What do you need to know about HCC coding?
- Monitor – the patient’s signs, symptoms, disease progression, disease regression;
- Evaluate – test results, medication effectiveness, response to treatment;
- Assess/Address – ordering tests, discussion, review records, counseling; and
- Treat – medications, therapies, other modalities ordered by the provider
What is HCC coding guidelines?
When it comes to the actual coding of HCCs, there are three base steps involved:
- Validation of medical record eligibility
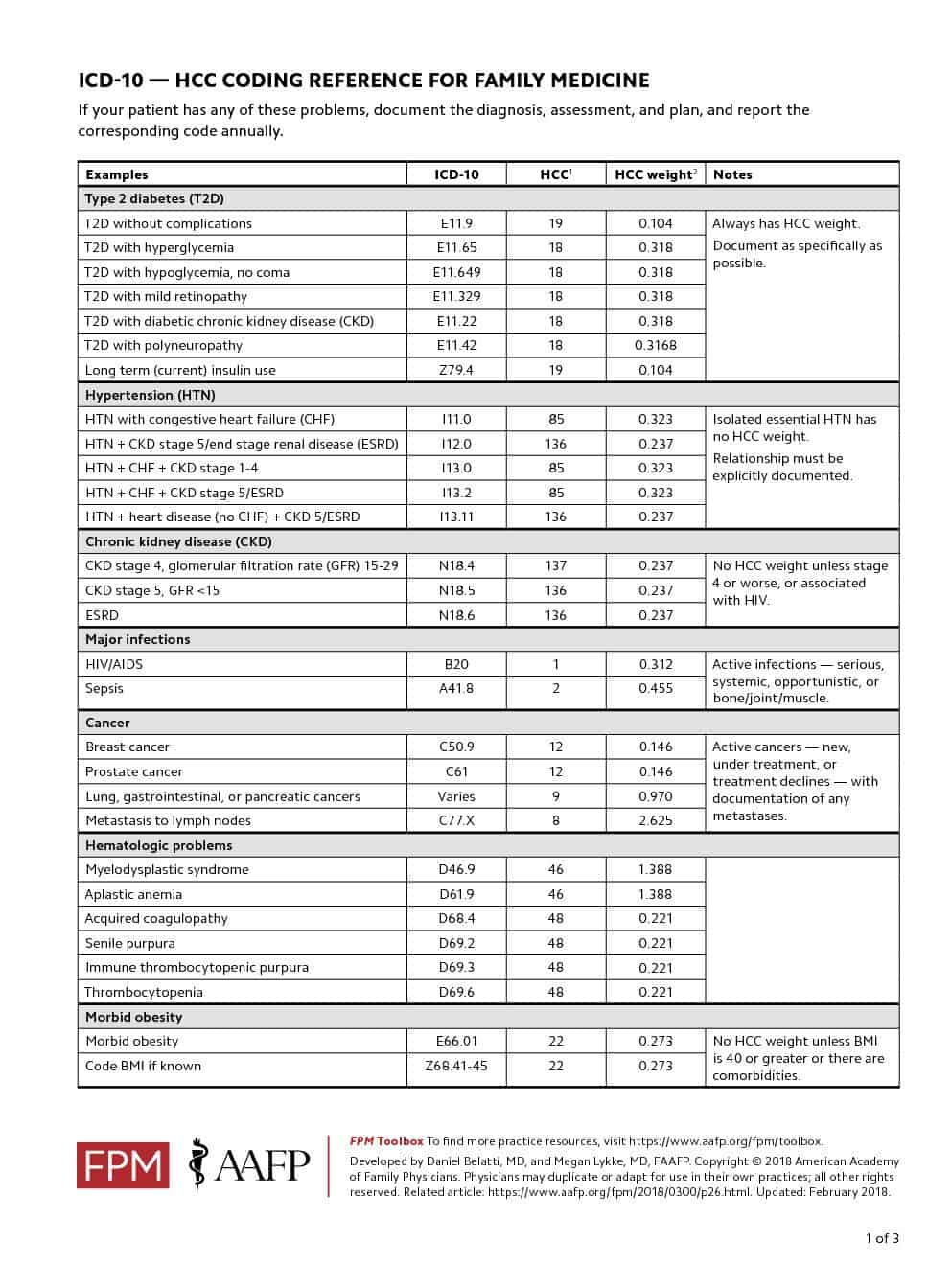
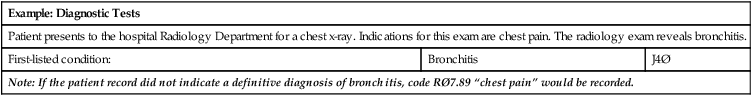
- Assignment of appropriate ICD-10-CM codes
- Submission of ICD-10-CM codes to CMS or HHS for reporting
What are the HCC codes?
HCC codes are a subset of ICD10 codes that Medicare uses to determine the risk scores of Medicare Advantage patients. HCC coding is a specific type of medical classification system used by health information technicians and medical billing and coding specialists. As an HCC coder, your job is to translate patient histories, symptoms, diagnoses ...
How to do HCC coding?
- Monitoring the patient’s symptoms and any signs of disease progression or regression
- Evaluating the patient’s response to medication and treatment
- Assessing ordered tests and reviewing patient records
- Treating a patient’s symptoms with medications and therapies
How many ICD-10 codes are there?
