What is the ICD 10 code for diagnosis 2022?
2022 ICD-10-CM Diagnosis Code R47.1 R47.1 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R47.1 became effective on October 1, 2021. This is the American ICD-10-CM version of R47.1 - other international versions of ICD-10 R47.1 may differ.
When to assign diagnosis codes to pathology?
Anytime a doc sends something to pathology, you should not be assigning a diagnosis until that path report comes back. Per the AHA coding clinic, there is no requirement to wait until the pathology report before assigning a diagnosis code for outpatient (and also physician) coding.
Can a doctor code from a final report?
If there is a final report available at the time of coding, which is authenticated by a physician, it may be used to code from. Outpatient coders may not code from laboratory reports unless the physician has made a notation regarding the findings with a diagnosis from the laboratory results.
What is the ICD 10 code for excluded note?
R47.1 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R47.1 became effective on October 1, 2021. This is the American ICD-10-CM version of R47.1 - other international versions of ICD-10 R47.1 may differ. A type 1 excludes note is a pure excludes.
When should ICD-10 code Z09 be used?
Z09 - Encounter for follow-up examination after completed treatment for conditions other than malignant neoplasm | ICD-10-CM.
What is diagnosis code Z71 89?
Other specified counselingICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
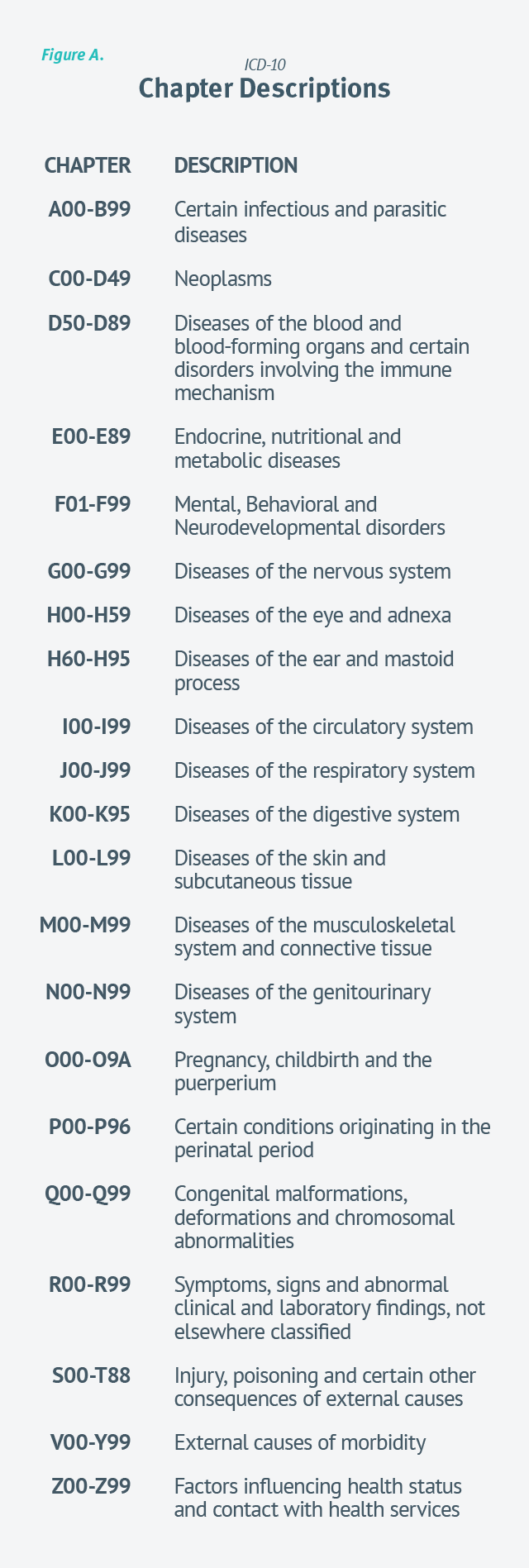
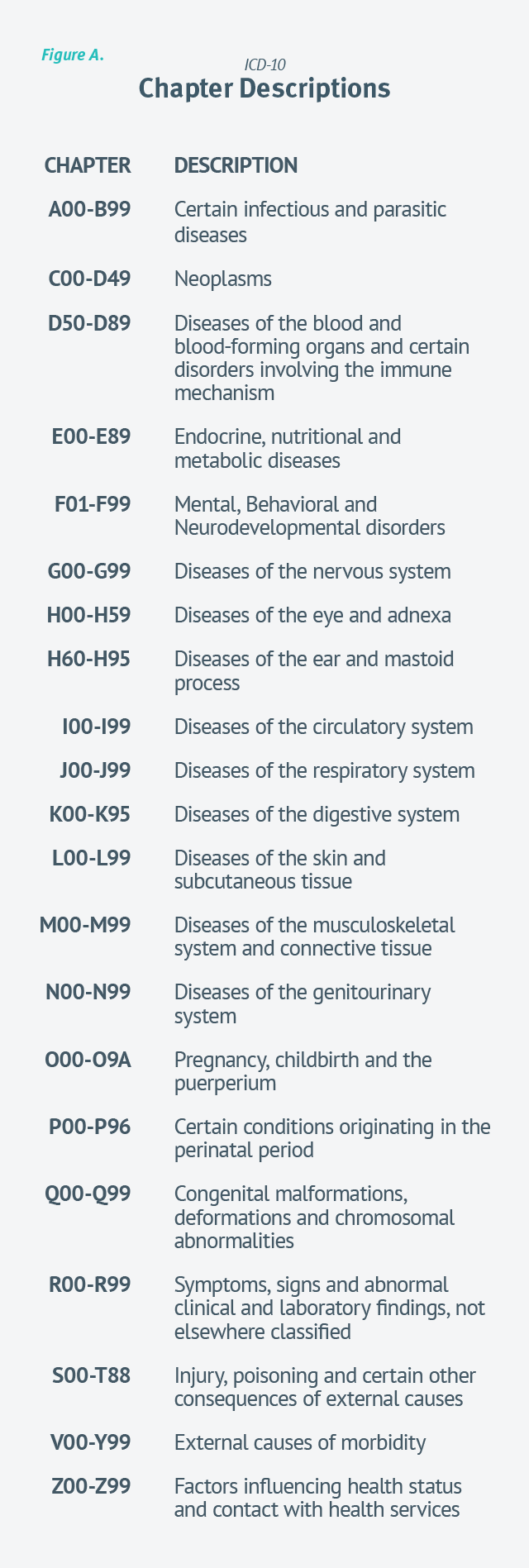
