What is the ICD 9 code for venous thrombosis?
Short description: VENOUS THROMBOSIS NOS. ICD-9-CM 453.9 is a billable medical code that can be used to indicate a diagnosis on a reimbursement claim, however, 453.9 should only be used for claims with a date of service on or before September 30, 2015.
What is the ICD 10 code for prosthetic thrombosis?
Thrombosis due to vascular prosthetic devices, implants and grafts, initial encounter. T82.868A is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2019 edition of ICD-10-CM T82.868A became effective on October 1, 2018.
What is suspected stent thrombosis?
Suspected stent thrombosis is an emergent condition which needs to be handled like any acute myocardial infarction. Laboratory studies (i.e., CBC, chemistry, cardiac enzymes) can be obtained at the time of patient presentation, but they should not slow referral to the catheterization laboratory.
What is the ICD 10 code for stent placement?
T82.855A Stenosis of coronary artery stent, initial encounter T82.857A Stenosis of other cardiac prosthetic devices, implants and grafts, initial encounter T82.867A Thrombosis due to cardiac prosthetic devices, implants and grafts, initial encounter
What is a stent thrombosis?
Stent thrombosis is a thrombotic occlusion of a coronary stent. This is usually an acute process in contrast to restenosis, which is a gradual narrowing of the stent lumen due to neointimal proliferation. Stent thrombosis often results in an acute coronary syndrome, while restenosis often results in anginal symptoms. Stent thrombosis is further defined according to the following characteristics: 1 Timing: early (within 1 month), late (from 1 to 12 months), and very late (more than 12 months). Timing is also sometimes categorized as acute (within 24 hours) or subacute (more than 24 hours). 2 Clinical scenario: stent thrombosis usually results in symptoms of an acute coronary syndrome; however, it can occasionally be clinically silent. 3 Underlying stent: bare-metal stent versus first generation drug-eluting stent versus second-generation drug-eluting stent thrombosis.
Why is stent thrombosis not reported?
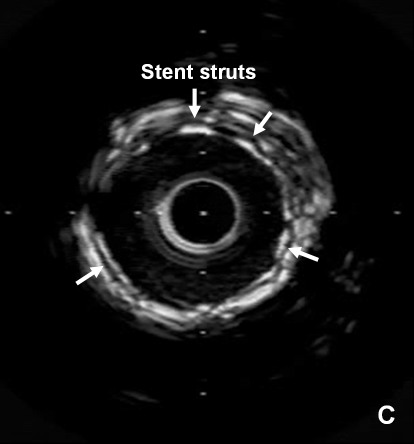
Likely in the majority of cases, this is due to lack of antiplatelet therapy . This is especially a concern in the perioperative period. Other reasons for stent thrombosis can lie with the stent itself, such as stent underexpansion or malapposition (acute or delayed). This would only be discerned by intravascular ultrasound or optical coherence tomography, which should be considered in all cases of stent thrombosis.
What is the management of a stent?
The immediate management of stent thrombosis is the same as the management of an acute coronary syndrome. Patients who present with a non-ST-elevation acute coronary syndrome are usually managed invasively accordingly to local practice patterns. For example, these patients would usually undergo urgent catheterization. Medical management consists of antiplatelet therapy (i.e., aspirin, and an ADP receptor antagonist), antithrombin therapy (i.e., heparin or direct thrombin inhibitor), statin, beta-blocker, and nitroglycerin. Patients who present with an ST-elevation acute coronary syndrome should undergo emergent reperfusion therapy according to local practice patterns (i.e., normally by primary PCI). Successful reperfusion of an acute myocardial infarction from stent thrombosis is less likely than for acute myocardial infarction due to native artery/plaque rupture. Supportive medical therapy is the same as for non-ST-elevation acute coronary syndrome.
How often do stents thrombosis occur?
With bare-metal stents, most stent thromboses occur within the first month of implant at a frequency <1%.
How long should I keep aspirin after a stent?
Therefore, antiplatelet agents should be held for the shortest possible duration (i.e., not longer than 7 days).
What is a thrombus 5 mm proximal to the stent?
Definite stent thrombosis: a patient with clinical signs or symptoms of an acute coronary syndrome and angiographic or autopsy evidence of a thrombus 5 mm proximal or distal to the stent.
Which receptor antagonist raises the likelihood of stent thrombosis?
A consideration which raises the likelihood of stent thrombosis is recent termination of an adenosine diphosphate (ADP) receptor antagonist (i.e., clopidogrel, prasugrel, or ticagrelor) and/or aspirin.
Is distal embolic protection billable?
The deployment of a device for distal embolic protection during an interventional procedure is considered part of the more complex procedure and is not separately billable.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.

Definition
- Stent thrombosis is a thrombotic occlusion of a coronary stent. This is usually an acute process in contrast to restenosis, which is a gradual narrowing of the stent lumen due to neointimal proliferation. Stent thrombosis often results in an acute coronary syndrome, while restenosis often results in anginal symptoms. Stent thrombosis is further def...
