Case 2
| ICD-9-CM Procedure Codes | ICD-9-CM Procedure Codes | ICD-10-PCS Codes | ICD-10-PCS Codes |
| 00.66 | PTCA | 027234Z | PTCA of 3 coronary artery sites with dru ... |
| 36.07 | Insertion of drug-eluting coronary arter ... | ||
| 00.47 | Insertion of three vascular stents | ||
| 00.41 | Procedure on two vessels |
What does CABG stand for?
Coronary artery bypass grafting (CABG) is a procedure to improve poor blood flow to the heart. It may be needed when the arteries supplying blood to heart tissue, called coronary arteries, are narrowed or blocked.
What is the CPT code for CABG?
There are no dedicated CPT codes to describe coronary bypass grafting performed robotically. Use the codes listed above. The physician may consider appending a -22 modifier (unusual procedural service) to the bypass codes if there is more work involved or reporting unlisted code 33999 for the robotic bypass surgery.
What is the ICD 10 code for status post CABG?
then what is the correct code for "Coronary artery disease status post three vessel coronary artery bypass graft" I25.10 & Z95.1 or I25.810. Please suggest ???
How to pronounce CABG?
Pronunciation of CABG with 1 audio pronunciations 1 rating rating ratings International Phonetic Alphabet (IPA) IPA : ˈkæbɪʤ
How do you code a CABG procedure?
Coronary Artery Bypass Graft (CABG) x4 The procedure was completed utilizing cardiopulmonary bypass. The ICD-10-PCS code assignment for this case example is: 02120Z9, Bypass, artery, coronary, Three sites. 021009W, Bypass, artery, coronary, One site.
What is the ICD code for CABG?
ICD-10-CM Code for Atherosclerosis of coronary artery bypass graft(s) without angina pectoris I25. 810.
What is the ICD-10 code for CAD with CABG?
I25. 810 - Atherosclerosis of coronary artery bypass graft(s) without angina pectoris | ICD-10-CM.
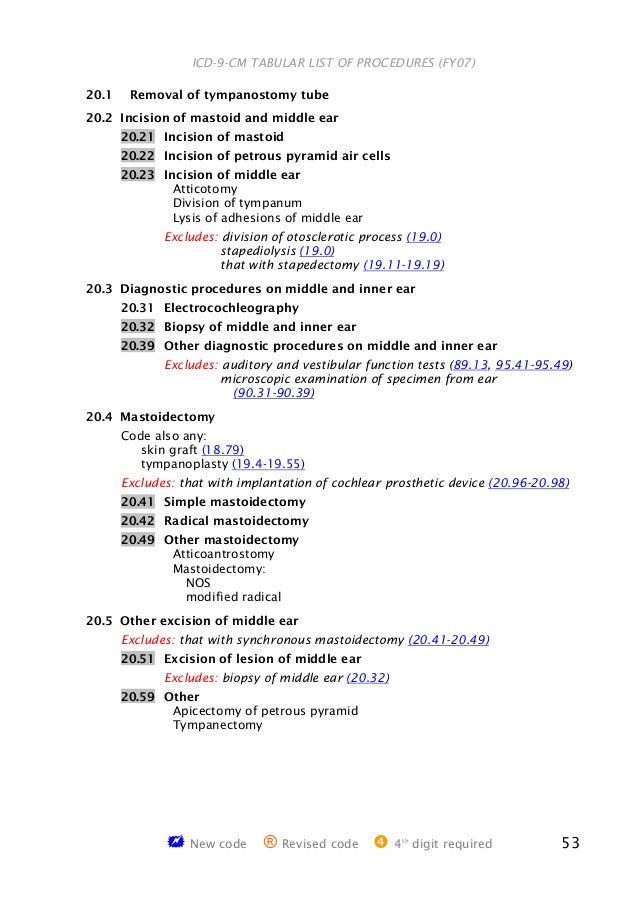
What are ICD-9 procedure codes?
ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started.
Do you code CAD after CABG?
ICD-10-CM still includes codes for patients who have undergone a CABG and have CAD. Those codes will identify whether the CAD affects a graft or a transplanted heart. The physician must document the type of graft, whether it is venous or arterial.
What is hx of CABG?
Coronary artery bypass grafting (CABG) is a type of surgery called revascularization, used to improve blood flow to the heart in people with severe coronary artery disease (CAD). CABG is one treatment for CAD.
What is the ICD 10 code for cardiovascular disease?
I25 Chronic ischaemic heart disease.
What is the ICD-10 diagnosis code for CAD?
Code I25* is the diagnosis code used for Chronic Ischemic Heart Disease, also known as Coronary artery disease (CAD). It is a is a group of diseases that includes: stable angina, unstable angina, myocardial infarction, and sudden coronary death.
What does CAD SP CABG mean?
What is coronary bypass graft surgery? Coronary artery bypass graft surgery (CABG) is a procedure used to treat coronary artery disease. Coronary artery disease (CAD) is the narrowing of the coronary arteries – the blood vessels that supply oxygen and nutrients to the heart muscle.
What is an example of an ICD-9 code?
Most ICD-9 codes are three digits to the left of a decimal point and one or two digits to the right of one. For example: 250.0 is diabetes with no complications. 530.81 is gastroesophageal reflux disease (GERD).
Where can I find procedure codes?
The American Medical Association (AMA) has several resources to help accurately bill procedures and services with the Current Procedural Terminology (CPT®) code set and Healthcare Common Procedure Coding System (HCPCS) codes. Visit the AMA Store for coding resources from the authoritative source on the CPT code set.