What are ICD-10-CM codes used for reporting?
Used for medical claim reporting in all healthcare settings, ICD-10-CM is a standardized classification system of diagnosis codes that represent conditions and diseases, related health problems, abnormal findings, signs and symptoms, injuries, external causes of injuries and diseases, and social circumstances.
What is the ICD-10 code for paperwork completion?
ICD-10-CM Code for Encounter for other administrative examinations Z02. 89.
Can Z23 be a primary diagnosis?
If the immunization is related to exposure (eg, the administration of a Tdap vaccine as a part of wound care), the ICD-10 code describing the exposure should be used as the primary diagnosis code for the vaccine, and Z23 should be used as the secondary code.
Is Z71 89 a billable code?
Z71. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z71. 89 became effective on October 1, 2021.
What are ICD-9 codes used for?
ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started.
Which is listed alphabetically according to Main term in ICD-10-CM?
A code listed next to a main term in the ICD-10-CM Alphabetic Index is called a default code, which: • Represents the condition most commonly associated with the main term; or • Indicates that it is the unspecified code for the condition.
What are some common ICD-10 codes?
Top 10 Outpatient Diagnoses at Hospitals by Volume, 2018RankICD-10 CodeNumber of Diagnoses1.Z12317,875,1192.I105,405,7273.Z233,219,5864.Z00003,132,4636 more rows
What is Z02 79?
2022 ICD-10-CM Diagnosis Code Z02. 79: Encounter for issue of other medical certificate.
What does Z02 mean?
