What are the new ICD 10 codes?
The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code XW023X7), and the infusion of other new technology monoclonal antibody (code XW023Y7).
What is the CPT code for transition of care?
CPT ® Code Descriptions 99495- Transitional Care Management services with the following required elements: Communication (direct contact, telephone, electronic) with the patient and/or caregiver
What is transition of care?
- Health Homes
- Person-Centered Hospital Discharge Model
- Person-Centered Planning Grants
- State Profile Tool Grant
- Balancing Long Term Services & Supports
- Integrating Care
- Employment Initiatives
- Institutional Long Term Care
- Money Follows the Person
- PACE
What does ICD - 10 stand for?
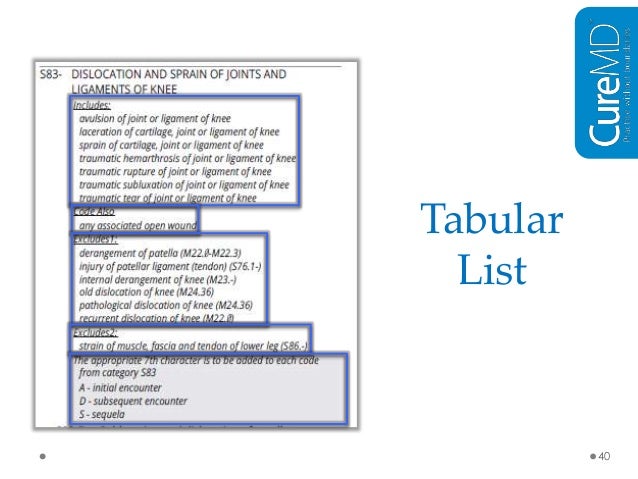
The ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) is a system used by physicians and other healthcare providers to classify and code all diagnoses, symptoms and procedures recorded in conjunction with hospital care in the United States.
How do you code transition of care?
TCM Coding The two CPT codes used to report TCM services are: CPT code 99495 – moderate medical complexity requiring a face-to-face visit within 14 days of discharge. CPT code 99496 – high medical complexity requiring a face-to-face visit within seven days of discharge.
What is a transition of care visit?
It involves a medical professional engaging in one face-to-face visit with the patient and then additional non face-to-face meetings (such as by telephone or a video call, as is the case with telemedicine). The idea here is to ensure there are no gaps in patient care.
What is the CPT code for transfer of care?
Transfer of Care Code-CPT 99495 and 99496.
What is code Z71 89?
ICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
How does CMS define transition of care?
The Centers for Medicare & Medicaid Services (CMS) defines a transition of care as the movement of a patient from one setting of care to another.
What is transitional care in nursing?
Transitional care: Care involved when a patient/client leaves one care setting (i.e. hospital, nursing home, assisted living facility, SNF, primary care physician, home health, or specialist) and moves to another.
When a patient is transferred from one facility to another?
Transfer-Moving a patient from one unit to another (intra-agency transfer) or moving a patient from one healthcare facility to another(inter-agency transfer). Discharge-release of a patient from a health care facility.
Can an office visit be billed with transitional care?
You can bill it as an office visit if documentation requirements for history, exam, and medical decision making are met should the patient die or be re-admitted.
What is the difference between 99495 and 99496?
There are two codes used to reimburse for Transitional Care Management, CPT 99495 for moderate complexity patients and CPT 99596 for high complexity patients. A key difference between these codes is days after discharge in which a face-to-face visit is required, 14 days for CPT 99495 and 7 days for CPT 99496.
What is diagnosis code Z51 81?
ICD-10 code Z51. 81 for Encounter for therapeutic drug level monitoring is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
Can Z76 89 be used as a primary diagnosis?
The patient's primary diagnostic code is the most important. Assuming the patient's primary diagnostic code is Z76. 89, look in the list below to see which MDC's "Assignment of Diagnosis Codes" is first.
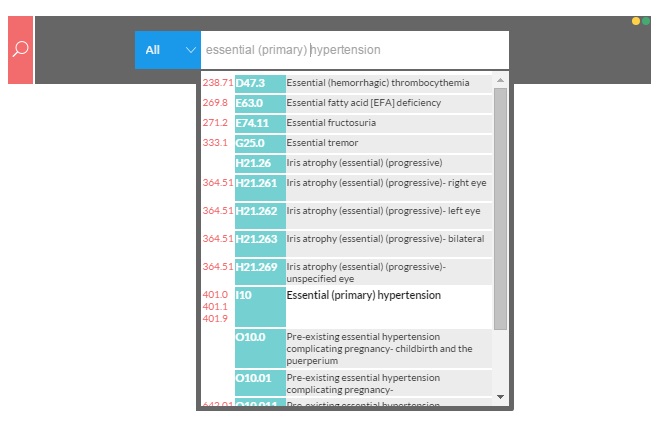
What is I10 diagnosis?
