How to recognize toenail fungus?
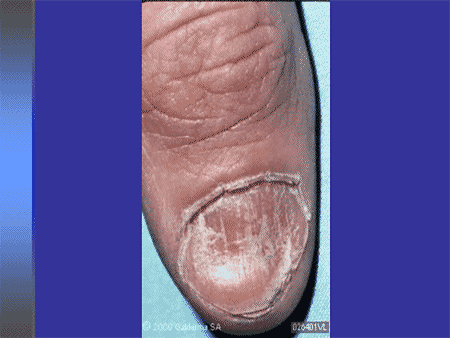
You may have nail fungus if one or more of your nails are:
- Thickened
- Whitish to yellow-brown discoloration
- Brittle, crumbly or ragged
- Distorted in shape
- A dark color, caused by debris building up under your nail
- Smelling slightly foul
How to get rid of fungus under the toenail?
Try One of These 10 Home Remedies for Toenail Fungus
- Vicks VapoRub. Vicks VapoRub is a topical ointment. ...
- Snakeroot extract. Snakeroot ( Ageratina pichinchensis) extract is an antifungal made from plants in the sunflower family.
- Tea tree oil. ...
- Oregano oil. ...
- Olive leaf extract. ...
- Ozonized oils. ...
- Vinegar. ...
- Listerine mouthwash. ...
- Garlic. ...
- Adjust your diet. ...
Do I need to go to the doctor for toenail fungus?
A dermatologist can give proper diagnosis on skin and nail conditions, and therefore will be able to identify the fungal infection and what type it is. To determine the cause of the problem and diagnose a fungal nail infection, the doctor may take a sample of the skin and nail fragments from the infected nail.
What is the diagnosis for toenail fungus?
Your doctor will first examine your toenails, but physical exam alone may be unreliable when it comes to diagnosing toenail fungus. Some conditions, such as psoriasis, hematoma (blood under the nail), and paronychia (skin infection), can mimic the symptoms of a fungal nail infection.
What is the ICD-10 code for toenail fungus?
ICD-10-CM Code for Tinea unguium B35. 1.
What is another name for tinea Unguium?
Tinea unguium is a common type of fungal infection. It is also called onychomycosis. The fungus infects the fingernails and, more commonly, the toenails.
What is the medical term for toenail fungus?
Definition. Fungal nail infections are common infections of the fingernails or toenails that can cause the nail to become discolored, thick, and more likely to crack and break. Infections are more common in toenails than fingernails. 1. The technical name for a fungal nail infection is “onychomycosis.”
What is the ICD-10 code for fungal infection?
B49 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM B49 became effective on October 1, 2021. This is the American ICD-10-CM version of B49 - other international versions of ICD-10 B49 may differ.
What is the difference between onychomycosis and tinea unguium?
Onychomycosis is a fungal infection of the nail unit. When onychomycosis is caused by dermatophytes, it is called tinea unguium. The term onychomycosis encompasses not only the dermatophytes but the yeasts and saprophytic molds infections as well.
What is the difference between tinea pedis and tinea unguium?
Tinea unguium was defined as a positive direct examination with potassium hydroxide and culture of the etiological agent from subjects with clinically abnormal nails. Patients with positive dermatophyte cultures of foot specimens were considered to have tinea pedis.
What are the different types of toenail fungus?
There are three main types of toenail fungus: subungual onychomycosis, white superficial onychomycosis, and candida onychomycosis. These different types of onychomycosis are defined by the nature of the fungus.
What is the main cause of toenail fungus?
Tiny, microscopic organisms called fungi (the plural of fungus) cause a fungal nail infection. Many people pick up the fungi when they have skin-to-skin contact with someone who has a fungal infection such as athlete's foot or ringworm on their hands.
What is tinea pedis and onychomycosis?
Tinea pedis is the infection of the skin of the foot with fungus and must be distinguished from other causes of scaling rashes of the hands and feet. Tinea unguium (onychomycosis) is the infection of the nail unit with fungus where the fungus may be in one or more of the component structures of the nail unit.
