What is the difference between ICD 9 and ICD 10?
The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started. The ICD-9-CM consists of: a tabular list containing a numerical list of the disease code numbers in tabular form; an alphabetical index to the disease entries; and
What does ICD-9 stand for?
The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) is based on the World Health Organization's Ninth Revision, International Classification of Diseases (ICD-9). ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States.
What is the format for ICD 9 diagnosis codes?
The format for ICD-9 diagnoses codes is a decimal placed after the first three characters and two possible add-on characters following: xxx.xx. ICD-9 PCS were used to report procedures for inpatient hospital services from Volume 3, which represent procedures that were done at inpatient hospital facilities.
How many chapters are in the ICD 9 cm?
ICD-9-CM Chapters. The 2016 edition of the ICD-9-CM is divided into 19 chapters, based on the subject of the ICD codes each chapter contains. Each chapter is identified by a chapter number and description.

What does cardiac pacemaker in situ?
If you need to have a pacemaker fitted, a small electrical device called a pacemaker will be surgically implanted in your chest. The pacemaker sends electrical pulses to your heart to keep it beating regularly and not too slowly.
How do I find ICD-9 codes?
ICD9Data.com takes the current ICD-9-CM and HCPCS medical billing codes and adds 5.3+ million links between them. Combine that with a Google-powered search engine, drill-down navigation system and instant coding notes and it's easier than ever to quickly find the medical coding information you need.
What are ICD-9 10 and CPT codes?
ICD-10-CM diagnosis codes provide the reason for seeking health care; ICD-10-PCS procedure codes tell what inpatient treatment and services the patient got; CPT (HCPCS Level I) codes describe outpatient services and procedures; and providers generally use HCPCS (Level II) codes for equipment, drugs, and supplies for ...
What is the ICD-9 code for follow up visit?
V67.99 for Unspecified follow-up examination is a medical classification as listed by WHO under the range -PERSONS ENCOUNTERING HEALTH SERVICES IN OTHER CIRCUMSTANCES (V60-V69).
Where can I find a list of ICD-10 codes?
ICD-10 CM Guidelines, may be found at the following website: https://www.cdc.gov/nchs/icd/Comprehensive-Listing-of-ICD-10-CM-Files.htm.
Are ICD-9 codes still used in 2021?
CMS will continue to maintain the ICD-9 code website with the posted files. These are the codes providers (physicians, hospitals, etc.) and suppliers must use when submitting claims to Medicare for payment.
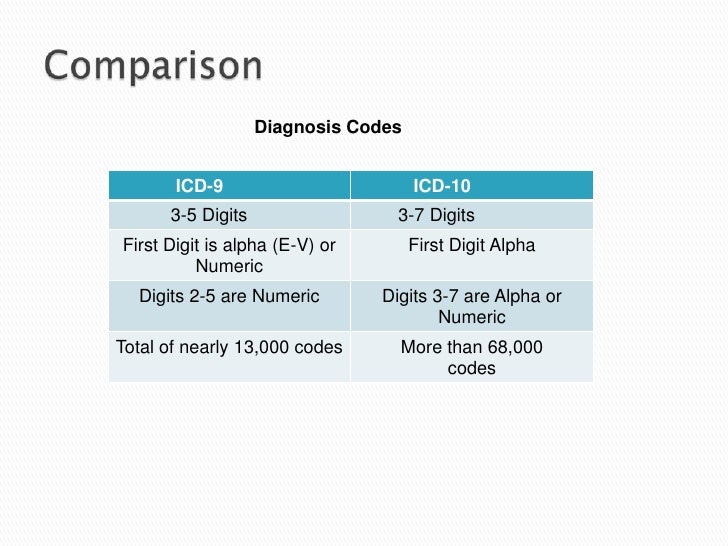
How is ICD-9 different from ICD-10?
ICD-9 uses mostly numeric codes with only occasional E and V alphanumeric codes. Plus, only three-, four- and five-digit codes are valid. ICD-10 uses entirely alphanumeric codes and has valid codes of up to seven digits.
What is an ICD-10 diagnosis code?
Used for medical claim reporting in all healthcare settings, ICD-10-CM is a standardized classification system of diagnosis codes that represent conditions and diseases, related health problems, abnormal findings, signs and symptoms, injuries, external causes of injuries and diseases, and social circumstances.
How do you write ICD-10 codes?
ICD-10-CM is a seven-character, alphanumeric code. Each code begins with a letter, and that letter is followed by two numbers. The first three characters of ICD-10-CM are the “category.” The category describes the general type of the injury or disease. The category is followed by a decimal point and the subcategory.
What is the CPT code for follow up visit?
Follow-up visits, like initial visits, should be coded using the appropriate evaluation and management (E/M) code (i.e., 99211–99215). Given the limited interaction with the patient and limited work involved, the level of service is likely to be low (e.g., 99211 or 99212).
When should ICD-10 code Z09 be used?
ICD-10 code Z09 for Encounter for follow-up examination after completed treatment for conditions other than malignant neoplasm is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What does ICD-9 stand for?
International Classification of Diseases, Ninth RevisionICD - ICD-9 - International Classification of Diseases, Ninth Revision. × Search NCHS. Search NCHS All CDC. National Center for Health Statistics.
What is PM in diagnostics?
This Program Memorandum (PM) clarifies our current coding guidelines for reporting diagnostic tests. Specifically, this PM clarifies the reporting of the International Classification of Diseases,Ninth Revision, Clinical Modification (ICD-9-CM) codes for diagnostic tests.
What is the code for a pathologist?
The pathologist is a physician and if a diagnosis is made it can be coded. It is appropriate for thepathologist to code what is known at the time of code assignment. For example, if the pathologisthas made a diagnosis of basal cell carcinoma, assign code 173.3, Other malignant neoplasm of skin,skin of other and unspecified parts of face. If the pathologist had not come up with a definitivediagnosis, it would be appropriate to code the reason why the specimen was submitted, in thisinstance, the skin lesion of the cheek.
What is the code for a malignant neoplasm of bladder?
The laboratory should report code 188.9, Malignant neoplasm of bladder, Bladder, part unspecified.It is appropriate to code the carcinoma, in this instance, because the cytology report wasauthenticated by the pathologist and serves as confirmation of the cell type, similar to a pathologyreport. The referring physician should report code 599.7, Hematuria, if the result of the cytologicalanalysis is not known at the time of code assignment.
What does it mean when a physician confirms a diagnosis?
If the physician has confirmed a diagnosis based on the results of the diagnostic test, thephysician interpreting the test should code that diagnosis. The signs and/or symptoms thatprompted ordering the test may be reported as additional diagnoses if they are not fullyexplained or related to the confirmed diagnosis.
What is a Medicare diagnostic order?
As further indicated in 42 CFR 410.32 all diagnostic tests “must be ordered by the physician who is treating the beneficiary.” As defined in §15021 of the Medicare Carrier Manual (MCM), an“order” is a communication from the treating physician/practitioner requesting that a diagnostictest be performed for a beneficiary. An order may include the following forms ofcommunication:
Popular Posts:
- 1. icd 10 code encounter for med refill
- 2. icd 10 code for medication no longer needed
- 3. icd 10 code for sacral ulcer stage 2
- 4. icd 10 code for follow up visit for diabetes
- 5. icd 10 code for mass of right breast
- 6. icd 10 code for rental stone
- 7. icd-10 code for myofascial pain
- 8. icd 10 cm code for a fib
- 9. icd 10 code for left femoral back fracture nondisplaced
- 10. icd 10 code for r03