What is the ICD 10 code for vitreous body?
2007 ICD-9-CM Diagnosis Code 379.21 Vitreous degeneration ICD-9-CM 379.21 is a billable medical code that can be used to indicate a diagnosis on a reimbursement claim, however, 379.21 should only be used for claims with a date of service on or before September 30, 2015.
What is the ICD 10 code for posterior vitreous detachment?
Oct 01, 2021 · Vitreous floaters (eye condition) Vitreous opacities; Vitreous opacity (eye condition) ICD-10-CM H43.399 is grouped within Diagnostic Related Group(s) (MS-DRG v 39.0): 124 Other disorders of the eye with mcc; 125 Other disorders of the eye without mcc; Convert H43.399 to ICD-9-CM. Code History. 2016 (effective 10/1/2015): New code (first year of non …
What are the signs and symptoms of a spontaneous vitreous hemorrhage (PVD)?
Disorders of vitreous body (379.2) ICD-9 code 379.2 for Disorders of vitreous body is a medical classification as listed by WHO under the range -DISORDERS OF THE EYE AND ADNEXA (360-379). Subscribe to Codify and get the code details in …
What is the ICD 10 code for opacities in the eye?
Oct 01, 2021 · Vitreous degeneration, unspecified eye. H43.819 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM H43.819 became effective on October 1, 2021.
What is the ICD-10 code for vitreous Syneresis?
H43. 819 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM H43. 819 became effective on October 1, 2021.
What is the vitreous degeneration?
What is the ICD-10 code for PVD bilateral eyes?
What ICD-10 code(s) should be used There are two valid diagnoses: H43. 811 (Vitreous degeneration, right eye) and Z96. 1 (Presence of intraocular lens; pseudophakia).Jan 1, 2016
What happens when the vitreous separates from the retina?
What is vitreous made of?
Can vitreous humor be replaced?
What does vitreous Syneresis mean?
What is a vitreoretinal tuft?
What is the ICD-10 code for PVD?
Can stress cause vitreous detachment?
What can happen if someone has too much vitreous humor?
How long does it take for vitreous to detach?
What is a vitreous hemorrhage?
Vitreous hemorrhage: A hemorrhagic PVD (i.e. vitreous hemorrhage secondary to a PVD) can occur in about 7.5% of P VDs. This occurs when a retinal blood vessel is torn during vitreous separation. The risk of having an underlying retinal tear increases to nearly 70% in the case of a hemorrhagic PVD.
What is the term for the separation of the vitreous from the retina?
This is known as a rhegmatogenous retinal detachment. Typically, however, the vitreous separates without any ill effects on the retina.
What is the separation of the posterior vitreous detachment?
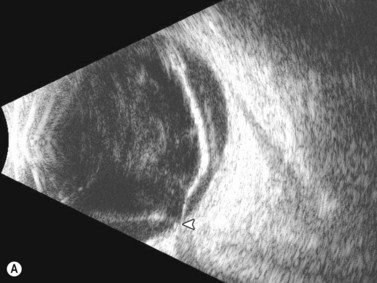
A posterior vitreous detachment (PVD) is defined as the separation of the posterior hyaloid face from the neurosensory retina. At birth, the vitreous "gel" fills the back of the eye and normally has Jello-like consistency. As one ages, the vitreous undergoes "syneresis," in which it becomes more fluid or liquid-like. The pockets of fluid in the vitreous cavity give the patient a sensation of "floaters" or "cobwebs." As the pockets of fluid collapse on themselves, they gently pull on the retina giving the patient a sensation of "flashes of light" or photopsias. Eventually, the vitreous may completely separate from the neurosensory retina, which is called a posterior vitreous detachment or "PVD" that is confirmed clinically with observation of Weiss ring on funduscopic examination. This usually occurs in one eye at a time, but a PVD in the contralateral eye often occur 6 to 24 months later (6). In high myopia, PVD develops increasingly with age and the degree of myopia (7). As the vitreous gel separates, it may cause a tear in the neurosensory retina which is fragile and thin like a piece of tissue paper. A retinal tear can allow the liquid part of the vitreous to escape behind the retina and separate the retina from its underlying attachments (and blood supply). This is known as a rhegmatogenous retinal detachment. Typically, however, the vitreous separates without any ill effects on the retina.
What is the risk of a PVD?
Patients are at greatest risk for a symptomatic PVD in the 5th to 7th decade of life, although it can occur much earlier. Most often patients are myopic (near-sighted). High myopes (i.e. refraction of -6.00 or greater) are at increased risk of complications related to a PVD due to thinning of the retina as it is stretched along a longer eye. Other predisposing risk factors for a PVD include a family history of retinal tears or detachments, intraocular inflammation (uveitis), trauma, and previous eye surgery.
What causes floaters in the retina?
