ICD-9-CM procedure codes are two numeric digits followed by a decimal, which is then followed by another one or two digits. The codes begin with 00.01, to describe a therapeutic ultrasound of vessels in the head and neck, and they end with 99.99, which describes other miscellaneous procedures.
Full Answer
What is the ICD 9 cm Procedure Code?
ICD-9-CM Procedure Codes. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) mandates that Volume 3 of the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) be used to code inpatient services on medical claims.
What is the difference between a diagnosis code and Procedure Code?
All procedure codes are attached to specific charges that a hospital has determined represents its reasonable cost to perform the service. Hospitals are paid according to Diagnosis Related Groups (DRGs) for inpatient services, but diagnosis codes are not, themselves, associated with charges.
What are the instructions for the selection of principal procedure?
The following instructions should be applied in the selection of principal procedure and clarification on the importance of the relation to the principal diagnosis when more than one procedure is performed: Procedure performed for definitive treatment of both principal diagnosis and secondary diagnosis
How are ICD-9-CM Volume 3 codes used for inpatient care?
By using ICD-9-CM Volume 3 codes, hospitals establish the amount owed for a specific inpatient encounter, while the DRG assigned to the patient’s inpatient stay determines the payment.
What are the conventions of ICd 9?
What is the ICd 9 code for symptoms?
What is the code for MRSA?
What are conventions and guidelines?
What is code assignment?
When coding the birth of an infant, assign a code from categories V30-V39, according to the?
When to use subcategory 733.1?
See more
About this website
What is a principal procedure code?
The principal procedure is one that is performed for definitive treatment rather than one performed for diagnostic or exploratory purposes, or was necessary to take care of a complication.
What are ICD-9 procedure codes?
ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started.
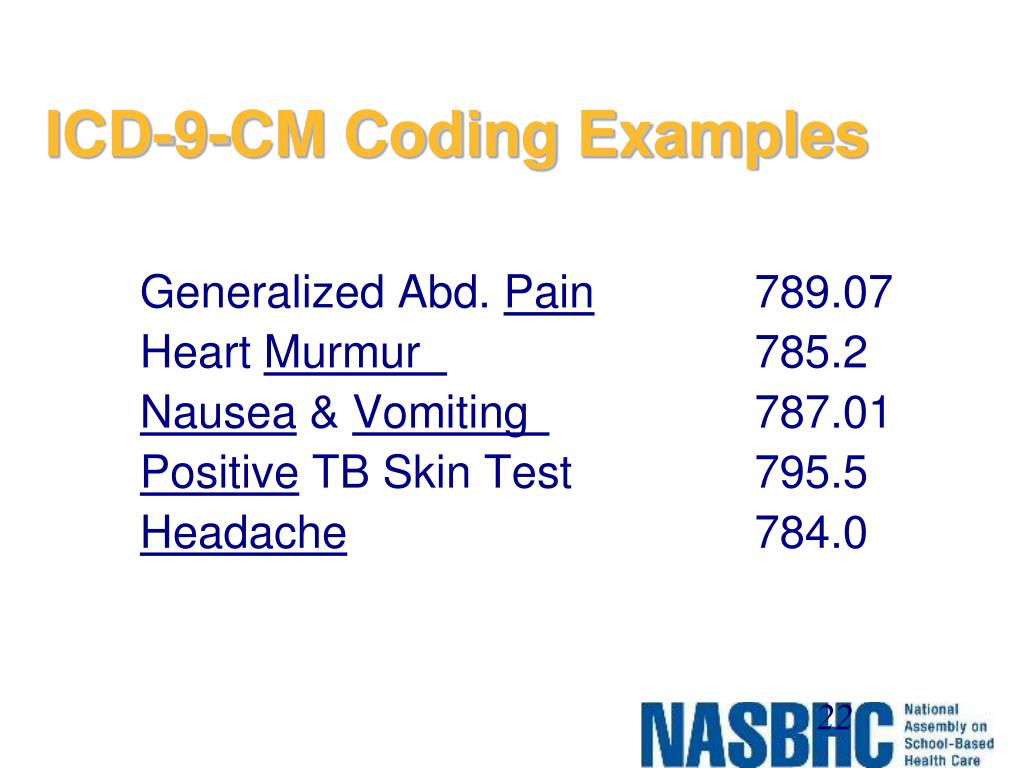
What is an example of an ICD-9 code?
