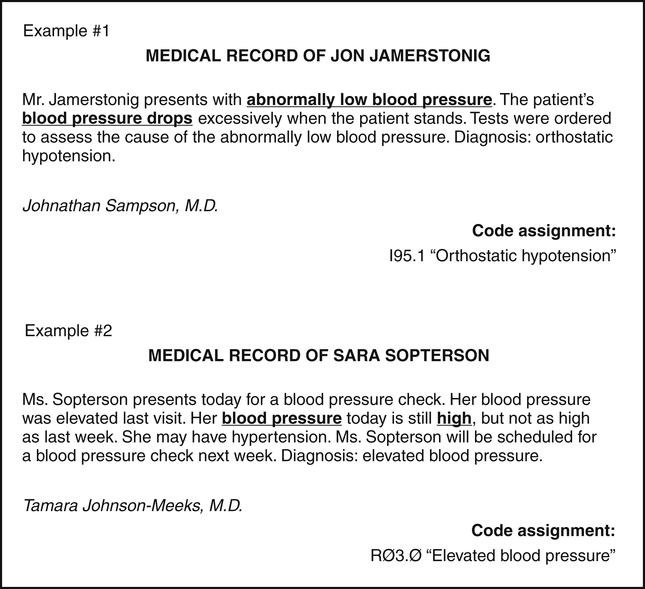
What should you code when a definitive diagnosis has not been established?
The general guidelines say, “If a definitive diagnosis has not been established by the end of the encounter, it is appropriate to report codes for sign(s) and/or symptom(s) in lieu of a definitive diagnosis.”
What is diagnosis code Z03 89?
Z03. 89 No diagnosis This diagnosis description is CHANGED from “No Diagnosis” to “Encounter for observation for other suspected diseases and conditions ruled out.” established. October 1, 2019, with the 2020 edition of ICD-10-CM.
What is diagnosis code Z029?
Encounter for administrative examinations, unspecifiedicd10 - Z029: Encounter for administrative examinations, unspecified.
What modifier is used for unsuccessful procedure?
Modifier 53 applies if the provider quits a procedure because the patient is at risk. In other words, the provider does not so much choose to discontinue the procedure, as sound medical practice compels him or her to do so.
What is reason code B15?
Denial Reason, Reason/Remark Code(s) CO-B15: Payment adjusted because this procedure/service requires that a qualifying service/procedure be received and covered. The qualifying other service/procedure has not been received/adjudicated.
Can you bill for unsuccessful procedure?
Yes, you can bill a procedure that is unsuccessful - IF - Big, Red, IF it is documented.
What is an uncertain diagnosis?
A: Uncertain diagnoses are those that at the time of discharge are still being documented as “probable,” “suspected,” “likely,” “questionable,” “possible,” “still to be ruled out,” or other similar terminology.
How do you code a suspected diagnosis?
Do not code diagnoses documented as “probable”, “suspected”, “questionable”, “rule out”, or “working diagnosis”. Rather, code the condition(s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit.
What diagnosis codes Cannot be primary?
Diagnosis Codes Never to be Used as Primary Diagnosis With the adoption of ICD-10, CMS designated that certain Supplementary Classification of External Causes of Injury, Poisoning, Morbidity (E000-E999 in the ICD-9 code set) and Manifestation ICD-10 Diagnosis codes cannot be used as the primary diagnosis on claims.
What is the ICd 9 code for symptoms?
Chapter 16 of ICD-9-CM, Symptoms, Signs, and Ill-defined conditions (codes 780.0 - 799.9) contain many, but not all codes for symptoms.
What are the conventions of ICd 9?
The conventions for the ICD-9-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the index and tabular of the ICD -9-CM as instructional notes. The conventions are as follows:
What is a category 250 code?
Codes under category 250, Diabetes mellitus, identify complications/manifestations associated with diabetes mellitus. A fifth-digit is required for all category 250 codes to identify the type of diabetes mellitus and whether the diabetes is controlled or uncontrolled.
What is the code for MRSA?
If a patient is documented as having both MRSA colonization and infection during a hospital admission, code V02.54, Carrier or suspected carrier, Methicillin resistant Staphylococcus aureus, and a code for the MRSA infection may both be assigned.
What does "see" mean in index?
The “see” instruction following a main term in the index indicates that another term should be referenced. It is necessary to go to the main term referenced with the “see” note to locate the correct code.
What does "with" mean in a code?
The word “with” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index, or an instructional note in the Tabular List.
What are conventions and guidelines?
The conventions, general guidelines and chapter-specific guidelines are applicable to all health care settings unless otherwise indicated. The conventions and instructions of the classification take precedence over guidelines.
What are the components of a 99283?
99283 requires all 3 components; Hx, exam and mdm.
Can you charge for vitals without seeing the doctor?
They can charge you (facility side) a minimum of a 99281 for vitals. However, if they ordered an x-ray or blood work then they can code for a 99283. If this is for physician side, I would dispute the charge. If it is facility and nothing was done but vitals, again I would dispute the charge. Hope this helps.
Why is Z53.09 not carried out?
Z53.09 Procedure and treatment not carried out because of other contraindication. Z53.1 Procedure and treatment not carried out because of patient's decision for reasons of belief and group pressure. Z53.2 Procedure and treatment not carried out because of patient's decision for other and unspecified reasons.
When will the ICd 10 Z53.21 be released?
The 2022 edition of ICD-10-CM Z53.21 became effective on October 1, 2021.
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
What is the ICd 9 code for prostate cancer?