They are caused by mechanical traction on the retina, caused by the vitreous gel "tugging" on the underlying neurosensory retina. Patients may also endorse new floaters. Generally these are described by patients as large, wispy objects moving around when they move their eye in different directions of gaze.
How long does it take for a PVD to develop?
Generally, an acute PVD develops suddenly, but becomes complete within weeks of onset of symptoms . A PVD is considered "partial" when the vitreous jelly is still attached at the macula/optic nerve head and "complete" once total separation of the jelly from the optic nerve head has occurred.
How long does it take for a scleral depressed exam to be completed?
sudden onset of many new floaters and/or flashes of lights), it is recommended the patient undergo a dilated fundus examination with complete 360 degree scleral depressed examination within 12-24 hours. The examiner should be an eye physician who feels confident in examining the peripheral retina, as this is typically where retinal tears and detachments originate. The examiner will likely examine both eyes thoroughly, even the asymptomatic eye, to ensure no pathology exists. Often times, having a tear in one eye may suggest a predisposition to having additional tears or retinal pathology in the same or contralateral eye. If an isolated retinal tear is found, laser demarcation will likely be advised. If a retinal detachment is present, immediate referral to a retina specialist is warranted.#N#If an evolving acute PVD is found without any retinal tears or detachments, it is commonly advised to have a follow-up scleral depressed examination approximately one month later. Follow-up varies based on severity, symptoms, and other risk factors. If the PVD is hemorrhagic, or other more concerning signs are present on exam, the examiner may recommend follow-up at more frequent intervals. Although there are no preventative measures, it is generally recommended that the patient avoids heavy exertion, lifting, or bending over in the setting of acute PVD with vitreous hemorrhage so that the blood in the vitreous cavity can settle inferiorly away from the center vision. Elevating the head of the bed will allow gravity to settle the blood inferiorly, out of the visual axis. Patients may continue their blood-thinning medications, as there is no evidence that the discontinuation of antiplatelet or anticoagulant agents speeds the recovery of vitreous hemorrhage.
Index to Diseases and Injuries
The Index to Diseases and Injuries is an alphabetical listing of medical terms, with each term mapped to one or more ICD-10 code (s). The following references for the code H43.89 are found in the index:
Approximate Synonyms
The following clinical terms are approximate synonyms or lay terms that might be used to identify the correct diagnosis code:
Convert H43.89 to ICD-9 Code
The General Equivalency Mapping (GEM) crosswalk indicates an approximate mapping between the ICD-10 code H43.89 its ICD-9 equivalent. The approximate mapping means there is not an exact match between the ICD-10 code and the ICD-9 code and the mapped code is not a precise representation of the original code.
Information for Patients
Some eye problems are minor and don't last long. But some can lead to a permanent loss of vision.
What are the causes of vision loss?
Eye Diseases. Some eye problems are minor and don't last long. But some can lead to a permanent loss of vision. Common eye problems include. Refractive errors. Cataracts - clouded lenses. Optic nerve disorders, including glaucoma. Retinal disorders - problems with the nerve layer at the back of the eye.
What causes pink eye?
Retinal disorders - problems with the nerve layer at the back of the eye. Macular degeneration - a disease that destroys sharp, central vision. Diabetic eye problems . Conjunctivitis - an infection also known as pinkeye. Your best defense is to have regular checkups, because eye diseases do not always have symptoms.
What are the common eye problems?
Common eye problems include. Refractive errors. Cataracts - clouded lenses. Optic nerve disorders, including glaucoma. Retinal disorders - problems with the nerve layer at the back of the eye. Macular degeneration - a disease that destroys sharp, central vision. Diabetic eye problems.
What is the best defense against eye diseases?
Diabetic eye problems. Conjunctivitis - an infection also known as pinkeye. Your best defense is to have regular checkups, because eye diseases do not always have symptoms. Early detection and treatment could prevent vision loss.
What is the GEM crosswalk?
The General Equivalency Mapping (GEM) crosswalk indicates an approximate mapping between the ICD-10 code H43.391 its ICD-9 equivalent. The approximate mapping means there is not an exact match between the ICD-10 code and the ICD-9 code and the mapped code is not a precise representation of the original code.

Popular Posts:
- 1. icd 10 code for comminuted distal radius metaphyseal fracture
- 2. icd 10 code for elevated bun and creatinine
- 3. icd 10 code for new born care
- 4. icd-10 code for lumbar vertebroplasty
- 5. icd 10 code for c3 fracture fostic fracutre
- 6. icd 10 code for radiculopath
- 7. icd 10 code for lasik eye surgery
- 8. icd 10 code for lumbago with right sciatica
- 9. icd 10 code for right hip 3 part intertrochanteric fracture
- 10. icd 10 code for head and neck injury