Most ICD-9 codes are three digits to the left of a decimal point and one or two digits to the right of one. For example: 250.0 is diabetes with no complications. 530.81 is gastroesophageal reflux disease (GERD).
Are there ICD-10 procedure codes?
ICD-10-PCS will be the official system of assigning codes to procedures associated with hospital utilization in the United States. ICD-10-PCS codes will support data collection, payment and electronic health records. ICD-10-PCS is a medical classification coding system for procedural codes.
What is ICD-9 and ICD-10 codes?
Code Structure: Comparing ICD-9 to ICD-10ICD-9-CMICD-10-CMFirst character is numeric or alpha ( E or V)First character is alphaSecond, Third, Fourth and Fifth digits are numericAll letters used except UAlways at least three digitsCharacter 2 always numeric; 3 through 7 can be alpha or numeric3 more rows•Aug 24, 2015
How many ICD-9 codes are there?
13,000 codesThe current ICD-9-CM system consists of ∼13,000 codes and is running out of numbers.
What does ICD code mean?
International Classification of DiseasesInternational Classification of Diseases, (ICD-10-CM/PCS) Transition - Background. Related Pages.
What is procedure code in medical billing?
“Procedure” code is a catch-all term for codes used to identify what was done to or given to a patient (surgeries, durable medical equipment, medications, etc.).
Which volumes of ICD-9-CM is used for diagnostic coding?
ICD-9-CM Volume 3 is a system of procedural codes used by health insurers to classify medical procedures for billing purposes. It is a subset of the International Statistical Classification of Diseases and Related Health Problems (ICD) 9-CM. Volumes 1 and 2 are used for diagnostic codes.
What is an ICD-10-CM code?
A: ICD-10-CM (International Classification of Diseases -10th Version-Clinical Modification) is designed for classifying and reporting diseases in all healthcare settings.
What is ICD-10 cms?
International Classification of Diseases, 10th Edition, Clinical Modification/Procedure Coding System (ICD-10-CM/PCS) is October 1, 2013 for all covered entities. ICD-10-CM/PCS will enhance accurate payment for services rendered and facilitate evaluation of medical processes and outcomes.
What ICD-10-CM?
The ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) is a system used by physicians and other healthcare providers to classify and code all diagnoses, symptoms and procedures recorded in conjunction with hospital care in the United States.
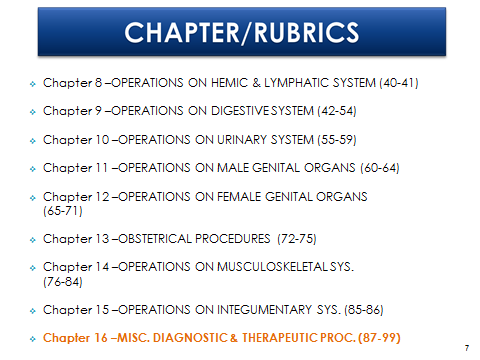
ICD-9-CM Chapters List
The 2016 edition of the ICD-9-CM is divided into 19 chapters, based on the subject of the ICD codes each chapter contains. Each chapter is identified by a chapter number and description.
ICD-9-CM Diagnosis and Procedure Codes: Abbreviated and Full Code ...
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
ICD-9 Codes Lookup - ICD-9 Codes List - Codify by AAPC
ICD-9 Codes Lookup. INTERNATIONAL CLASSIFICATION OF DISEASES, 9TH REVISION, CLINICAL MODIFICATION ICD-9-CM VOLUMES 1 & 2 (DIAGNOSES) is the code set used by Non-HIPAA covered entities (Workers’ Compensation and auto insurance companies) “that were not required to be converted to ICD-10.
(PDF) ICD-10-CM 2019: The Complete Official Codebook - Academia.edu
ICD-10-CM 2019: The Complete Official Codebook
2021 ICD-10-CM Guidelines
ICD-10-CM Official Guidelines for Coding and Reporting FY 2021 (October 1, 2020 - September 30, 2021) Narrative changes appear in bold text . Items underlined have been moved within the guidelines since the FY 2020 version
ICD-9-CM Diagnosis Codes - International Classification of Diseases ...
