What is the ICD 10 code for pleural empyema?
Empyema of pleura. Pleural empyema (pus between lung and chest wall) Clinical Information. Suppurative inflammation of the pleural space. ICD-10-CM J86.9 is grouped within Diagnostic Related Group (s) (MS-DRG v38.0): 177 Respiratory infections and inflammations with mcc.
What is the ICD 9 code for pleurisy?
Diagnosis Code 511.9. ICD-9: 511.9. Short Description: Pleural effusion NOS. Long Description: Unspecified pleural effusion. This is the 2014 version of the ICD-9-CM diagnosis code 511.9. Code Classification. Diseases of the respiratory system (460–519) Other diseases of respiratory system (510-519) 511 Pleurisy.
What is the CPT code for pleural effusion?
511.9 is a legacy non-billable code used to specify a medical diagnosis of unspecified pleural effusion.
What is the pH of pleural fluid with emphysema?
Empyema fluid generally has a pH of less than 7.2, a glucose level of less than 40mg/dL, and an LDH activity generally over 1,000IU/L. A pleural fluid pH below 7.2 indicates the need for drainage. If the pleural effusion is secondary to pancreatitis (usually on the left)...
What is the ICD-10-CM code for empyema?
ICD-10-CM Diagnosis Code J01 8); acute abscess of sinus; acute empyema of sinus; acute infection of sinus; acute inflammation of sinus; acute suppuration of sinus; code (B95-B97) to identify infectious agent.
What is the ICD 10 code for left empyema?
Convert to ICD-10-CM: 510.9 converts approximately to: 2015/16 ICD-10-CM J86. 9 Pyothorax without fistula.
What is the ICD code for pleural effusion?
ICD-10 Code for Pleural effusion in other conditions classified elsewhere- J91. 8- Codify by AAPC.
What is the ICD 10 code for pleural effusion unspecified?
J91. 8 - Pleural effusion in other conditions classified elsewhere | ICD-10-CM.
Is empyema a type of pleural effusion?
Pleural empyema is a collection of pus in the pleural cavity caused by microorganisms, usually bacteria. Often it happens in the context of a pneumonia, injury, or chest surgery. It is one of the various kinds of pleural effusion.
How do you code empyema?
J86. 9 converts approximately to one of the following ICD-9-CM codes: 510.9 - Empyema without mention of fistula.
What is the ICD 10 code for History of pleural effusion?
J91. 8 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM J91. 8 became effective on October 1, 2021.
Do you code pleural effusion with CHF?
A: Usually, pleural effusion is integral to congestive heart failure and isn't coded as a secondary diagnosis. But, if the physician documents that the pleural effusion is clinically significant and required monitoring and further evaluation, then it can be reported as a secondary diagnosis.
