What is the format for ICD 9 diagnosis codes?
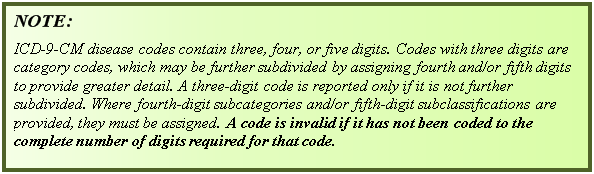
The format for ICD-9 diagnoses codes is a decimal placed after the first three characters and two possible add-on characters following: xxx.xx. ICD-9 PCS were used to report procedures for inpatient hospital services from Volume 3, which represent procedures that were done at inpatient hospital facilities.
Where can I find free ICD-9 coding reference?
The Web's Free ICD-9-CM Medical Coding Reference. ICD9Data.com takes the current ICD-9-CM and HCPCS medical billing codes and adds 5.3+ million links between them. Combine that with a Google-powered search engine, drill-down navigation system and instant coding notes and it's easier than ever to quickly find the medical coding information you need.
What does ICD-9-CM mean?
ICD-9 Lookup The ICD-9-CM was an adaption maintained by the Centers for Medicare and Medicaid Services (CMS) that was used for assigning diagnostic codes associated with inpatient, outpatient, and physician office utilization.
What is osteogenesis imperfecta ICD 10?
Definition of ICD-10 Q78.0. Osteogenesis imperfecta (OI, or brittle bones disease) is a group of genetic disorders that mainly affect the bones. The term "osteogenesis imperfecta" means imperfect bone formation. People with this condition have bones that break easily, often from mild trauma or with no apparent cause.

What ICD-9 codes?
ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started.
Are ICD-9 codes still used in 2021?
CMS will continue to maintain the ICD-9 code website with the posted files. These are the codes providers (physicians, hospitals, etc.) and suppliers must use when submitting claims to Medicare for payment.
What is clinical Modification?
The ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) is a system used by physicians and other healthcare providers to classify and code all diagnoses, symptoms and procedures recorded in conjunction with hospital care in the United States.
What type of code may be used when two diagnoses or a diagnosis with a secondary process is present?
Combination Codes: single code used to identify two diagnoses, or a diagnosis with a secondary process or manifestation, or a diagnosis with an associated complication.
When was ICD-9 discontinued?
Therefore, CMS is to eliminating the 90-day grace period for billing discontinued ICD-9- CM diagnosis codes, effective October 1, 2004.
What is the difference between ICD-9 and ICD-10?
ICD-9 uses mostly numeric codes with only occasional E and V alphanumeric codes. Plus, only three-, four- and five-digit codes are valid. ICD-10 uses entirely alphanumeric codes and has valid codes of up to seven digits.
Is ICD-9 still used in 2020?
In the United States, ICD-10 has been used since 1999 to code and classify mortality data from death certificates. However, a modification of the 9th revision (ICD-9) is still used to assign codes to diagnoses associated with inpatient, outpatient, and physician office use and for inpatient procedures.
Who can change a diagnosis code?
Your healthcare provider may be able to change the diagnosis code to one that gives you the coverage you need. If ICD-10 coding is not the reason for the billing issue, you may need to make an appeal with your insurance company.
What ICD-10 codes Cannot be primary?
Diagnosis Codes Never to be Used as Primary Diagnosis With the adoption of ICD-10, CMS designated that certain Supplementary Classification of External Causes of Injury, Poisoning, Morbidity (E000-E999 in the ICD-9 code set) and Manifestation ICD-10 Diagnosis codes cannot be used as the primary diagnosis on claims.
What type of code may be used when two diagnoses or a diagnosis with a secondary process is present quizlet?
What is a combination code? A combination code is a single code used to classify 1) two diagnoses, 2) a diagnosis with an associated secondary process (manifestation), or 3) a diagnosis with an associated complication.
Is it possible that ICD-9 and ICD 10 codes will be used simultaneously?
However, most ICD-9-CM codes are still matched with multiple terms in ICD-10-CM, and there is still room for double billing during the period when the two systems will be activated simultaneously.
What is the difference between IDC 9 and ICD-10?
The major differences between the two code systems include the number of characters involved. ICD-9 has up to five characters while ICD-10 has up to seven. ICD-10 adds laterality (preference to use one side of the body more than the other) to the coding system, which ICD-9 lacks.
What type of code describes two diagnoses or a diagnosis with an associated complication quizlet?
Combination codes may also exist that classify two diagnoses or one diagnoses with an associated complication. The diseases and injuries in the Tabular List are organized into chapters according to etiology, body system, or purpose.
When two or more interrelated conditions are present that qualify for principal diagnosis either may be listed first?
When there are two or more interrelated conditions (such as diseases in the same ICD-10- CM chapter or manifestations characteristically associated with a certain disease) potentially meeting the definition of principal diagnosis, either condition may be sequenced first, unless the circumstances of the admission, the ...
Which type of code is important to include because the individuals health status might affect the course of treatment and its outcome?
A status code is informative, because the status may affect the course of treatment and its outcome. A status code is distinct from a history code.
Can Z codes be used as principal diagnosis?
Z codes may be used as either a first-listed (principal diagnosis code in the inpatient setting) or secondary code, depending on the circumstances of the encounter. Certain Z codes may only be used as first-listed or principal diagnosis.
What is the ICd 10 code for brittle bones?
Definition of ICD-10 Q78.0. Osteogenesis imperfecta (OI, or brittle bones disease) is a group of genetic disorders that mainly affect the bones. The term "osteogenesis imperfecta" means imperfect bone formation. People with this condition have bones that break easily, often from mild trauma or with no apparent cause.
What is the ICd 9 code for a syringe?
For claims with a date of service on or after October 1, 2015, use an equivalent ICD-10-CM code (or codes).
Is osteogenesis imperfecta life threatening?
Osteogenesis imperfecta can sometimes be life-threatening if it occurs in babies either before or shortly after birth. Approximately one person in 20,000 will develop brittle bone disease. It occurs equally among males and females and among ethnic groups.
Can multiple fractures occur before birth?
Multiple fractures are common, and in severe cases, can occur even before birth. Milder cases may involve only a few fractures over a person's lifetime. Additional complications can involve hearing loss, heart failure, spine issues, and deformities.
Popular Posts:
- 1. icd 10 code for stage iv adenocarcinoma of the lung
- 2. icd 10 code for history esophageal ulcer
- 3. icd 10 code for ataxia (a staggering gait)
- 4. icd 10 cm code for peg tube issues
- 5. icd 10 code for reduced libido
- 6. icd 10 code for left lower lobe pulmonary embolism
- 7. icd 10 code for dm lowe extremity ulcers
- 8. what is icd 10 code for visit with no abnormal findings
- 9. icd 10 code for exposure to carbon monoxide
- 10. icd 10 code for cellulitis left foot