Contraindications
- Any patient with prior percutaneous coronary intervention who presents with signs/symptoms consistent with an acute coronary syndrome, especially when there is ischemia in the territory of the prior stent, should be considered for stent thrombosis. A consideration which raises the likelihood of stent thrombosis is recent termination of an adenosine diphosphate(ADP) receptor …
Prognosis
- While stent thrombosis can be a devastating event, fortunately it is a rare problem after percutaneous coronary intervention (PCI). With bare-metal stents, most stent thromboses occur within the first month of implant at a frequency <1%. Patients who suffer from stent thrombosis have a poor prognosis. Up to two thirds of patients who have stent thrombosis will die or have a …
Epidemiology
- Events beyond 6 months are exceedingly rare. With first generation drug-eluting stents, early events occur at the same low frequency as bare-metal stents. First generation drug-eluting stents (paclitaxel-eluting and sirolimus-eluting) have a higher rate of late and especially very late stent thrombosis compared with bare-metal stents. Some registries have documented this event rate …
Symptoms
- Since stent thrombosis patients present with an acute coronary syndrome, they may have signs/symptoms of heart failure or cardiogenic shock.
Diagnosis
- The electrocardiogram is a first-line test in any patient with a chest pain syndrome. Ischemia in the territory of a prior stent is supportive stent thrombosis; however, the patient may also have progression of disease upstream or downstream of the stented segment, which would not be due to stent thrombosis per se. A silent electrocardiogram in a patient with chest pain and prior sten…
Management
- The management of stent thrombosis is the same as the management of an acute coronary syndrome. The immediate management of stent thrombosis is the same as the management of an acute coronary syndrome. Patients who present with a non-ST-elevation acute coronary syndrome are usually managed invasively accordingly to local practice patterns. For example, th…
Signs and symptoms
- The physical examination is nonspecific with stent thrombosis; however, there may be findings of heart failure (i.e., rales, elevated jugular venous distention, hypotension, etc.).
Risks
- The perioperative period can pose unique risks to patients with coronary stents. The following recommendations are taken from the American College of Cardiology/American Heart Association:
Treatment
- For emergent/urgent surgeries, it is recommended that patients proceed to the operating room on dual antiplatelet therapy. The question of using a glycoprotein IIb/IIIa inhibitor as a bridge often comes up as a mechanism to perform surgery sooner than 12 months.
Prevention
- Since most stent thromboses occur in the perioperative or postoperative period rather than the preoperative period, a preoperative glycoprotein IIb/IIIa inhibitor bridge is likely ineffective at preventing thrombotic events. Therefore, there are no guideline recommendations endorsing the use of a glycoprotein IIb/IIIa inhibitor bridge. An unfractionated heparin (or low-molecular weigh…
Clinical significance
- Patient noncompliance is an important comorbidity thatmay have resulted in the stent thrombosis. For example, such a patient may not have taken the recommended aspirin/ADP receptor antagonist. This history might influence if an additional stent is used during PCI for the stent thrombosis and if an additional stent is used, a bare-metal stent might be a better choice.
Interactions
- Lack of adequate antiplatelet therapy during this early period increases the risk of stent thrombosis. Examples of inadequate antiplatelet therapy would be aspirin without a periprocedural glycoprotein IIb/IIIa inhibitor or an adenosine diphosphate (ADP) receptor antagonist (i.e., clopidogrel, prasugrel, or ticagrelor).
Medical uses
- After bare-metal stent PCI, aspirin is recommended for life and an ADP receptor antagonist for a minimum of 4 to 6 weeks and ideally up to 12 months. Early drug-eluting stent thrombosis shares the same predictors of early bare-metal stent thrombosis.
Cause
- Late and very late stent thrombosis is usually due to the type of stent (i.e., first generation drug-eluting) and antiplatelet therapy (i.e., premature termination of ADP receptor antagonist within 6 months or complete termination of antiplatelet agents at any time). As mentioned previously, late stent thrombosis of a bare-metal stent is exceedingly rare and based on available data, stent thr…
Characteristics
- For completeness, the following other characteristics have been associated with late stent thrombosis: acquired incomplete stent apposition, diabetes, small vessels/small stents, long stent length/multiple stents, stent underexpansion, renal failure, acute coronary syndrome at the index procedure, bifurcation lesion, left ventricular dysfunction, residual disease in the culprit vessel, le…
Funding
- No sponsor or advertiser has participated in, approved or paid for the content provided by Decision Support in Medicine LLC. The Licensed Content is the property of and copyrighted by DSM.
Popular Posts:
- 1. icd 10 code for necrotizing cellulitis of foot
- 2. icd 10 code for sprain toe
- 3. icd 10 code for paraplegia unspecified
- 4. icd 10 code for left incarcerated inguinal hernia
- 5. icd 10 data code for left shoulder strain
- 6. icd 10 code for post void dribbling
- 7. icd 10 code for druj instability
- 8. icd 10 code for left scapular contusion
- 9. icd 10 code for ludwigs angina
- 10. icd 10 code for breast cancer return