ICD-9-CM Medical Diagnosis Codes. The International Statistical Classification of Diseases and Related Health Problems (commonly known as the ICD) provides alpha-numeric codes to classify diseases and a wide variety of signs, symptoms, abnormal findings, complaints, social circumstances and external causes of injury or disease.
What is the ICD-9-CM code manual?
While most professional medical coders and medical billers use the diagnosis codes in ICD-9-CM every day, the code manual also contains a series of codes used to describe medical procedures. All editions of ICD-9-CM contain Volume 1 and Volume 2. Expert editions of ICD-9-CM, designed for use by hospitals and payers, also contain Volume 3, which is dedicated to procedural coding.
What is procedure code?
All procedure codes are attached to specific charges that a hospital has determined represents its reasonable cost to perform the service. Hospitals are paid according to Diagnosis Related Groups (DRGs) for inpatient services, but diagnosis codes are not, themselves, associated with charges. By using ICD-9-CM Volume 3 codes, hospitals establish the amount owed for a specific inpatient encounter, while the DRG assigned to the patient’s inpatient stay determines the payment.
What is the ICd 9 code for inpatient services?
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) mandates that Volume 3 of the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) be used to code inpatient services on medical claims. While most professional medical coders and medical billers use the diagnosis codes in ICD-9-CM every day, ...
Why are medical coders important?
Being able to bear all the code variations in mind while reviewing medical records and assembling claims, professional medical coders and medical billers reduce fraud and abuse of the healthcare reimbursement system , limiting a hospital’s legal exposure to charges of the same.
What is volume 3 code?
CMS states that hospitals can use Volume 3 codes for internal tracking purposes, but the HIPAA standard is to use Healthcare Common Procedure Coding System (HCPCS) codes in every other setting when financial transactions take place with third-party payers.
What is an inpatient hospital?
Inpatients are patients who are admitted to the hospital and stay at least overnight. Patients can be admitted to a hospital overnight solely for observation. Any services these patients receive are described by the use of HCPCS codes because they do are not in an inpatient treatment status.
When will ICD-10 replace ICd 9?
PPACA mandates that ICD-9-CM be replaced by ICD-10 in 2013. Medical coders and billers who have a solid understanding of ICD-9-CM are expected to make a smooth transition to the new coding system. ICD-10-CM, which will replace Volume 1 and Volume 2 of ICD-9-CM, and ICD-10-PCS, which will replace Volume 3 of ICD-9-CM.
Why is it important to know the definition of the principal diagnosis?
The definition of the principal diagnosis is the condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care. When a medical coder correctly assigns the principal diagnosis this will help in determining the correct principal procedure.
What is a diagnostic procedure?
A diagnostic procedure was performed for the principal diagnosis and a procedure is performed for definitive treatment of a secondary diagnosis.Sequence diagnostic procedure as principal procedure, since the procedure most related to the principal diagnosis takes precedence.
What is a sequence procedure?
Procedure performed for definitive treatment of both principal diagnosis and secondary diagnosis.Se quence procedure performed for definitive treatment most related to principal diagnosis as principal procedure.
Can an incorrect principal diagnosis lead to a lower reimbursement?
As mentioned early this can affect the reimbursement that is provided. Because of this it is essential that a medical coder assign the correct principal diagnosis and principal procedure. Incorrect assignment of these can lead to higher or lower reimbursement for the services provided to the patient .
Is a procedure related to a principal diagnosis?
No procedures performed that are related to principal diagnosis; procedures performed for definitive treatment and diagnostic procedures were performed for secondary diagnosis.Sequence procedure performed for definitive treatment of secondary diagnosis as principal procedure, since there are no procedures (definitive or non-definitive treatment) related to principal diagnosis.
Can you take shortcuts when coding inpatient records?
In order to correctly assign the principal diagnosis and principal procedure the medical coder needs to review the entire inpatient record. You cannot take shortcut when you are coding inpatient records. There are examples about the assignment of the principal procedure in the fourth quarter AHA Coding Clinic for ICD-9-CM. We encourage you to review the examples in this coding clinic to get a better understanding of the correct assignment of the principal procedure.
What are the conventions of ICd 9?
