How to code a patient on dialysis?
• This situation should be coded using the ESRD-related services G codes for a home dialysis patient per full month. • Physicians and practitioners should use G0320 through G0323 when billing for outpatient ESRD-
What is the ICD 10 code for diagnosis?
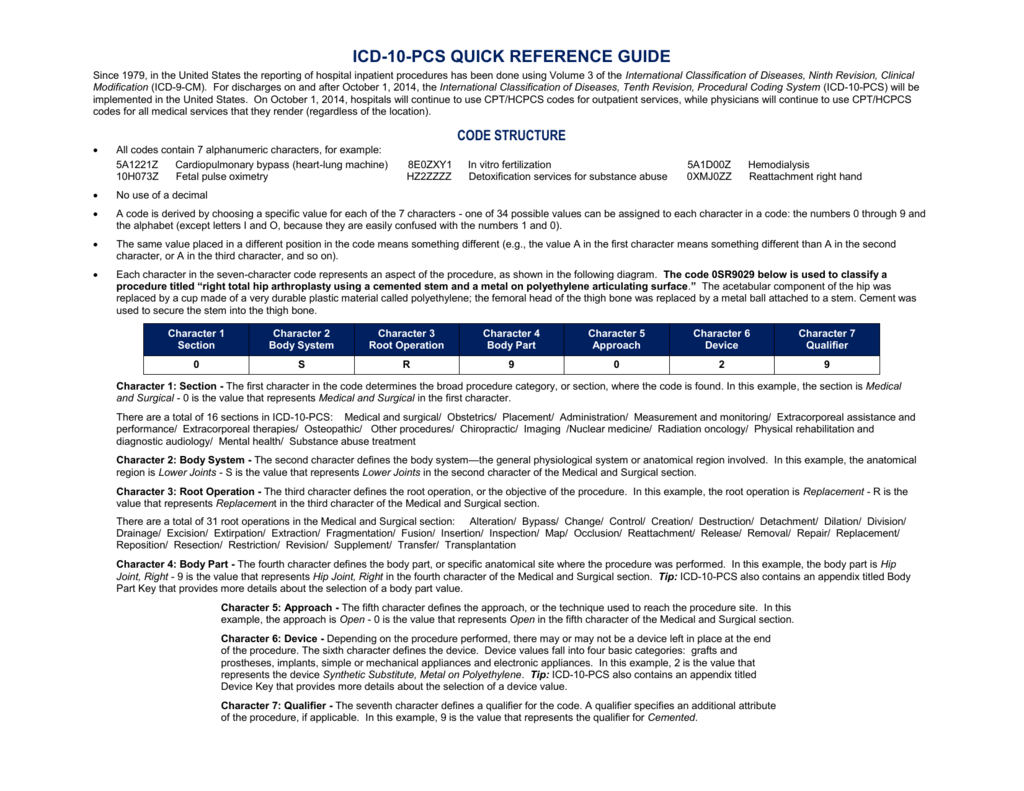
- Similar to the diagnosis code set, the alpha characters in ICD 10 code sets are not case-sensitive.
- The letters “O” and “I” are not in the code set. ...
- The 7 characters in the procedure code set help in providing very precise details. ...
- The fourth character identifies the part of the body. ...
What is the ICD 10 code for dialysis?
External cause codes for renal dialysis coding
- Publication Date:
- ICD 10 AM Edition:
- Retired Date:
- Query Number: External cause codes for renal dialysis coding. In particular we would like the VICC to clarify the use of the Y code associated with renal dialysis - Y84.1 ...
- Response. ...
What is the CPT code for home dialysis?
inpatient dialysis services. CPT Code Description 90963 End-stage renal disease (ESRD) related services for home dialysis per full month, for patients younger than 2 years of age 90964 End-stage renal disease (ESRD) related services for home dialysis per full month, for patients 2 thru 11 years of age

How do you code hemodialysis?
CPT code 90935 applies to one hemodialysis treatment that includes a single physician or other qualified health care provider's evaluation of the patient and 90937 is for a hemodialysis procedure when patient re-evaluation(s) must be done during the procedure, with or without substantial revision of the dialysis ...
What is the ICD-10 code for ESRD on hemodialysis?