What is the ICD-10 code for B35 9?
Dermatophytosis, unspecifiedICD-10 code B35. 9 for Dermatophytosis, unspecified is a medical classification as listed by WHO under the range - Certain infectious and parasitic diseases .
What is ICD-10 code for tinea pedis?
ICD-10 code: B35. 3 Tinea pedis | gesund.bund.de.
What b37 9?
9: Candidiasis, unspecified.
What does tinea unguium look like?
A brownish or whitish-yellow nail color often signals toenail fungal infection. The infection can be painful and may cause toenails to become thick, brittle, or to change shape. The big toenail is most likely to be infected with nail fungus.
How do you get tinea unguium?
You are more likely to get tinea unguium if you:Have another fungal infection, such as athlete's foot.Have sweaty feet.Share nail clippers with a person who has a fungal infection.Swim often.Walk barefoot in damp areas, such as locker rooms.Use communal or shared showers.Wear artificial nails.
What dermatological condition is usually associated with tinea unguium?
Nail Disease 13), or tinea unguium, is a fungal or yeast infection of the nail, usually caused by Tinea rubrum, Tinea mentagrophytes, or Candida albicans. Onychomycosis is the most common nail disorder. Predisposing factors for infection include heat, moisture, trauma, diabetes mellitus, and tinea pedis.
How do you deal with tinea unguium?
Treatment. Mild infections affecting less than 80% of one or two nails may respond to topical antifungal medications but cure usually requires an oral antifungal medication. Fingernail infections are usually cured more quickly and effectively than toenail infections.
What is a fungal infection of the nail?
A fungal infection of the nail, usually caused by dermatophytes; yeasts; or nondermatophyte molds. Reimbursement claims with a date of service on or after October 1, 2015 require the use of ICD-10-CM codes.
When will the ICD-10 B35.1 be released?
The 2022 edition of ICD-10-CM B35.1 became effective on October 1, 2021.
How to get rid of fungus on nails?
Medicated nail cream. Your doctor may prescribe an antifungal cream, which you rub into your infected nails after soaking. These creams may work better if you first thin the nails. This helps the medication get through the hard nail surface to the underlying fungus.
How to reduce pain from nail fungus?
Trim and thin the nails. This helps reduce pain by reducing pressure on the nails. Also, if you do this before applying an antifungal, the drug can reach deeper layers of the nail. Before trimming or using a nail file to thin thick nails, soften them with urea-containing creams.
How to get rid of white spots on nails?
Try over-the-counter antifungal nail creams and ointments. Several products are available. If you notice white markings on the surfaces of the nails, file them off, soak your nails in water, dry them, and apply the medicated cream or lotion.
How long do you need to use nail polish?
After seven days, you wipe the piled-on layers clean with alcohol and begin fresh applications. You may need to use this type of nail polish daily for almost a year. Medicated nail cream. Your doctor may prescribe an antifungal cream, which you rub into your infected nails after soaking.
What causes a nail to get infected?
He or she may also take some nail clippings or scrape debris from under your nail and send the sample to a lab to identify the type of fungus causing the infection. Other conditions, such as psoriasis, can mimic a fungal infection of the nail. Microorganisms such as yeast and bacteria also can infect nails. Knowing the cause of your infection helps ...
How long does it take for a fungus to go away?
It may take four months or longer to eliminate an infection. Treatment success rates with these drugs appear to be lower in adults over age 65. Oral antifungal drugs may cause side effects ranging from skin rash to liver damage. You may need occasional blood tests to check on how you're doing with these types of drugs.
Can you take antifungal medication on your nails?
Your doctor may prescribe antifungal drugs that you take orally or apply to the nail. In some situations, it helps to combine oral and topical antifungal therapies.
What is a disorder of nail?