The conventions for the ICD-9-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the index and tabular of the ICD -9-CM as instructional notes. The conventions are as follows:
What is the ICd 9 code for symptoms?
Chapter 16 of ICD-9-CM, Symptoms, Signs, and Ill-defined conditions (codes 780.0 - 799.9) contain many, but not all codes for symptoms.
What is the code for MRSA?
If a patient is documented as having both MRSA colonization and infection during a hospital admission, code V02.54, Carrier or suspected carrier, Methicillin resistant Staphylococcus aureus, and a code for the MRSA infection may both be assigned.
What are conventions and guidelines?
The conventions, general guidelines and chapter-specific guidelines are applicable to all health care settings unless otherwise indicated. The conventions and instructions of the classification take precedence over guidelines.
What is code assignment?
Code assignment is based on the provider’s documentation of the relationship between the condition and the care or procedure. The guideline extends to any complications of care, regardless of the chapter the code is located in. It is important to note that not all conditions that occur during or following medical care or surgery are classified as complications. There must be a cause-and-effect relationship between the care provided and the condition, and an indication in the documentation that it is a complication. Query the provider for clarification, if the complication is not clearly documented.
When coding the birth of an infant, assign a code from categories V30-V39, according to the?
When coding the birth of an infant, assign a code from categories V30-V39, according to the type of birth. A code from this series is assigned as a principal diagnosis, and assigned only once to a newborn at the time of birth.
When to use subcategory 733.1?
Subcategory 733.1 may be used while the patient is receiving active treatment for the fracture. Examples of active treatment are: surgical treatment, emergency department encounter, evaluation and treatment by
What is the procedure code for IP claims?
IP claims are expected to have procedure codes reported in T-MSIS as coded and identified by the medical service provider when procedures are performed during an inpatient stay. The principal procedure should be reported in T-MSIS using the PROCEDURE-CODE-1 field with secondary and other procedures reported in fields PROCEDURE-CODE-2 through 6. The fields PROCEDURE-CODE-FLAG-1 through PROCEDURE-CODE-FLAG-6 are used to indicate the type of procedure code reported by the provider and should be coded either “02” (ICD-9 CM) or “07” (ICD-10 CM PCS) [1].
Why is it important to include diagnostic codes in a fee for service?
This information is important for CMS to identify, measure and evaluate Medicaid participants’ health and associated health care services delivery. Diagnosis codes are used in conjunction with procedure information from claims to support the medical necessity determination for the service rendered and, sometimes, to determine appropriate reimbursement. This information is critical and is associated with the T-MSIS priority item (TPI) Completeness of Key Claims Service Data Elements – TPI-20.
What should be left blank in a diagnosis code?
Any unused diagnosis code or flag field should be left blank. If the diagnosis code is blank, the corresponding diagnosis code flag should also be blank. If the diagnosis code is not blank, the corresponding diagnosis code flag should be populated with a valid value.
Do OT claims have diagnostic codes?
Several types of services on OT claims, such as transportation services, DME, and lab work, are not expected to have diagnosis codes. However, OT claim records for medical services, such as outpatient hospital services, physicians’ services, or clinic services are generally expected to have at least one diagnosis code.
Do all claims need to be populated with diagnosis codes?
However, not all claims and encounters require, or should be populated with diagnosis and procedure codes. This can lead to confusion in how states should submit data to T-MSIS. This guidance is intended to address that confusion.
What is principal procedure?
What is the principal procedure? The procedure that is performed for definitive treatment or is taking care of a complication is the principal procedure. Procedures for diagnostic or exploratory purposes that are performed in addition to a procedure being performed for definitive treatment, would be reported in addition to the principal procedure.
What is a diagnostic procedure?
A diagnostic procedure was performed for the principal diagnosis and a procedure is performed for definitive treatment of a secondary diagnosis. a. Sequence diagnostic procedure as principal procedure, since the procedure most related to the principal diagnosis takes precedence. No procedures performed that are related to principal diagnosis;
What are some examples of definitive and diagnostic procedures?
An example of definitive and diagnostic procedures being performed on the same admission would be: Patient is admitted with chest pain and this is worked up with cardiac catheterization/angiography. The patient is found to have significant coronary artery disease and is the scheduled for bypass surgery on the same date. In this case, the coronary artery bypass is the principal procedure as it is being performed for definitive treatment of the heart disease. The heart catheterization and angiography would be reported as additional procedures since they were diagnostic tests. Sometimes, there are only diagnostic/exploratory procedures performed. If this is the case then one of these would be reported first.