What is the difference between CPT and ICD-9 procedure codes?
In a concise statement, ICD-9 is the code used to describe the condition or disease being treated, also known as the diagnosis. CPT is the code used to describe the treatment and diagnostic services provided for that diagnosis.
What is CABG in a cardiologist?
The abbreviation CABG is used to indicate a coronary artery bypass graft. There are, however, two different surgical approaches, one using the aorta and the other using the internal mammary to bypass the blockage in the coronary artery. Each is coded differently, with confusion stemming from the fact that the axis for coding coronary artery bypass procedures changes within category 36, which is unusual in ICD-9-CM.
Which artery is grafted to the left internal mammary?
3. The left internal mammary was brought down to bypass occlusion in the LAD (left anterior descending); saphenous vein graft to obtuse marginal branch of the circumflex artery, saphenous vein graft to diagonal artery, and saphenous vein graft to proximal posterior descending artery.
What is the purpose of internal mammary bypass?
The internal mammary-coronary artery bypass is accomplished by loosening the internal mammary artery from its normal position and using the internal mammary artery to bring blood from the subclavian artery to the occluded coronary artery. The axis for coding internal mammary artery bypass is whether one or both internal mammary arteries are used, regardless of the number of coronary arteries that may be involved.
Which artery is used for aortocortical grafts?
All four grafts brought blood from the aorta to the coronary arteries. Sections of both saphenous vein and internal artery were used for this purpose, but the vessels used for the graft do not affect the code. The axis in assigning the code for aortocoronary bypass grafts is the number of arteries that were involved in the graft.
What is the ICD-9 code for MI?
Also, what about coding for MI or a chronic condition? If a patient is admitted to the hospital for an acute MI of the anterior wall the appropriate diagnosis code is 410.11, right? Immediately intervention is performed which resolves the acute MI. Subsequent visits for that patient during that hospital admission will still be coded with 410.11 along with all other relevant ICD-9 codes because that code demonstrates the reason for the visit. Same goes for chronic conditions like atrial fibrillation. Sometimes a patient will have atrial fibrillation for years but occasionally will spontaneously convert to normal sinus rhythm. Even when the patient is not in atrial fibrillation we would still code an office visit with 427.31 because it is an ongoing chronic condition and it will be taken into account when changing medications or ordering diagnostic tests.
What is the CPT code for a device being removed?
Actually, the CPT code 33968 tells the payer that the device is being removed. The diagnosis code is just to tell them why it is being removed, and yes 458.9 is not the most accurate code but if it allows the claim to be paid and V53.39 creates a denial then I will use 458.9.
What is the fitting and adjustment V code?
I understand everything you said except I disagree with this statement, "The fitting and adjustment V code is the one that tells the payer the device is being removed". Actually, the CPT code 33968 tells the payer that the device is being removed. The diagnosis code is just to tell them why it is being removed, and yes 458.9 is not the most accurate code but if it allows the claim to be paid and V53.39 creates a denial then I will use 458.9.
What page do you read the guidelines on?
You need to read all the guidelines page 1 included.
Can you use a DX code for a condition?
I disagree it is never acceptable to use a dx code for a condition the patient does not currently possess. The coding guidelines are mandated to followed under the HIPAA.#N#The guidelines state:#N#Aftercare visit codes cover situations when the initial treatment of a disease or injury has been performed and the patient requires continued care during the healing or recovery phase, or for the long-term consequences of the disease.#N#The aftercare codes are generally first listed to explain the specific reason for the encounter.#N#Status V codes may be used with aftercare V codes to indicate the nature of the aftercare. For example code V45.81, Aortocoronary bypass status, may be used with code V58.73, Aftercare following surgery of the circulatory system, NEC, to indicate the surgery for which the aftercare is being performed.#N#The fitting and adjustment V code is the one that tells the payer the device is being removed. You stated in your earlier post that the patient is no longer hypotensive and that is the reason the device is being removed. Yet you continue to communicate with the 458.9 that the patient stills has the hypotensive condition.#N#The payer is required to accept the V codes when properly used. They can have coverage issues that are for the encounter as a whole but not just because you use a V code properly.
Can you eliminate V codes?
Ok but it does not state you eliminate the V codes and it clearly states the provider determines the patients diagnosis. You stated the documented reason for the procedure is that the patient is no longer hypotensive . Therefore you cannot assign a code for hypotension. You must use the aftercare V codes.
Can a payer dictate a DX code?
The payer cannot dictate the dx code. You have stated exactly what I said, the patient is no longer hypotensive, the reason for the removal of the device is the absence of this status. You cannot use a dx code for a condition that does not exist. V codes are perfectly acceptable as a primary dx code , there are just certain V codes that are secondary only allowed such as the V45.81. You never use the dx code for the reason for a procedure as the dx for the aftercare. This covered in the coding guidelines.
Popular Posts:
- 1. icd 10 code for fall injury left rib
- 2. icd 10 code for nicu for jaundice due to fetal abo incompatibility
- 3. icd 10 code for viral meningoencephalitis.
- 4. icd 10 code for stoma prolapse
- 5. icd 10 code for left thumb cmc arthritis
- 6. icd 10 code for cpt code 99396
- 7. icd 10 code for lebac disease
- 8. icd 10 code for stage 4 chronic kidney disease
- 9. icd 10 code for plahdomyolysis
- 10. icd 10 code for neural foraminal narrowing lumbar