The usefulness of HCCs — not to mention future reimbursement for your practice — is reliant on the accuracy of your diagnosis coding. With approximately 70,000 diagnosis codes in ICD-10-CM, compared to the roughly 14,500 ICD-9-CM codes we are used to, this is no easy task.
What conditions should be coded for in a physician?
Physicians should code for all documented conditions that coexist at the time of the encounter/visit, and require or affect patient care treatment or management. Do not code conditions that were previously treated and no longer exist.
Is computer assisted physician documentation a replacement for human interaction?
Although not a viable replacement for human interaction, computer-assisted physician documentation, coding, and documentation improvement technology also can enhance productivity and accuracy.
Can a history code be used as a secondary code?
However, history codes may be used as secondary codes if the historical condition or family history has an impact on current care or influences treatment. Co-existing conditions include chronic, ongoing conditions, such as diabetes, congestive heart failure, atrial fibrillation, COPD, etc.
What does HCC mean in medical coding?
So, what does HCC stand for in medical coding? The Hierarchical Condition Categories (HCC) is a risk-adjustment model that has existed for many years. With the introduction of the Medicare Advantage Plans and its requirement of RAF reimbursement scores, the HCC has become more popular.
What are the main categories of HCC?
The main HCC categories are bipolar disorders, pulmonary disease, diabetes, congestive heart failure, rheumatoid arthritis, prostate & breast cancer and specified heart arrhythmias.
What does the Affordable Care Act do?
Here’s the deal…. The Affordable Care Act (ACA) ensures that insurance companies don’t give healthy patients cheap insurance plans. These are people who rarely visit the doctor, and this ensures that they do not inflate or deny cover for ill patients.
Can a physician document HCC?
While physician and other healthcare providers can document the services performed accurately, legibly and completely, collaborating with the right medical coding company with experience in HCC coding will ensure accurate code assignment.
Is HCC a good equalizer?
Therefore, the HCC is a great equalizer. Before the rise of the risk adjustment model, reimbursement was solely based on demographic factors. Costs may vary widely among patients. As such, risk adjustment can be used to evaluate patients on an equal scale.
What are HCCs?
HCCs, or Hierarchical Condition Categories, are sets of medical codes that are linked to specific clinical diagnoses. Since 2004, HCCs have been used by the Centers for Medicare and Medicaid Services (CMS) as part of a risk-adjustment model that identifies individuals with serious acute or chronic conditions. This allows Medicare to project the expected risk and future annual cost of care. Each HCC represents diagnoses with similar clinical complexity and expected annual care costs.
How and by whom are HCCs used?
HCCs are used to calculate payments to healthcare organizations for patients who are insured by Medicare Advantage (MA) plans, Accountable Care Organizations (ACOs), some Affordable Care Act (ACA) plans and many more. Clinicians add HCCs to a patient’s medical record along with supporting documentation as required by CMS.
How does HCC affect healthcare?
HCCs directly impact the amount of money received by healthcare organizations from the largest single payer in healthcare, CMS. Patients with high HCCs are expected to require intensive medical treatment, and clinicians that enroll these high-risk patients are reimbursed at higher rates than those with enrollees who have low HCCs. Organizations who do not document HCC codes properly or to the highest specificity will not receive these additional reimbursement amount for applicable patients.
How many HCC codes are there in 2020?
HCC codes represent costly chronic health conditions, as well as some severe acute conditions. As of 2020, there are 86 HCC codes, arranged into 19 categories. These 86 codes are comprised of 9,700 ICD-10-CM codes, each representing a singular medical condition. The top HCC categories include major depressive and bipolar disorders, asthma and pulmonary disease, diabetes, specified heart arrhythmias, congestive heart failure, breast and prostate cancer, and rheumatoid arthritis.
How much is the bonus for HCC code 19?
For example, diabetes with no complications, HCC code 19, pays a $894.40 premium bonus, while diabetes with ESRD, requires 2 HCC codes, 18 and 136, and has a bonus of $1273.60. The ability to document with greater precision can dramatically impact payment amounts.
What is a RAF score and what does it have to do with HCCs?
A Risk Adjustment Factor, known as a RAF score, is a measure of the estimated cost of an individual’s care based on their disease burden and demographic information. The RAF score is then used to calculate payments to healthcare organizations. Each HCC associated with a patient is assigned a relative factor that is averaged with any other HCC code factors and a demographic score. The resulting score is then multiplied by a predetermined dollar amount to set the per-member-per-month (PMPM) capitated reimbursement for the next period of coverage. The PMPM is the payment amount a provider receives for a patient enrolled in an MA plan regardless of services provided. Healthier patients will have a below average RAF while sicker patients will have a higher one, which impacts the calculated payment amount. Scores are calculated on an annual basis.
Popular Posts:
- 1. 2016 icd 10 code for straightening cervical lordosis
- 2. icd 10 code for recent bka
- 3. icd 10 code for opportunistic infection
- 4. icd-10 code for nexplanon complication
- 5. icd 10 code for nail injury
- 6. icd 9 code for hairline fracture
- 7. icd 10 code for paranoid behavior
- 8. icd 10 code for compression fracture of spine
- 9. icd 10 code for lump of left foot
- 10. icd 10 code for ca right breast