That code is I10, Essential (primary) hypertension. As in ICD-9, this code includes “high blood pressure” but does not include elevated blood pressure without a diagnosis of hypertension (that would be ICD-10 code R03. 0).
When should I bill my CMS?
Billing should occur at the conclusion of the 30-day post-discharge period. Now CMS put out on their website FAQ’s in 2018, saying that the date of the face to face can be the date the entire service is billed. But I would use caution and common sense here. Once all of the 30 days of service is met, then report the code. By reporting prior to the 30-day period, you run the risk of staff not finishing the tasks that are part of the code compliance.
When should medication reconciliation and management happen?
Medication reconciliation and management should happen no later than the face-to-face visit.
What is the CPT code for a face to face visit?
CPT Code 99496 covers the same code details, involves medical decision making of high complexity and a face-to-face visit within seven days of discharge. The work RVU is 3.05. or an approximate reimbursement of $109.80
How long does TCM last?
TCM commences upon date of discharge and then for the next 29 days. There is a combination of face to face and non-face to face services within this time frame. There has been some misinformation out there on the requirements to report these codes that has triggered some payer audits, so we wanted to clear up any confusion.
What is CPT service?
Per CPT, these services, “address any needed coordination of care performed by multiple disciplines and community service agencies. The reporting individual provides or oversees the management and/or coordination of services needed, for all medical conditions, psychosocial needs and activity of ADL support by providing first contact and continuous access”.
How often is TCM payable?
They are payable only once per patient in the 30 days following discharge, thus if the patient is readmitted TCM cannot be billed again.
What is transitional care management?
Transitional Care Management. There are three kinds of care for a Medicare patient after being an inpatient. They are Transitional Care, Chronic Care Management, and Complex Care Management. Each of these is a critical component of primary care that contributes to better health and care for beneficiaries.
What is CPT code 99496?
CPT® Code 99496 – Transitional Care Management services with the following required elements: Communication (direct contact, telephone, electronic) with the patient and/or caregiver within 2 business days of discharge; Medical decision-making of high complexity during the service period; Face-to-face visit, within 7 calendar days of discharge
How long is the TCM period?
The 30-day TCM period begins on the beneficiary's inpatient discharge date and continues for the next 29 days. The provider must furnish medication reconciliation and management on or before the date of your face-to-face visit.
What is TCM in healthcare?
Each of these is a critical component of primary care that contributes to better health and care for beneficiaries. Transitional care management (TCM) is the coordination and continuity of healthcare during a movement from one healthcare setting to either another or to home. It addresses the period between the inpatient stay and community setting.
Can you bill TCM if you have a face to face visit?
If the face-to-face visit is not within the required timeframe, you cannot bill TCM services (for more information, see the Face-to-Face Visit section). The provider must furnish non-face-to-face services to the beneficiary, unless you determine they are not medically indicated or needed.
Can you report TCM on the same day?
The required face-to-face visit may not take place on the same day you report discharge day management services.
What is TCM code?
The TCM codes are care management codes. As care management codes , auxiliary personnel may provide the non-face-to-face services of TCM under the general supervision of the physician or NPP subject to applicable state law, scope of practice, and the Medicare Physician Fee Schedule (PFS) “incident to” rules and regulations.
How long does chronic care management last?
Chronic care management services with the following required elements: multiple (two or more) chronic conditions expected to last at least 12 months, or until the death of the patient, chronic conditions place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline, comprehensive care plan established, implemented, revised, or monitored; first 20 minutes of clinical staff time directed by a physician or other qualified health care professional per calendar month
How many face to face visits are required for CPT?
You must provide 1 face-to-face visit within the timeframes described by these 2 CPT codes:
What to do if you make 2 unsuccessful attempts to get a TCM?
Report the service if you make 2 or more unsuccessful separate attempts in a timely manner. Document your attempts in the medical record if you meet all other TCM criteria. Continue trying
How long is the 30 day period for Medicare?
This booklet outlines transitional care services during the “30-day period,” which begins when a physician discharges the patient from an inpatient stay and continues for the next 29 days. Medicare may cover these services to
Who provides non-face-to-face services of TCM?
CNMs, CNSs, NPs, and PAs may also provide the non-face-to-face services of TCM incident to the services of a physician.
Can you bill TCM services?
If the face-to-face visit isn’t within the required timeframe, you can’t bill TCM services (see the Face-to-Face Visit
Popular Posts:
- 1. icd 9 code for personal history of polysubstance abuse
- 2. icd 10 code for hypoxic encephalopathy
- 3. icd 10 code for chronic compression fracture
- 4. icd 10 code for joint effusion left knee
- 5. icd 10 code for low vision both eyes
- 6. icd 9 code for bilirubin
- 7. icd 10 code for r03.0
- 8. icd 10 code for left upper cts
- 9. icd 10 code for lumbar mri without contrast
- 10. icd-10-cm code for hypothoyrodism