ESRD is reported as 585.6 in ICD-9-CM and N18. 6 in ICD-10-CM. Additional guidance is provided in ICD-10-CM under N18. 6 to use additional codes to identify dialysis status (Z99.
What is the ICD-10 code for chronic dialysis?
Z99. 2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD-10-CM code for presence of an AV fistula for dialysis?
ICD-10 code I77. 0 for Arteriovenous fistula, acquired is a medical classification as listed by WHO under the range - Diseases of the circulatory system .
What is the difference between ICD-10 code N18 31 and N18 32?
N18. 31- Chronic Kidney Disease- stage 3a. N18. 32- Chronic Kidney Disease- stage 3b.
What is the ICD-10 code for renal disease?
ICD-10 code N18. 9 for Chronic kidney disease, unspecified is a medical classification as listed by WHO under the range - Diseases of the genitourinary system .
What is the ICD-10 code for dialysis catheter?
For a hemodialysis catheter, the appropriate code is Z49. 01 (Encounter for fitting and adjustment of extracorporeal dialysis catheter). For any other CVC, code Z45. 2 (Encounter for adjustment and management of vascular access device) should be assigned.
What is the ICD-10 code for EVAR?
Presence of other vascular implants and grafts Z95. 828 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z95. 828 became effective on October 1, 2021.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
Refer to the National Government Services Local Coverage Determination (LCD) L37475, Frequency of Hemodialysis, for reasonable and necessary requirements and frequency limitations.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that are Covered” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
Refer to the WPS GHA Local Coverage Determination (LCD) L37537, Frequency of Hemodialysis, for reasonable and necessary requirements and frequency limitations.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Are Covered” section of this policy.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
How to remove thrombus from dialysis catheter?
There are three ways to remove clots and thrombus, fibrin sheaths, and other obstructive material from dialysis catheters: (1) declotting by injection, (2) removing external obstruction, or (3) removing internal obstruction.
Can a physician bill for a catheter?
For procedures performed in the office where the physician incurs the cost of the catheter, the physician can bill the HCPCS A-code for the catheter in addition to the CPT™* code for the procedure of placing it. However, many payers include payment for the device in the payment for the CPT™* procedure code and do not pay separately for the catheter.
Can you use 76937 and 77001 with dialysis?
The code depends on the type of imaging used. If both ultrasound guidance and fluoroscopic guidance are performed, both 76937 and 77001 can be assigned together with the dialysis catheter code.
Can a dialysis catheter be used in an outpatient setting?
However, some patients who are already hospitalized may need a dialysis catheter. When insertion is performed as an inpatient the ICD-10-PCS code set is used to report the procedure provide in this care setting. The ICD-10-PCS procedure code depends on several factors, including non-tunneled (acute, short term use) or tunneled (chronic, long-term use), and the anatomic site where the internal tip of the dialysis catheter rests.
What is HD in hemodialysis?
For patients with end-stage renal disease (ESRD), hemodialysis (HD) is a convenient option for “renal replacement” therapy. HD includes two components, “ultrafiltration,” which is employed to remove extra fluid and “dialysis,” which relies on diffusion to remove small molecule waste products. In practice, these are delivered by channeling a portion of a patient’s blood flow into an extracorporeal circuit which includes an artificial kidney within which the critical therapeutic processes take place. Control and monitoring of these functions are regulated by features built into the dialysis machine. On average, patients must receive HD treatment three times a week for a duration of three or more hours.
Does Medicare cover home dialysis?
Medicare does cover home dialysis and other medically necessary items for home dialysis, when reasonable and necessary for patients with end-stage renal disease. Refer to the Medicare Benefit Policy Manual Chapter 11- End-Stage Renal Disease (ESRD) at
Popular Posts:
- 1. icd 10 code for previous left craniotomy
- 2. icd 10 code for mild sleep apnea
- 3. icd 10 code for tinea inguinal
- 4. icd 10 code for grade 3 liver laceration
- 5. icd 10 code for r12
- 6. icd 10 code for hx of bipolar disorder
- 7. icd-10 code for dilated biliary tree
- 8. icd 10 code for cervical spine osteoarthritis
- 9. due to hypoglycemia (without coma is what code for icd 10 cm
- 10. icd 10 code for abnormal treadmill