What is the ICD 10 code for endoscopy and colonoscopy?
However, the endoscopy or colonoscopy is normal. The diagnosis codes used default to the signs and symptoms based on ICD-10 guidelines - coding signs and symptoms if no definitive diagnosis at end of encounter. There is a discussion about the use of K31.89 (other diseases stomach/duodenum) or K59.9 (functional intestinal disorder).
What is the CPT code for colonoscopy with malignant neoplasm?
The patient is eligible for a screening colonoscopy. Reportable procedure and diagnoses include: Z12.11, encounter for screening for malignant neoplasm of colon The HCPCS code is the correct code to use—not the CPT ® code—because the patient is a Medicare patient. Additionally, G0121 is selected because the patient is not identified as high risk.
What is the ICD 10 code for neoplasm of colon?
Encounter for screening for malignant neoplasm of colon. 2016 2017 2018 2019 2020 Billable/Specific Code POA Exempt. Z12.11 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2020 edition of ICD-10-CM Z12.11 became effective on October 1, 2019.
What is the ICD 10 code for colonoscopy with stoma?
Report 45378 with ICD-10 code Z86.010 on the first line of the CMS 1500 form. • If the procedure is performed through a stoma rather than the anus, report 44388 - 44408: 44388 Colonoscopy through stoma 44389 Biopsy

What is the ICD-10 code for colonoscopy?
A screening colonoscopy should be reported with the following International Classification of Diseases, 10th edition (ICD-10) codes: Z12. 11: Encounter for screening for malignant neoplasm of the colon.
What is the ICD-10 code for poor preparation for colonoscopy?
If the procedure was cancelled due to poor bowel preparation, and the admission meets criteria for reporting, then a code from Z53. - Persons encountering health services for specific procedures, not carried out can be assigned.
How do I code a Medicare screening colonoscopy?
G0121 – Colorectal cancer screening; colonoscopy on individual not meeting criteria for high risk.G0105 – Colorectal cancer screening; colonoscopy on individual at high risk.G0104 – Colorectal cancer screening; flexible sigmoidoscopy.
Do you use Z12 11 on surveillance colonoscopy?
Report Z01. 818 (Encounter for other preprocedural examination) as the first-listed diagnosis code. Since the screening colonoscopy/sigmoidoscopy is not performed at this encounter, Z12. 11 is not an appropriate diagnosis code.
What is the procedure code for a colonoscopy?
Group 1CodeDescription45378COLONOSCOPY, FLEXIBLE; DIAGNOSTIC, INCLUDING COLLECTION OF SPECIMEN(S) BY BRUSHING OR WASHING, WHEN PERFORMED (SEPARATE PROCEDURE)45379COLONOSCOPY, FLEXIBLE; WITH REMOVAL OF FOREIGN BODY(S)45380COLONOSCOPY, FLEXIBLE; WITH BIOPSY, SINGLE OR MULTIPLE22 more rows
What is the ICD 10 code for colon polyps?
ICD-10 code K63. 5 for Polyp of colon is a medical classification as listed by WHO under the range - Diseases of the digestive system .
