What is the CPT code for a Pulse Ox?
The Current Procedural Terminology (CPT) identifies three codes and descriptors that may be reported for pulse oximetry 94760, 94761, and 94762. The code descriptions and the approximate Medicare reimbursement are as follows:
What does CPT code 94760 mean?
What does CPT code 94760 mean? 94760 , noninvasive ear or pulse oximetry for oxygen saturation; single determination: simple pulse oximetry study with one Sao2 (Spo2) value documented. Does Medicare pay for CPT 99050?
What is 94760 CPT code?
The Current Procedural Terminology (CPT ®) code 94760 as maintained by American Medical Association, is a medical procedural code under the range - Pulmonary Diagnostic Testing and Therapies. Subscribe to Codify and get the code details in a flash.
What is CPT 94760?
CPT codes covered if selection criteria is met: 94760 : Noninvasive ear or pulse oximetry for oxygen saturation; single determination: 94761 : multiple determinations (e.g., during exercise) 94762 : by continuous overnight monitoring (separate procedure) Other CPT codes related to the CPB: 42820: Tonsillectomy and adenoidectomy; younger than age 12: 42821
What is the CPT code for a pulse oximetry?
Group 2CodeDescription94762NONINVASIVE EAR OR PULSE OXIMETRY FOR OXYGEN SATURATION; BY CONTINUOUS OVERNIGHT MONITORING (SEPARATE PROCEDURE)
What is ICD 10 code for oxygen desaturation?
R09. 02 - Hypoxemia. ICD-10-CM.
What is diagnosis code R09 02?
HypoxemiaICD-10 code R09. 02 for Hypoxemia is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD 10 code for oxygen?
Z99. 81 - Dependence on supplemental oxygen. ICD-10-CM.
What is R53 83?
ICD-9 Code Transition: 780.79 Code R53. 83 is the diagnosis code used for Other Fatigue. It is a condition marked by drowsiness and an unusual lack of energy and mental alertness. It can be caused by many things, including illness, injury, or drugs.
What is the diagnosis for ICD-10 code r50 9?
9: Fever, unspecified.
What is the ICD-10 code for acute hypoxia?
ICD-10 code J96. 01 for Acute respiratory failure with hypoxia is a medical classification as listed by WHO under the range - Diseases of the respiratory system .
What is hypoxemia medical term?
Definition. By Mayo Clinic Staff. Hypoxemia is a below-normal level of oxygen in your blood, specifically in the arteries. Hypoxemia is a sign of a problem related to breathing or circulation, and may result in various symptoms, such as shortness of breath.
Is hypoxia and hypoxemia the same thing?
Hypoxemia (low oxygen in your blood) can cause hypoxia (low oxygen in your tissues) when your blood doesn't carry enough oxygen to your tissues to meet your body's needs. The word hypoxia is sometimes used to describe both problems.
What is the ICD-10 code for shortness of breath?
ICD-10 code R06. 02 for Shortness of breath is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD-10 code for respiratory failure?
ICD-10 code J96. 90 for Respiratory failure, unspecified, unspecified whether with hypoxia or hypercapnia is a medical classification as listed by WHO under the range - Diseases of the respiratory system .
How many ICD-10 codes are there?
Another difference is the number of codes: ICD-10-CM has 68,000 codes, while ICD-10-PCS has 87,000 codes.
What is desaturation?
/ (diːˌsætʃəˈreɪʃən) / noun. physics the addition of white light to a pure colour to produce a paler less saturated colour.
Is hypoxia and hypoxemia the same thing?
Hypoxemia (low oxygen in your blood) can cause hypoxia (low oxygen in your tissues) when your blood doesn't carry enough oxygen to your tissues to meet your body's needs. The word hypoxia is sometimes used to describe both problems.
What does low o2 saturation indicate?
Low blood oxygen levels indicate that your lungs and/or circulatory system may not be working as they should.
What hypoxemia means?
Definition. By Mayo Clinic Staff. Hypoxemia is a below-normal level of oxygen in your blood, specifically in the arteries. Hypoxemia is a sign of a problem related to breathing or circulation, and may result in various symptoms, such as shortness of breath.
Why do you need pulse oximetry?