Z02.2. Encounter for examination for admission to residential institution.
What is the ICD-10 code for work clearance?
1: Encounter for pre-employment examination.
Can Z76 89 be a primary diagnosis?
The patient's primary diagnostic code is the most important. Assuming the patient's primary diagnostic code is Z76. 89, look in the list below to see which MDC's "Assignment of Diagnosis Codes" is first. That is the MDC that the patient will be grouped into.
What does obesity unspecified mean?
Having a high amount of body fat (body mass index [bmi] of 30 or more). Having a high amount of body fat. A person is considered obese if they have a body mass index (bmi) of 30 or more.
What does encounter for screening for other disorder mean?
Encounter for screening for other diseases and disorders Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.
What is the CPT code for preventive care exam?
99381 Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; infant (age younger than 1 ...
Who is on the technical advisory panel for ICD-10 PCS?
A Technical Advisory Panel, which included representatives from the American Health Information Management Association, American Hospital Association and the American Medical Association, provided review and comment throughout.
What is the importance of ICD-10 PCS?
The CDACs concluded that procedures coded in ICD-10-PCS provided a much more complete and accurate description of the procedure performed. The specification of the procedures performed not only affects payment, but is integral to internal management systems, external performance comparisons, and the assessment of quality of care. The detail and completeness of ICD-10-PCS is essential in today’s healthcare environment.
What is the ICD-9-CM volume 3?
Volume 3 of the International Classification of Diseases 9th Revision Clinical Modification (ICD-9-CM) has been used in the U.S. for the reporting of inpatient pro-cedures since 1979. The structure of Volume 3 of ICD-9-CM has not allowed new procedures associated with rapidly changing technology to be effectively incorporated as new codes. As a result, in 1992 the U.S. Centers for Medicare and Medicaid Services (CMS) funded a project to design a replacement for Volume 3 of ICD-9-CM. After a review of the preliminary design, CMS in 1995 awarded 3M Health Information Systems a three-year contract to complete development of the replacement system. The new system is the ICD-10 Procedure Coding System (ICD-10-PCS).
What is a qualifier in a code?
The qualifier is specified in the seventh character. The qualifier contains unique values for individual procedures as needed. For example, the qualifier can be used to identify the destination site in a bypass.
How many diagnosis codes can be sent in MEDENT?
MEDENT Users Only: Use EXTDX or 99080 ANSI 5010 guidelines specify a maximum of 12 diagnosis codes can be sent at the claim level; however, charges can only have a total of 4 diagnosis pointers in MEDENT software.
What is the TP code for 1181F?
1181F (Initial assessment by BCBA) with G8539 (Initial assessment & TP per 15 min units); G9165 (patient status code); AND G9166 (initial ABA TP goal); OR if no deficiencies found use G8542 with 1181F
What is S5108 in ABA?
S5108 (ABA reinforcement rendered jointly by Supervisor and BCaBA/Tutor)
What is 99091?
99091 – Collection and interpretation of physiologic data (eg, ECG, blood pressure, glucose monitoring) digitally stored and/or transmitted by the patient and/or caregiver to the physician or other qualified health care professional, qualified by education, training, licensure/regulation (when applicable) requiring a minimum of 30 minutes of time
Can you send diagnostic codes beyond the maximum allowed per claim?
Diagnosis codes beyond the maximum allowed per claim will not be sent.
Is DWC-073 reimbursement for RME?
NOTE: When required by §129.5 to submit a DWC-073, an RME doctor or designated doctor is not reimbursed the $15 for filing the report. Reimbursement to RME doctors and designated doctors for the report is included in the reimbursement for the examination, as outlined in subsections (i) and (k) of §134.204 and addressed above in the Return to Work and Evaluation of Medical Care Exams section of this training module.
What is the ICd 10 code for screening?
There is a general code for screening, Z01.89, described in the ICD-10 guidelines, below. There are also more specific codes for screening that are required by Medicare and other payers for specific tests and conditions.
What are the difficulties in coding?
One of the difficulties in coding is that there are different rules for professional services and facility services.
Why is testing used to rule out a suspected diagnosis?