What causes pleural effusion?
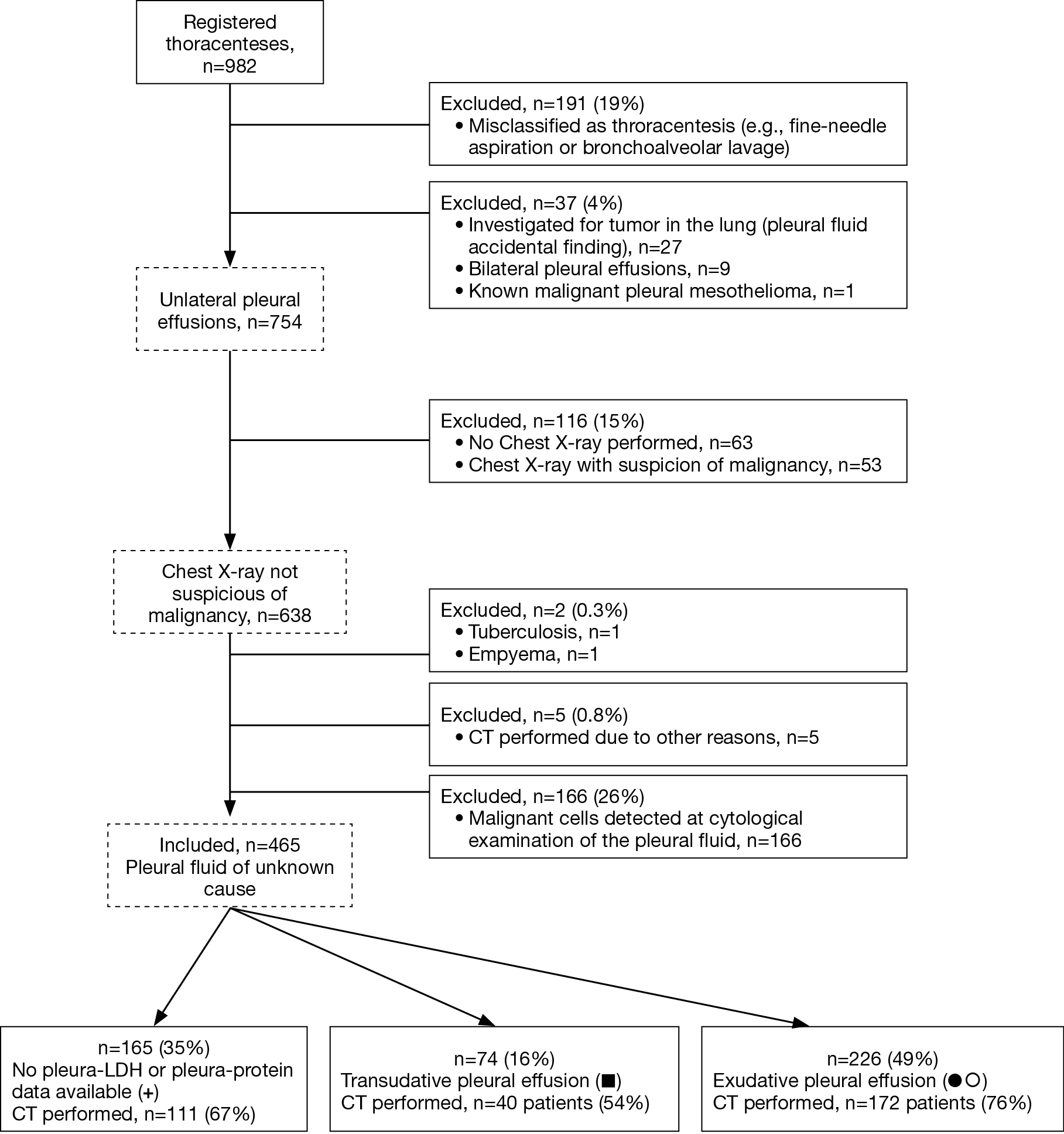
The most common causes of pleural effusion are congestive heart failure, cancer, pneumonia, and pulmonary embolism. Pleural fluid puncture (pleural tap) enables the differentiation of a transudate from an exudate, which remains, at present, the foundation of the further diagnostic work-up.
What is pleural effusion in medical terms?
Listen to pronunciation. (PLOOR-ul eh-FYOO-zhun) An abnormal collection of fluid between the thin layers of tissue (pleura) lining the lung and the wall of the chest cavity.
What is malignant pleural effusion?
A malignant pleural effusion (MPE) is the build up of fluid and cancer cells that collects between the chest wall and the lung. This can cause you to feel short of breath and/or have chest discomfort. It is a fairly common complication in a number of different cancers.
What is the ICD 10 code for pleural drain?
Drainage of Right Pleural Cavity with Drainage Device, Percutaneous Approach. ICD-10-PCS 0W9930Z is a specific/billable code that can be used to indicate a procedure.
What is an empyema?
Empyema is the medical term for pockets of pus that have collected inside a body cavity. They can form if a bacterial infection is left untreated, or if it fails to fully respond to treatment. The term empyema is most commonly used to refer to pus-filled pockets that develop in the pleural space.
What is empyema Thoracis?
Empyema thoracis is an infection of the pleural space that is most commonly a complication of pneumonia (parapneumonic),[1–3] but also can be a complication of primary fungal or mycobacterial infections (tuberculous), a complication of abdominal infections (sub-phrenic abscess, infected pancreas necrosis, spontaneous ...
How is empyema treated?
Antibiotics are prescribed to control the infection. A doctor will place a chest tube to completely drain the pus. A surgeon may need to perform a procedure to peel away the lining of the lung (decortication) if the lung does not expand properly.
Is the collection of pus in the pleural cavity?
Empyema is defined as a collection of pus in the pleural cavity, gram-positive, or culture from the pleural fluid. Empyema is usually associated with pneumonia but may also develop after thoracic surgery or thoracic trauma.
When will the ICD-10 J86.9 be released?
The 2022 edition of ICD-10-CM J86.9 became effective on October 1, 2021.
When a respiratory condition is described as occurring in more than one site and is not specifically indexed, it should be?