For patients on long-term oxygen therapy, pulse oximetry arterial oxygen saturation (SaO2) measurements are unnecessary except to assess changes in clinical status, or to facilitate changes in the oxygen prescription. Home pulse oximetry is also indicated when there is a need to monitor the adequacy of SaO2 or the need to quantitate the response of SaO2 to a therapeutic intervention.
What is the purpose of an oximeter?
They are often also referred to as "pulse oximeters" because they also measure and record an individual’s heart rate. A sensor is placed on a finger, toe or ear and uses light to estimate the oxygen saturation in the arterial blood; the sensor is connected by a wire to a monitor, which then displays both the oxygen saturation (O2 sat) and the heart rate.
Why is home oximetry important?
Home oximetry may be used to monitor the O2 sat in the blood of individuals with known or suspected heart disease or many other circulatory or lung disorders. It may be considered medically necessary to assist the physician in determining the correct flow of supplemental oxygen, monitor changes in O2 sat during exercise and assist with management of home ventilators. The units used in the home are usually small, portable hand-held devices, though they can be larger, stationary machines.
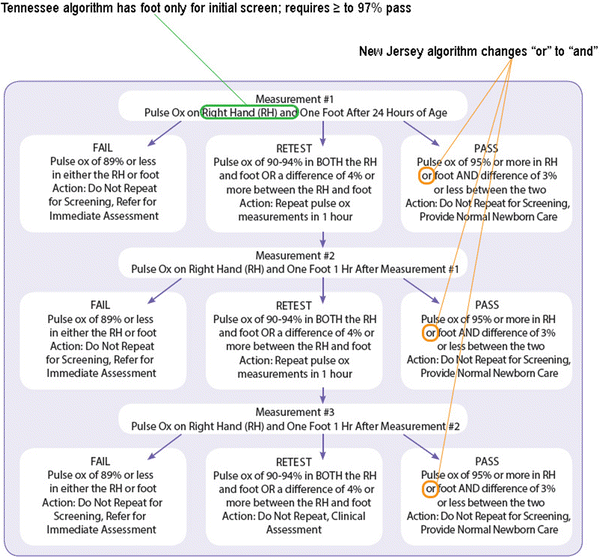
Can pulse oximetry be used for infants?
Pulse oximetry can be used in conjunction with infant home apnea monitoring; for information on infant apnea monitors, see CPB 0003 - Apnea Monitors for Infants. Home pulse oximetry for indications other than those listed above may be considered medically necessary upon medical review.
How to reduce inter-stage morbidity and mortality for patients with single ventricle following stage 1 palli?
Use of telemedicine devices for home monitoring has been shown to improve outcomes in adults. These devices allow for a more automated approach to home monitoring that have many advantages. These researchers described their program that utilizes a web-based telemedicine device to capture and transmit data from the homes of their patients during the inter-stage period. The authors stated that their early data suggested that home telemedicine is feasible, provides a more systematic data review and analysis and supports the assertion that patients using home surveillance have significantly better nutritional status than those not using home monitoring.
Can pulse oximetry rule out OSA?
The sensitivity and negative predictive value of pulse oximetry is not adequate to rule out OSA in patients with mild to moderate symptoms. Therefore, a follow-up sleep study would be required to confirm or exclude the diagnosis of OSA, regardless of the results of pulse oximetry screening.
Is pulse oximeter considered durable medical equipment?
Policy. Aetna considers a pulse oximeter for home use medically necessary durable medical equipment (DME) for members with chronic lung disease, severe cardiopulmonary disease or neuromuscular disease involving muscles of respiration, and any of the following indications: To determine appropriate home oxygen liter flow for ambulation, exercise, ...
Can you bill pulse ox?
To find out more about why you cannot routinely bill the pulse ox CPT code in the emergency department , visit the pulse ox FAQ at www.acep.org/reimbursement.
Is ACEP coding and nomenclature committee partnering with ACEP?
The ACEP Coding and Nomenclature Committee has partnered with ACEP Now to provide you with practical, impactful tips to help you navigate through this coding and reimbursement maze.
How often should oximetry be performed?
