What is the ICD 10 code for preventive visit new patient?
CPT CODE 99381, 99382 - 99385 - Preventive visit new patient - Medical Billing and Coding - Procedure code, ICD CODE.
What is the coverage of preventive visits?
Coverage of preventive visits varies by insurer, so it is important to be aware of the patient’s health plan. Most plans limit the frequency of the preventive visit to once a year, and not all tests are covered. Fecal occult blood tests, audiometry, Pap smear collection, and vaccines and their administration should be billed separately.
Is there a guide to Medicare coding for preventive services?
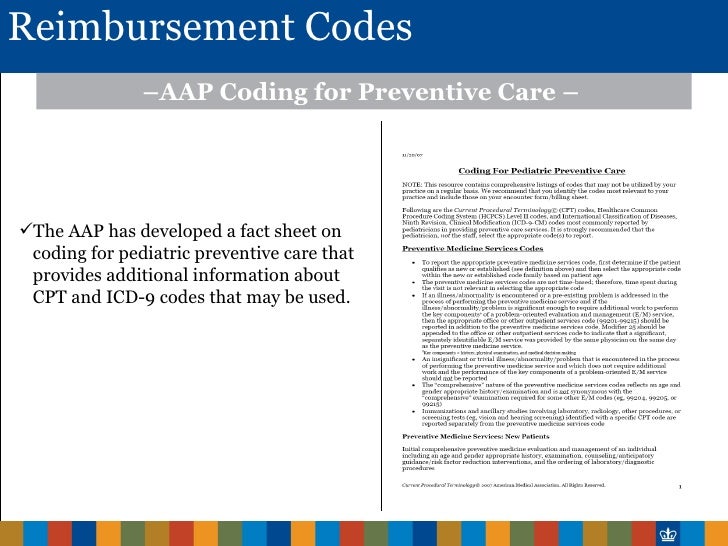
Download the AMA's guide on Medicare coding for preventive services that do not incur patient cost-sharing. It is critical that physicians and other health care providers clearly communicate to payers through careful documentation and coding for health care items and services.
How do I code for preventive services covered under the ACA?
To obtain insurance payments for preventive services covered under the ACA, you must properly code the combination of CPT/HCPCS and ICD-10 codes. For help with that, see “ Modifier 33 and more .”
How do you code preventive visits?
Preventive visit codes 99381-99397 include “counseling/anticipatory guidance/risk factor reduction interventions,” according to CPT. However, when such counseling is provided as part of a separate problem-oriented encounter, it may be billed using preventive medicine codes 99401-99409.
What is the ICD 10 code for preventive care visit?
The adult annual exam codes are as follows: Z00. 00, Encounter for general adult medical examination without abnormal findings, Z00.
What is the ICD 9 code for an annual physical?
V70. 0 Routine medical exam - ICD-9-CM Vol.
What is the difference between Z00 00 and Z00 01?
Use code Z00. 01 as the primary code as well as the codes for the chronic condition(s). When to use code Z00. 00: Patient presents for an Annual Wellness Visit (AWV).
What is the ICD 10 code for medical screening exam?
ICD-10 Code for Encounter for general adult medical examination without abnormal findings- Z00. 00- Codify by AAPC.
What is the ICD 10 code for Medicare Annual Wellness visit?
G0439 Annual Wellness Visit, Subsequent (AWV) Annual Wellness Visits can be for either new or established patients as the code does not differentiate. The initial AWV, G0438, is performed on patients that have been enrolled with Medicare for more than one year.
How do you code an annual wellness visit?
AWV Coding. The two CPT codes used to report AWV services are: G0438 initial visit. G0439 subsequent visit.
How do you code an annual physical exam?
Physical Exam CPT Codes For New Patients CPT 99381: New patient annual preventive exam (younger than 1 year). CPT 99382: New patient annual preventive exam (1-4 years). CPT 99383: New patient annual preventive exam (5-11 years). CPT 99384: New patient annual preventive exam (12-17 years).
Can you bill an office visit with an annual wellness visit?
A - Yes. Traditional Medicare and all managed Medicare plans will accept the G codes for AWVs. Q - Can I bill a routine office visit with a Medicare AWV? A - When appropriate, a routine office visit (9920X and 9921X) may be billed with a Medicare AWV.
What does code Z12 11 mean?
A screening colonoscopy should be reported with the following International Classification of Diseases, 10th edition (ICD-10) codes: Z12. 11: Encounter for screening for malignant neoplasm of the colon.
When should Z00 00 be used?
A: Z00. 00 (Encounter for general adult medical examination without abnormal findings) would be appropriate since there are no new findings at the visit. You should also bill the chronic stable conditions (i.e., hypertension and diabetes) along with the Z00.