When a respiratory condition is described as occurring in more than one site and is not specifically indexed, it should be classified to the lower anatomic site (e.g. tracheobronchitis to bronchitis in J40 ).
What is empyema in the lung?
Empyema is a collection of pus between the lung and the chest wall (pleural space). Infections of the pleural space most commonly follow pneumonia, accounting for 40 to 60% of all empyema. Thoracotomy is the next most common cause of empyema, accounting for approximately 20%, and trauma accounts for another 10%. Less commonly empyema can develop following esophageal rupture, subdiaphragmatic spread, or direct extension from head and neck infections.
What causes empyema in the pleural space?
The most common cause of empyema is extension of bacterial infection of the lung into the pleural space. This accounts for 40 to 60% of cases in most publications. Prior thoracic surgery accounts for another 20% of cases, and extension from subdiagphragmatic infections accounts for 5 to 10%.
How did the patient develop empyema? What was the primary source from which the infection spread?
The most common cause of empyema is extension of bacterial infection of the lung into the pleural space. This accounts for 40 to 60% of cases in most publications. Prior thoracic surgery accounts for another 20% of cases, and extension from subdiagphragmatic infections accounts for 5 to 10%.
What imaging studies will be helpful in making or excluding the diagnosis of empyema?
The standard plain chest X-ray is still useful in detecting pleural effusions which may represent an empyema. Up to 200 to 500mL of pleural fluid is necessary to be visible on a plain X-ray. A lateral decubitus film can detect as little as 5mL of free pleural fluid. Most studies recommend a thoracentesis if on a lateral decubitus film the fluid is more than 10mm. Ultrasound is widely available and costs much less than computed tomography (CT) or magnetic resonance imaging (MRI). Ultrasound is useful for detecting small amounts of pleural fluid and can be useful for guiding diagnostic thoracentesis or for pleural drainage. CT has emerged as the imaging study of choice. It is more accurate in distinguishing lung abscess from empyema than traditional chest films. Chest CT with contrast may also help differentiate transudates from exudates. Pleural thickening and enhancement is usually only seen with exudative effusions. The role of MRI in the evaluation of empyema is more limited. It may be useful when intravenous contrasts cannot be given with CT imaging. MRI can detect pleural effusions, pleural tumors, and chest wall invasion. In some cases MRI can distinguish hemorrhagic causes from other etiologies. MRI may be able to differentiate transdates from exudates with the use of triple echo pulse sequence or the use of gadolinium.
What other clinical manifestations may help me to diagnose and manage empyema?
In patients with tuberculosis, symptoms of weight loss, night sweats, fever, and hemoptysis may be helpful clues to the diagnosis. In patients with actinomycosis, the development of a draining fistula with sulfa granules is very suggestive.
How can empyema be prevented?
The use of influenza vaccine can reduce infection due to influenza, which in turn reduces the risk of secondary bacterial pneumonia, particularly S. pneumoniae and S. aureus. Despite an increase in empyema of all causes, the rate of pneumococcal empyema has been stable. It is possible that this may be due to the introduction of conjugated vaccine (PCV7) in children, which started in 2000 and which has resulted in a decrease in pneumonia hospitalization in both children and adults. However, recent studies observed an increase in pneumococcal pneumonia and empyema in children aged less than 5 years. Most of this has been with serotypes not covered in the PCV7 formulation. The recent introduction of a 13-valent pneumocococal conjugated vaccine should provide protection against serotypes 1, 3, 7F, and 19A, which are associated with empyema.
How to determine if empyema is transudative or exudative?
After obtaining fluid, the first step is to determine if the effusion is transudative or exudative by applying Light criteria (Table I). Fluid obtained by thoracentesis should be sent for cell count with differential, glucose, protein, lactate dehydrogenase (LDH), and pH. If tuberculous empyema is suspected an adenosine deaminase determination or polymerase chain reaction (PCR) assay for M tuberculosis can be sent. Fluid should be sent to microbiology for Gram stain and aerobic and anaerobic cultures. Detection of pneumococcal antigen in pleural fluid increases the yield over conventional microbiology, particularly if the patient has received prior antibiotics. Cytology studies should be sent if a malignant effusion is suspected.
What is the clinical presentation of pleural empyema?
The clinical presentation of both the adult and pediatric patient with pleural empyema depends upon several factors, including the causative micro-organism. Most cases present themselves in the setting of a pneumonia, although up to one third of patients do not have clinical signs of pneumonia and as many as 25% of cases are associated with trauma ...