ICD-9 code 185 and ICD-10 code C61 are the diagnostic codes used for malignant neoplasm of the prostate. Note that ICD-9 code 185 and ICD-10 code C61 contain three characters. 185 is all numeric and C61 is alpha-numeric. Most ICD-9 codes are numeric and all ICD-10 codes are alpha-numeric. Codes 185 and C61 include the various histological malignant tumors of the prostate namely, the common adenocarcinoma, transitional cell tumors, squamous cell tumors, and prostatic sarcoma. Other diagnoses often associated with neoplasms of the prostate include carcinoma in situ of the prostate, high grade prostatic intraepithelial neoplasm, high grade PIN, diagnostic codes 233.4 for ICD-9 and D07.5 for ICD-10, dysplasia of the prostate, PIN grades 1 and 2, diagnostic codes 602.3 for ICD-9 and N42.3 for ICD-10 ( Table 63.1 ). ICD-9 code 790.93 and ICD-10 code R07.2 indicate an elevated prostate-specific antigen (PSA). A PSA level is considered elevated when determined as elevated by the attending urologist not only by the determined level itself. For example, an elevation of PSA above four may or may not represent a true elevation. However, a PSA level of 0.5 several months after a radical prostatectomy would represent an elevation. In either example the diagnosis would be 790.93, elevation of PSA.
What is the advantage of ICD-9 scoring?
Another advantage of ICD-9 scoring is that risk stratification can easily be expanded to include coded comorbidities. 35 ICISS does not include physiologic data; however, it predicts mortality, costs, and length of stay as well as or better than risk adjustment models like TRISS and ASCOT that do. 35–40.
What is the difference between CPT and HCPCS?
5 The breadth of HCPCS is larger than that of CPT, encompassing both goods and services. As a result, the accommodation of CPT within HCPCS is accomplished by dividing HCPCS into three levels with level I being identical to CPT, level II representing an additional set of nonphysician services such as ambulance rides, durable medical goods such as walkers, and level III representing additional “local codes” for use within specific jurisdictions such as state-level Medicaid programs or Medicare contractors. In any case, both HCPCS and CPT codes consist of five characters where, as mentioned, level I HCPCS and CPT codes are equivalent meaning that codes authored as CPT are simply understood as HCPCS level I codes by CMS without any transformation of the code itself.
How many characters are in a CPT code?
In any case, both HCPCS and CPT codes consist of five characters where, as mentioned, level I HCPCS and CPT codes are equivalent meaning that codes authored as CPT are simply understood as HCPCS level I codes by CMS without any transformation of the code itself.
Why is it laborious to map a test to a linc?
Mapping laboratory tests to LOINC becomes laborious because the documentation necessary to do the mapping accurately is often missing from the E HR, as stated earlier; you have to gather the information through interviews with the laboratory staff. LOINC also has its idiosyncrasies: if a test for a substance is expressed in different units (eg, pounds vs. kilograms; milligrams vs. micrograms) its LOINC code does not change except when it is expressed in molar units (eg, micromoles per unit volume). This does not make sense from the scientific perspective: a mole is merely a different kind of unit, based upon the substance’s molecular weight in grams. In other words, mapping to LOINC is necessary but not sufficient for interoperation: all systems that share a particular test must have the data converted to an identical unit at some point. Otherwise, if pooled, “normal” numerical values may vary by several orders of magnitude.
What is PCS code?
PCS codes are compact but highly formulaic making them amenable to expansion into a tabular format to ease analysis. For example, it may be worthwhile to create a table with seven columns, which are populated with the seven character value-encoded terms from a patient’s given PCS code and an eighth column with patient’s unique identifier. This makes it possible to apply simpler SQL-based selection criteria to identify patients with similar procedure attributes.
Why should ICD-9 based scores be supplemented?
ICD-9 based scores (ICISS) should begin to supplement (and may supplant) AIS-based scores (ISS) because these ICD-9 based scores have better statistical properties and are less expensive to calculate.
Why is it important to have ICD-9 codes?
Providing the most specific ICD-9 codes is important for several reasons. For one, many hospitals use these codes to keep track of their utilization management. ICD-9 codes are also used by public health officials to track epidemics, create census reports , and for medical research purposes. While ICD-9 codes are updated every year, ...
How often are ICD-9 codes updated?
While ICD-9 codes are updated every year , the reality is that it’s all too easy for both physicians and coders to become complacent and use a narrow range of codes with which they are familiar. The good news is that when physicians provide enough detail in the medical record, coders can avoid using these codes altogether.
What is the ICD-9 code for myocardial infarction?
Once again, the coder must use myocardial infarction of unspecified site, with unspecified episode ICD-9 410.90. Tamra McLain can be reached through e-mail.
What happens if you don't give your coders enough information?
If you don’t give your coders enough information in the medical record, they’ll be forced to report this code. Both you and your hospital won’t receive your due credit for taking care of a sicker patient.
What is the difference between benign and malignant hypertension?
The ICD-9 manual lists two basic types of hypertension. Benign hypertension is defined as generally asymptomatic and stable, while malignant hypertension can include symptoms such as headache or vision problems. In addition, malignant hypertension starts with abrupt onset and often ends with renal failure and/or CVA.
Popular Posts:
- 1. icd 10 code for left knee trauma
- 2. icd-10 code for cracked skin on foot
- 3. icd 9 code for homocysteine
- 4. icd 10 code for sprain toe
- 5. icd 10 code for acute pulmonary embolus
- 6. icd 10 cm code for toenail fungus
- 7. icd 9 code for seizure unspecified
- 8. icd-10 code for combs positive
- 9. icd 10 code for right wrist instability
- 10. icd 10 code for cyst removal