Is coding advice valid?
The information contained in this coding advice is valid at the time of posting. Viewers are encouraged to research subsequent official guidance in the areas associated with the topic as they can change rapidly.
Is MS-DRG the same regardless of sequencing?
In the example above the MS-DRG would be the same regardless of the sequencing, HOWEVER for consistency and accuracy in reporting data the coding guidelines should be followed.
Is a sequence procedure performed for definitive treatment of secondary diagnosis?
No procedures performed that are related to principal diagnosis; procedures performed for definitive treatment and diagnostic procedures were performed for secondary diagnosis. a. Sequence procedure performed for definitive treatment of secondary diagnosis as principal procedure, since there are no procedures (definitive or nondefinitive treatment) ...
What are the conventions of ICd 9?
The conventions for the ICD-9-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the index and tabular of the ICD -9-CM as instructional notes. The conventions are as follows:
What is the ICd 9 code for symptoms?
Chapter 16 of ICD-9-CM, Symptoms, Signs, and Ill-defined conditions (codes 780.0 - 799.9) contain many, but not all codes for symptoms.
What is the code for MRSA?
If a patient is documented as having both MRSA colonization and infection during a hospital admission, code V02.54, Carrier or suspected carrier, Methicillin resistant Staphylococcus aureus, and a code for the MRSA infection may both be assigned.
What are conventions and guidelines?
The conventions, general guidelines and chapter-specific guidelines are applicable to all health care settings unless otherwise indicated. The conventions and instructions of the classification take precedence over guidelines.
What is code assignment?
Code assignment is based on the provider’s documentation of the relationship between the condition and the care or procedure. The guideline extends to any complications of care, regardless of the chapter the code is located in. It is important to note that not all conditions that occur during or following medical care or surgery are classified as complications. There must be a cause-and-effect relationship between the care provided and the condition, and an indication in the documentation that it is a complication. Query the provider for clarification, if the complication is not clearly documented.
When coding the birth of an infant, assign a code from categories V30-V39, according to the?
When coding the birth of an infant, assign a code from categories V30-V39, according to the type of birth. A code from this series is assigned as a principal diagnosis, and assigned only once to a newborn at the time of birth.
When to use subcategory 733.1?
Subcategory 733.1 may be used while the patient is receiving active treatment for the fracture. Examples of active treatment are: surgical treatment, emergency department encounter, evaluation and treatment by
Organization of ICD-9-CM Volume 3
- ICD-9-CM procedure codes are two numeric digits followed by a decimal, which is then followed by another one or two digits. The codes begin with 00.01, to describe a therapeutic ultrasound of vessels in the head and neck, and they end with 99.99, which describes other miscellaneous procedures. ICD-9-CM indicates that leech therapy falls under 99.99...
Uses of ICD-9-CM Procedure Codes
- The Center for Medicare and Medicaid Services (CMS) which administrates the implementation of HIPAA, has offered clear guidance that Volume 3 procedure codes are only to be used in the inpatient setting to obtain reimbursement. CMS states that hospitals can use Volume 3 codes for internal tracking purposes, but the HIPAA standard is to use Healthcare Common Procedure Co…
Appropriate Use of ICD-9-CM Volume 3
- In the medical office setting, most billing software is loaded with a database of the complete set of ICD-9-CM codes, both diagnostic and procedural. Even if they are not appropriate, Volume 3 codes are available to medical billers and medical coders in the outpatient setting. Properly trained and certified medical coders and professional medical coders recogize the difference be…
Popular Posts:
- 1. icd 10 code for vertigo left ear
- 2. icd 10 code for eps side effects of medication
- 3. icd 10 code for acute on chronic abdominal pain
- 4. icd 10 code for ckd on hd
- 5. icd code for pain management
- 6. icd 10 code for polytopenia
- 7. what is the correct icd 10 code for status post laminectomy
- 8. 2017 icd 10 code for small airway disease infant
- 9. icd 10 cm code for om with effusion
- 10. icd 10 code for leiomyoma of uterus in pregnancy