Disorder of nail. Nail disease. Clinical Information. Diseases of the nail plate and tissues surrounding it. The concept is limited to primates. Your toenails and fingernails protect the tissues of your toes and fingers. They are made up of layers of a hardened protein called keratin, which is also in your hair and skin.
When will the ICD-10-CM L60.9 be released?
The 2022 edition of ICD-10-CM L60.9 became effective on October 1, 2021.
What is the ICD-10 code for dermatophytosis of the nail?
110.1 is a legacy non-billable code used to specify a medical diagnosis of dermatophytosis of nail. This code was replaced on September 30, 2015 by its ICD-10 equivalent.
What are the health benefits of toenails?
The health of your nails can be a clue to your overall health. Healthy nails are usually smooth and consistent in color. Specific types of nail discoloration and changes in growth rate can be signs of lung, heart, kidney, and liver diseases, as well as diabetes and anemia. White spots and vertical ridges are harmless.
What is a code also note?
Code also note - A "code also" note instructs that two codes may be required to fully describe a condition, but this note does not provide sequencing direction.
What does NOS mean in a syllable?
NOS "Not otherwise specified" - This abbreviation is the equivalent of unspecified.
Where do fungal infections start?
You can inhale the spores or they can land on you. As a result, fungal infections often start in the lungs or on the skin. You are more likely to get a fungal infection if you have a weakened immune system or take antibiotics.
Can you remove a nail?
Keeping your nails clean, dry, and trimmed can help you avoid some problems. Do not remove the cuticle, which can cause infection.
Can fungi cause athlete's foot?
If you have ever had athlete's foot or a yeast infection, you can blame a fungus. A fungus is a primitive organism. Mushrooms, mold and mildew are examples. Fungi live in air, in soil, on plants and in water. Some live in the human body. Only about half of all types of fungi are harmful.

Overview
- Icd 9 Code For Onychomycosis Of Toenail A nail fungus causes thickened, brittle, crumbly, or ragged nails. Usually, the problems caused by this condition are cosmetic. The main symptoms are changes in the appearance of nails. If you are experiencing toenail fungus, changing your dietmay be a good idea. This condition is often resistant to topical m...
What You Need to Know About Onychomycosis
- Onychomycosis is the scientific name for nail fungus. The condition can be caused by a number of things, such as an injury to the nail. A weakened immune system makes it difficult to fight off the fungi. Diabetes also increases the risk of fungal nail infections. These treatments are often painful and require several months of treatment. Usually, the best option for treating nail fungus …
The Initial Causes Icd 9 Code For Onychomycosis of Toenail
- If you suspect that your nails are infected with fungus, it is best to consult your doctor and get a diagnosis. Your doctor will ask you about the symptoms and conduct a thorough examination of your nails. A biopsy is required to determine the cause of the infection. Various types of fungus are found in the skin, including the toenails. Among the most common forms of nail fungus are y…
Treatment
- Oral antifungal supplements are the first choice of treatment for toe fungus. Although oral antifungal drugs are usually the most effective, they can also interact with other medications and take a long time to work. In addition to oral drugs, you can use olive leaf salve or apply a topical solution directly to the infected area. Both of these methods are effective, but they can take mon…
Final Thoughts
- If the toenail fungus is severe, you can use prescription medications. A doctor can prescribe these medications or recommend over-the-counter medications. The recommended treatments for toe fungus are oral and can be found here. The most effective treatment is what they use in space in the space station. You can also try medicated nail polishes to treat the fungus. If you’re not satis…
Popular Posts:
- 1. icd code for hammertoes
- 2. icd 10 code for requesting vasectomy
- 3. what is the icd 10 code for status peritoneal dialysis catheter
- 4. icd 10 code for left sided obstructive uropathy
- 5. icd 10 code for factor 8 deficiency
- 6. icd 10 code for repatha injection
- 7. icd-10 code for agranulocytosis due to infection
- 8. icd-10 code for bereavement unspecified
- 9. icd 9 code for sprain strain right index finger
- 10. icd 10 code for sweet's syndrome