What does code Z12 31 mean?
For example, Z12. 31 (Encounter for screening mammogram for malignant neoplasm of breast) is the correct code to use when you are ordering a routine mammogram for a patient.
When should a physician report CPT code?
Physicians should report CPT code, for developmental screening or other similar screening or testing, separate and distinct from the Preventive medicine service only when the testing or screening results in an interpretation and report by the physician being entered into the medical record.
When a physician furnishes a Medicare beneficiary a covered visit at the same place and on the same occasion
When a physician furnishes a Medicare beneficiary a covered visit at the same place and on the same occasion as a noncovered preventive medicine service (CPT codes 99381- 99397), consider the covered visit to be provided in lieu of a part of the preventive
What is preventive medicine?
A: Counseling, anticipatory guidance and risk factor reduction interventions are integral to a Preventive Medicine visit. Historical information may be obtained either through direct questioning or through completion of a written questionnaire. The responses on a questionnaire often identify areas for more focused interventions or treatments. Since this screening is part of a Preventive Medicine service, it is not reimbursed separately. Occasionally, a screening instrument requires interpretation, scoring, and the development of a report separate from the Preventive Medicine encounter. In those situations, where a CPT code exists for that service, screening, interpretation and development of a report is reimbursed separately from a Preventive Medicine service.
What is CPT code 99381?
Preventive Medicine Services [Current Procedural Terminology (CPT®) codes 99381-99387, 99391-99397, Healthcare Common Procedure Coding System (HCPCS) code G0402] are comprehensive in nature, reflect an age and gender appropriate history and examination, and include counseling, anticipatory guidance, and risk factor reduction interventions, usually separate from disease-related diagnoses. Occasionally, an abnormality is encountered or a preexisting problem is addressed during the Preventive visit, and significant elements of related Evaluation and Management (E/M) services are provided during the same visit. When this occurs, Oxford will reimburse Preventive Medicine service plus 50% the Problem-Oriented E/M service code when that code is appended with modifier 25. If the Problem-Oriented service is minor, or if the code is not submitted with modifier 25 appended, it will not be reimbursed.
What is a periodic comprehensive preventive medicine?
Periodic comprehensive preventive medicine re-evaluation and management of an individual, including an age- and gender-appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of appropriate immunizations, laboratory/diagnostic procedures for an established patient.
What is preventive medicine evaluation?
Initial comprehensive preventive medicine evaluation and management of an individual including an age- and gender-appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of appropriate immunizations, laboratory/diagnostic procedures for a new patient.
What is a 99381?
99381 – Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; infant (age younger than 1 year)
What is the AMA coding guide?
The AMA offers coding guides that helps physicians ensure that they are coding services correctly to be eligible for zero-dollar coverage. Explore the AMA's interactive coding guides or download guides for reference.
When to use modifier 33?
For instance, in 2015, Medicare announced that modifier 33 may be used when anesthesia is furnished in conjunction with a screening colonoscopy. In addition, in 2016, Medicare mandated the use of modifier 33 with Advance Care Planning services when provided on the same day as Annual Wellness Visits, so that any coinsurance and deductibles are waived.
What happens if you don't specify modifier 33?
If physicians and other health care providers do not specify modifier 33, the insurance plan may think that the preventive service was for a patient who is not eligible for the zero-dollar benefit, and the patient may be billed. To be eligible for the zero-dollar benefit, patients must fall within the evidence-based recommendations provided by ...
Does insurance cover preventive services?
Preventive services coding guides. Due to the Affordable Care Act (ACA), when physicians order certain evidence-based preventive services for patients, the insurance company may cover the cost of the service, with the patient having no cost-sharing responsibility (zero-dollar). The ACA requires that most private insurance plans provide zero-dollar ...
Does Medicare require modifier 33?
In addition, in 2016, Medicare mandated the use of modifier 33 with Advance Care Planning services when provided on the same day as Annual Wellness Visits, so that any coinsurance and deductibles are waived. Several preventive services covered by Medicare do not have a USPSTF recommendation grade of A or B.

Popular Posts:
- 1. icd 9 code for femoral artery stenosis
- 2. billable icd 9 code for diabetes type 2
- 3. icd 10 code for klinefelter syndrome
- 4. icd 10 code for hypersexual behavior
- 5. icd 10 code for cavitary lung lesion
- 6. icd 10 code for dysfunctional bladder
- 7. icd 9 code for hyperopia
- 8. 2017 icd 10 code for heterotopic gray matter and closed lip schizencephaly changes
- 9. icd 10 code for hx cad with cabg
- 10. icd 10 code for history of sbo