Testing to rule out or confirm a suspected diagnosis because the patient has a sign or symptom is a diagnostic examination, not a screening.
What is encounter Z13.220?
Z13.220, encounter for screening for lipoid disorder.
What is screening for disease?
Screening is the testing for disease or disease precursors in seemingly well individuals so that early detection and treatment can be provided for those who test positive for the disease (e.g., screening mammogram). Notice that the guidelines say a screening is a test performed on a patient who is well, for the purpose of the early detection.
When to use a sign, symptom or diagnosis?
Use a sign, symptom or diagnosis when the test is being done to monitor an existing disease or condition or to diagnosis a condition, based on a symptom. Use a screening diagnosis for tests ordered “in the absence of any signs, symptoms or associated diagnosis.”. Associated diagnosis is the condition being treated.
Can you code a definitive diagnosis?
For outpatient encounters for diagnostic tests that have been interpreted by a physician, and the final report is available at the time of coding, code any confirmed or definitive diagnosis (es) documented in the interpretation. Do not code related signs and symptoms as additional diagnoses.
What is the V code for a routine test?
For encounters for routine laboratory/radiology testing in the abscence of any signs, or associated diagnosis, assign V72.5 and a code from subcategory V72.6. If routine testing is performed during the same encounter as a test to evaluate a sign, symptom, or diagnosis, it is appropriate to assign both the V code and the code describing the reason for the non-routine test.
What is sequenced in a diagnosis?
For patients receiving diagnostics services only during an encounter/visit, sequence first the diagnosis, condition, problem or other reason for the encounter shown in the medical record to be chiefly responsible for the outpatient service provided during encounter. Codes for other diagnosises (eg chronic conditions) may be sequenced as additional diagnosises.
Can you code a definitive diagnosis?
For outpatient encounters for diagnostic tests that have been interpreted by a physician, and the final report is available at the time of coding, code any confirmed or definitive diagnosis (es) documented in the interpretation. Do not code related signs and symptoms as additional diagnosises.
When was the first symptom classification published?
In May 1974 , the National Ambulatory Med- ical Care Survey Symptom Classification was published as “the first attempt of the National Center for Health Statistics to develop a meth- odolo~y for classifying patients’ symptoms, com- plaints, problems, and reasons for seeking ambulatory medical care.”1 The Symptom Classification has been used since that time in the National Ambulatory Medical Care Survey and by others. In 1975, an evaluation of the National Ambulatory Medical Care Survey Symptom Classification and other existing classi- fications that might be used to classify reasons fur ambulatory medical care visits was under- tdwm by the American Medical Record Associa- tion under contract to the National Center for Hm.lth Statistics. As a finaJ product of the con- tract, a model system for classifying reason for visit data was developed. This report, abstracting mtiterial from the contractor’s final report and related sources, presents the Reason for Visit Classification for Ambulatory Care (RVC) along with a summary of events leading to its develop- ment. The philosophy and structure of the RVC are presented, along with comments on possible applications and on updating or revision of the
What was the purpose of the 1975 NAMCS symptom classification?