What is the difference between a diagnostic colonoscopy and a screening colonoscopy?
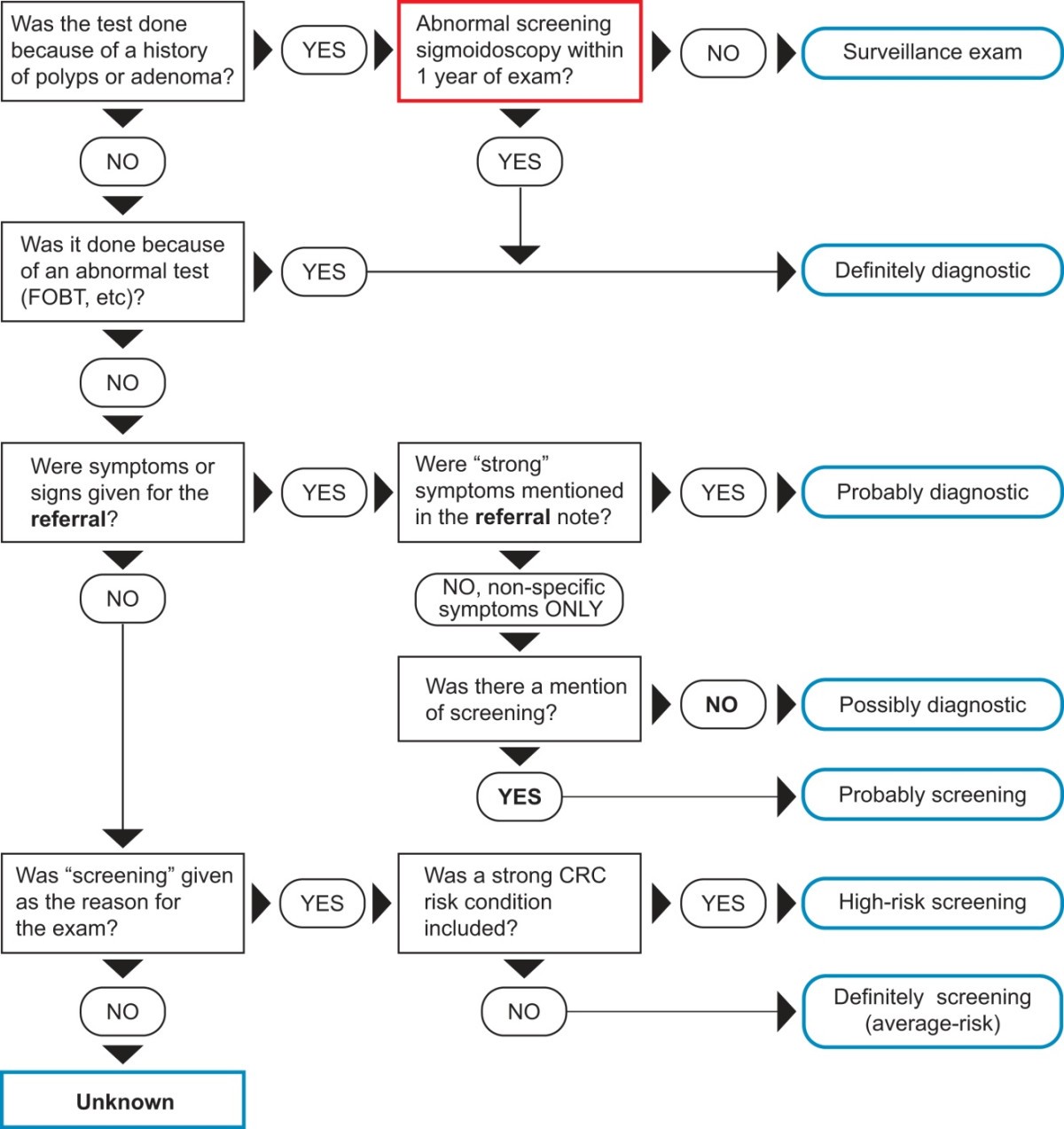
A screening colonoscopy will have no out-of-pocket costs for patients (such as co-pays or deductibles). A “diagnostic” colonoscopy is a colonoscopy that is done to investigate abnormal symptoms, tests, prior conditions or family history.
Does Medicare cover colonoscopy procedure?
Colonoscopies. Medicare covers screening colonoscopies once every 24 months if you're at high risk for colorectal cancer. If you aren't at high risk, Medicare covers the test once every 120 months, or 48 months after a previous flexible sigmoidoscopy. There's no minimum age requirement.
Is a colonoscopy considered a diagnostic test?
A colonoscopy is considered diagnostic when you've had: Signs or symptoms in the lower gastrointestinal tract noted in your medical record before the procedure, including: Abdominal pain that doesn't improve. Anemia.
When should Z12 11 be used?
If the patient presents for a screening colonoscopy and a polyp or any other lesion/diagnosis is found, the primary diagnosis is still going to be Z12. 11, Encounter for screening for malignant neoplasm of colon. The coder should also report the polyp or findings as additional diagnosis codes.
How do you report a screening colonoscopy performed on a 65 year old Medicare patient?
Report a screening colonoscopy for a Medicare patient using G0105 (colorectal cancer screening; colonoscopy on individual at high risk) and G0121 (colorectal cancer screening; colonoscopy on individual not meeting the criteria for high risk).
How do I bill 82270 to Medicare?
A written order from the physician responsible for using the results of the test in the management of the beneficiary's medical condition is required for Medicare coverage of this test. A health care provider gives a fecal occult blood test card to the beneficiary, who takes it home and places stool samples on it.
Does Medicare pay for CPT code 82270?
Effective on or after January 1, 2007, CPT code 82270 will be used for billing and payment purposes by Medicare for screening FOBT.
What is the difference between 45378 and 45380?
A family of CPT codes applies to colonoscopy. For example, code 45378 applies to a colonoscopy in which no polyp is detected, while codes 45380-45385 apply to colonoscopy that involves an intervention (e.g., 45385 is the code for colonoscopy with polypectomy.)
What is the HCPCS code for colonoscopy?
For Medicare beneficiaries, screening colonoscopy is reported using the following HCPCS codes: - G0105 (Colorectal cancer screening; colonoscopy on individual at high risk), for a Medicare beneficiary at high risk for colorectal cancer, and the appropriate diagnosis code that necessitates the more frequent screening.
What is the ICD-10 code for colonoscopy without biopsy?