How many pleural effusions are there in pneumonia?
Simple pleural effusions occur in up to 40% of bacterial pneumonias. They are usually small and resolve with appropriate antibiotic therapy. If however an empyema develops additional intervention is required.
What are the risk factors for pleural empyema?
Risk factors include alcoholism, drug use, HIV infection, neoplasm and pre-existent pulmonary disease.
What is the treatment for pleural empyema?
Treatment. Supportive care, antibiotics, surgery, chest tube. Pleural empyema is a collection of pus in the pleural cavity caused by microorganisms, usually bacteria. Often it happens in the context of a pneumonia, injury, or chest surgery. It is one of the various kinds of pleural effusion.
What are the stages of pleural fluid?
There are three stages: exudative, when there is an increase in pleural fluid with or without the presence of pus; fibrinopurulent, when fibrous septa form localized pus pockets; and the final organizing stage, when there is scarring of the pleura membranes with possible inability of the lung to expand.
What is proven empyema?
Proven empyema (as defined by the "golden" criteria mentioned earlier) is an indication for prompt chest tube drainage. This has been shown to improve resolution of the infection and shorten hospital admission. Data from a meta-analysis has shown that a pleural fluid pH of <7.2 is the most powerful indicator to predict the need for chest tube drainage in patients with non-purulent, culture negative fluid. Other indications for drainage include poor clinical progress during treatment with antibiotics alone and patients with a loculated pleural collection.
How long does it take for empyema to return to normal?
Chest radiograph returns to normal in the majority of patients by 6 months. Patients should, of course, be advised to return sooner if symptoms redevelop.
What is the ICD code for pleural empyema?
The ICD code J86 is used to code Pleural empyema. Pleural empyema, also known as pyothorax or purulent pleuritis, is empyema (an accumulation of pus) in the pleural cavity that can develop when bacteria invade the pleural space, usually in the context of a pneumonia. It is one of various kinds of pleural effusion.
What are the stages of pleural fluid?
There are three stages: exudative, when there is an increase in pleural fluid with or without the presence of pus; fibrinopurulent, when fibrous septa form localized pus pockets; and the final organizing stage, when there is scarring of the pleura membranes with possible inability of the lung to expand.
What is the approximate match between ICd9 and ICd10?
This is the official approximate match mapping between ICD9 and ICD10, as provided by the General Equivalency mapping crosswalk. This means that while there is no exact mapping between this ICD10 code J86.9 and a single ICD9 code, 511.0 is an approximate match for comparison and conversion purposes.
What is billable code?
Billable codes are sufficient justification for admission to an acute care hospital when used a principal diagnosis.
Can pleural effusion be a sign of congestive heart failure?
Pleural effusion is commonly seen with congestive heart failure with or without pulmonary edema. The pulmonary veins and lymphatics drain the pleural space and return fluid to the heart. In left heart failure, which results in elevated pressures in the venous system, there is usually some accumulation of fluid in the pleural space. Ordinarily the pleural effusion is minimal and is not specifically addressed other than by more aggressive treatment of the underlying congestive heart failure. In this situation it should not be reported unless the coder is directed to do so by the physician.
Can pleural effusion be documented?
Pleural effusion documented only as an x-ray finding without the physician having made such a diagnosis should not be reported. Occasionally, however, special x-rays such as decubitus views are required to confirm the presence of pleural effusion or a diagnostic thoracentesis may be performed to identify its etiology.
What DRG grouping is pleural effusion?
If no possible etiology can be identified, then the pleural effusion is the principal diagnosis and DRG assignment would be to the DRG grouping of 186, 187 or 188. The provider could also identify a probable etiology if the etiology is uncertain, allowing for a more specific DRG to be assigned.
Is pleural effusion a heart failure?
First, understand the coders’ motivation—a pleural effusion is considered integral to heart failure, and would not be coded separately if related to heart failure, so likely he or she is trying to identify the etiology of the pleural effusion.
Popular Posts:
- 1. icd-10 code for iron deficiency anemia
- 2. icd code for right inguinal hernia
- 3. icd 10 code for muscle tenderness
- 4. icd 10 code for left buttock pressure ulcer unstageable
- 5. what is the icd 10 code for infection of screws
- 6. icd 10 code for cervical spine s p fusion surgery
- 7. icd 10 code for status post gallbladder removal
- 8. icd 10 code for fungal infection of the foot
- 9. 2017 icd 10 code for cbd sludge
- 10. icd 10 code for high blood pressure in pregnancy