In July 1975, the American Medical Record Association (AMRA) was awarded a contract to evaluate, the NAMCS Symptom Classification and other existing medical taxonomies that might be used to classify patients’ reasons for seeking ambulatory medical care, and to develop and test a model system for classifying this type of information. One of the many requirements of this model system was that it meet not only the needs of the NAMCS, but also the needs of a wide variety of other users. An initial research phase included an exten- sive review of the literature pertaining to medi- cal and health care classifications and the com- pilation of an annotated bibliography relating to the design, development, description, use, evaluation, and analysis of medical classification systems. Consultations with over 100 individ- uals involved in fields relating to the classifica- tion ofhealth care data provided the necessary input to determine the needs and purposes for a classification of reason for visit data. This preliminary research paved the way for the Conference on Symptom Classifications for Ambulatory Care held in November 1975. This ‘conference provided a forum for national ex- perts in the field of ambulatory medical care classifications and users of the NAMCS Symp- tom Classification for input into the project. The specific goals of the conference included establishing criteria forevaluation of reason visit classifications and concepts leading to the development of a methodology for the design of health care classification systems. Information was gathered from a variety of users of the NAMCS Symptom Classification, and problems associated with the Symptom Classification were identified. A methodology for the evaluation and de- sign of medical classification systems was sub- sequently developed. The principles set forth in this methodology provided the conceptual framework from which the model reason for visit classification was deveIoped and tested. A complete description of the background for the evaluation and design methodology has been presented by Schneider and Parziale.T Six existing classification systems were selected, tested, and evaluated for their applica- bility in coding reason for visit data; (1) NAMCS Symptom Classification,l (2) Patient Request Code,s (3) CR Alpha Code,g (4) Columbia Medical Plan Classification,l O (5) International Classification of Health Problems in Primary Care,l 1 and (6) International Classification of Diseases (ICD-9).1 z The last two classifications areprimarily diagnostic codes and not spe- cifically designed to classify reason for visit data, particularly in lay terminology. They were in- cluded in the evaluation because of their wide- spread use, and because they may be considered by many users for coding reason for visit data. Reason for visit data from the 1974 NAMCS and from the State of Wisconsin emergency room study]s were used to test each of the above system’s applicability to code these data. Each system was evaluated according to the fol- lowing criteria: ease of understanding, clarity, accuracy, specificity, efficiency, conciseness, comprehensiveness, flexibility revision, and computer applicability. These evaluations helped to pinpoint the strengths and weaknesses of the existing systems, and the findings from these evaluations were used as a basis for the develop- ment of the RVC. The RVC underwent several revisions before reaching the version presented in this report. The modular structure, which is discussed later in the report, was introduced in the first version.
What is the test results module?
Test Results Module. –Reasons coded into this module represent return visits to receive test results. The patient may have been toId that results from previously administered tests were abnormal or may be returning to receive test results. The dia~osis may or may not yet be established. The physician’s response is usually tocarry out further diagnostic tests or initiate a therapeutic regimen.
What is the injury and adverse effect module?
Injuries and Adverse Efji?cts Module. –This module includes reasons for visit that are clearly the result of an injury or adverse effect. These visitsare often emergency that require im- mediate care, and the physician’s response is to aIleviate the patient’s immediate problem.
What is a treatment module?
Treatment Module. –These visits are, gener- ally, for the purpose of providing specific thera- peutic care, treatment, or counseling; the physi- cian’s response is to carry out the request and usually includes the provision of a therapeutic procedure.
What is the disease module?
Disease Module. –Reasons coded into this section represent visits at which the patient gives a diagnosis as the reason for visit. This could be either a diagnosis previously supplied by the physician or a condition that the patient has ex- perienced before and/or has self-diagnosed. Most folIowup visits for chronic diseases will be coded into this module. Physician’s response is prob- ably a checkup or observation of the condition. The Disease Module, also arranged by body sys- tem, is based on a condensation of theInterna- tional Classification of Health Problems In Pri- mary Care. *1 Diagnostic, Screening, and Preventive hlod- ule. —The reasons for visit coded into this mod- ule usually represent nonillness visits, for example, visits routine physicals and preven- tive care, visits by patients in high-risk groups, or visits for family planning services or pregnancy- related examinations. The physician’s response is to directly carry out the patient’s request and generally involves the provision of some type of test or diagnostic procedure.
What is ICDA 15?
International Classification Oj -Diseases, Adapted(ICDA)15 or theInternational Classification of Health Problems in Pri- mary Care(ICHPPC),l 1 may be inserted into the Disease Module.
Popular Posts:
- 1. icd-10 code for homosexual behavior
- 2. icd-10 code for umbilical cord complication in pregnancy
- 3. icd 10 code for diarrhea due to adverse effect
- 4. icd 9 code for cowden syndrome
- 5. icd 10 code for left pca territory infarct
- 6. icd 10 code for acute l2 compression fracture
- 7. icd 10 code for ankle abrasion
- 8. icd 9 code for diverticulosis nos
- 9. icd 10 code for hemorrhagic transformation
- 10. icd 10 code for inguinal bulging