Point to note: Code 45378 is the base code for a colonoscopy without biopsy or other interventions. It includes brushings or washings if performed. Report 45378 with ICD-10 code Z86.010 on the first line of the CMS 1500 form.
How often does Medicare require colonoscopy?
Medicare beneficiaries without high-risk factors are eligible for a screening colonoscopy every ten years. Beneficiaries at higher risk for developing colorectal cancer are eligible for screening once every 24 months. Medicare considers an individual who is at high risk of developing colorectal cancer as one who has one or more of the following:
How effective is colonoscopy?
According to a study by the American Cancer Society, 90% colorectal cancer (CRC) cases are detected in individuals with over 50 years in the U.S and colonoscopy is the most effective and the most commonly adopted procedure for the diagnosis and screening of CRC in older adults.
Why do you need a colonoscopy?
A Screening colonoscopy is performed on person without symptoms in order to test for the presence of colorectal cancer or colorectal polyps. Even if a polyp or cancer is found during a screening exam, it does not change the screening intent.
What is colonoscopy examination?
CPT defines a colonoscopy examination as "the examination of the entire colon, from the rectum to the cecum or colon-small intestine anastomosis, and may include an examination of the terminal ileum or small intestine proximal to an anastomosis" as well.
Is GI endoscopy a Medicare Part B procedure?
For the calendar year (CY) 2017, CMS separated moderate sedation services from the majority of GI endoscopy procedures under Medicare Part B.
What is the code for colonoscopy?
Medicare uses Healthcare Common Procedure Coding System (HCPCS) codes for screening. For a patient of typical risk, the screening procedure is reported with HCPCS code G0121; for a patient at high risk, it is reported with HCPCS code G0105. Medicare has a separate modifier for situations in which polyps are found and removed during a screening colonoscopy. In these instances, the correct CPT code is used (for example, 45385), but with modifier PT. Medicare’s reimbursement policy for this type of case is the same as other payors; only the coding differs. Each endoscopist should review the policies of their insurance providers to be certain which system is used, especially for Medicare Advantage plans offered by commercial insurers.
What modifier is used for colonoscopy?
All colonoscopy procedures now include the provision of moderate sedation. Incomplete colonoscopies not reaching the splenic flexure are reported as flexible sigmoidoscopies. Incomplete screening or diagnostic colonoscopies that reach beyond the splenic flexure but not to the cecum are reported with modifier 53.
What does the modifier do in an endoscopist?
By using this modifier and the proper diagnosis codes, the endoscopist tells the payor that the diagnostic procedure is done for screening. The base value of the code is not subject to a copayment, but the patient may be required to remit a copayment for the additional cost of the therapeutic procedure.
What is the difference between screening and colonoscopy?
Much of the confusion with respect to coding for colonoscopy arises from the dichotomy between screening and diagnostic colonoscopy. Screening colonoscopy is defined as a procedure performed on an individual without symptoms to test for the presence of colorectal cancer or polyps. Discovery of a polyp or cancer during a screening exam does not change the screening intent. Surveillance colonoscopy is a subset of screening, performed at an interval less than the standard 10 years from the last colonoscopy (or sooner, in certain high-risk patients), due to findings of cancer or polyps on the previous exam. The patient in this case is also asymptomatic. Unlike the two procedures mentioned previously, a diagnostic colonoscopy allows physicians to evaluate symptoms, such as anemia, rectal bleeding, abdominal pain, or diarrhea.
What is Z12.11?
Z12.11: Encounter for screening for malignant neoplasm of the colon (note: it is important that the Z code is listed first)
Is colonoscopy considered an endoscopy?
Colonoscopy is no longer defined as endoscopy beyond the splenic flexure; to be considered a colonoscopy, the examination must be to the cecum (or to the enterocolic anastomosis if the cecum has been surgically removed). All colonoscopy procedures now include the provision of moderate sedation.
Is CPT code for colonoscopy revalued?
All Current Procedural Terminology (CPT) codes for colonoscopy were revised for 2015.* Several new CPT codes were introduced for interventional colonoscopy procedures, which were not valued for 2015; however, all of these codes have been valued for 2016 and are reimbursed by Medicare and private insurance plans. Several clarifications were made in the 2015 revision, including the following:
Popular Posts:
- 1. icd 10 code for anterior of the front body
- 2. icd-9-cm code for polypeuritis
- 3. icd-10 code for external cause for p
- 4. icd 10 code for kyphosis spine
- 5. icd 10 code for acute chronic renal failure
- 6. icd 10 code for stage 2 pressure ulcer lower back
- 7. icd 9 code for head and neck cancer
- 8. icd 10 code for hyperleukocytosis
- 9. icd code for paresthesia
- 10. icd 10 code for secondary cancer to liver