In outpatient or home management for patients with chronic cardiopulmonary problems, oximetric determinations once or twice a year are considered reasonable. In all instances, there must be a documented request by a physician/non-physician provider in the medical record for these services. Regular or routine testing will not be allowed for reimbursement. In all circumstances, testing would be expected to be useful in the continued management of a patient, particularly in acute exacerbations or unstable conditions (e.g., acute bronchitis in a patient with Chronic Obstructive Pulmonary Disease (COPD)) where increased frequency of testing would be considered, on an individual consideration basis, for coverage purposes.
Why is oximetry needed?
Patient has chronic lung disease, severe cardiopulmonary disease or neuromuscular disease involving the muscles of respiration, and oximetry is needed for at least one of the following reasons: Initial evaluation to determine the severity of respiratory impairment. Evaluation of an acute change in condition.
What is arterial pulsation?
Arterial pulsation is used to gate the signal to the arterial component of blood contained within the nailbed. Ear oximetry is a noninvasive method for evaluating arterial oxygenation. Ear oximeters are commonly used in sleep studies. Single and Multiple Determinations (94760, 94761):
Is 94762 a primary procedure?
Likewise, these codes are considered included as an element of other primary procedures such as a simple pulmonar y stress test (94620) and respiratory therapy services (G0237, G0238, and G0239).5 Conversely, 94762 achieves “A” status, allowing for separate reimbursement when coverage regulations are met. Under certain circumstances, 94762 may be separately payable to a physician (see “Indications, Medical Necessity, and Documentation”).
Do CPT codes have long descriptors?
Providers are reminded to refer to the long descriptors of the CPT codes in their CPT book. The American Medical Association (AMA) and the Centers for Medicare & Medicaid Services (CMS) require the use of short CPT descriptors in policies published on the Web.
Does Medicare cover oximetry?
Medicare will allow payment for oximetry when accompanied by an appropriate ICD-9-CM code for a pulmonary disease (s) which is commonly associated with oxygen desaturation. Routine use of oximetry is non-covered. Medically necessary reasons for pulse oximetry include:
What documentation is needed for ear oximetry?
Medical record documentation maintained by the ordering/referring physician (e.g., office/progress notes) must indicate the medical necessity for performing ear or pulse oximetry studies. Additionally, a copy of the study results should be maintained in the medical records.
What is the procedure code for 94761?
Procedure codes 94760 and 94761 represent services that have a T-status indicator. Therefore, if any other services payable under the physician fee schedule are billed on the same date by the same provider, this service is bundled into the physician services for which payment is made.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Who must maintain hard copy documentation of test results and interpretation along with copies of the ordering/referring physician's order for?
If the provider of oximetry studies is other than the ordering/referring physician, that provider must maintain hard copy documentation of test results and interpretation along with copies of the ordering/referring physician's order for the study. The ordering/referring physician must state the clinical indication/medical necessity for the oximetry study in the order for the test.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
What is the Medicare 94760?
94760 is a Medicare status T code, which says : There are RVUs and payment amounts for these services, but they are only paid if there are no other services payable under the physician fee schedule billed on the same date by the same provider. If any other services payable under the physician fee schedule are billed on the same date by ...
Do pulse oximeters charge for blood pressure?
Pulse oximeter charges used to be paid, back when the equipment was expensive. Advise your doctor that now a pulse ox is similar to taking a blood pressure reading, and you don't charge separate for that tool. The pulse ox is part of the diagnostics that aids in medical decision making, complexity, and the lower the pulse ox reading, then the more complicated the medical decision making. So it is fair to be part of the E & M CPT, just make sure the documentation supports the level of coding.
Popular Posts:
- 1. icd 10 cm code for acute prostatitis.
- 2. icd code 10 for bilateral hypomastia
- 3. icd 10 code for dermatofibroma
- 4. icd 9 code for tendonitis in both feet
- 5. icd 1 code for carpal tunnel syndrome left wrist
- 6. 2019 icd 10 code for metallic anchor suture appearance in the left posterior calcaneus
- 7. icd-10 code for pain in limb
- 8. the icd-10-cm code for an outpatient encounter for routine laboratory/radi
- 9. icd 10 code for encounter for smoking cessation counseling
- 10. icd 10 code for chiari malformation type 2