What are the symptoms of flash pulmonary edema?
Related Searches For Flash Pulmonary Edema Symptoms
- Top Suggestions For Flash Pulmonary Edema Symptoms. One of the main manifestations of flash pulmonary edema is that breathing suddenly becomes much more difficult.
- Pulmonary Edema Signs. ...
- Pulmonary Edema Nursing. ...
- Acute Pulmonary Edema Treatment. ...
- Heart Failure Pulmonary Edema. ...
- Flash Pulmonary Edema Causes. ...
- Pulmonary Edema Animation
What does medication cause flash pulmonary edema?
The alveolis become more permeable, allowing fluid to enter the alveoli space. Similarly, what drug causes flash pulmonary edema? Many drugs — ranging from illegal drugs such as heroin and cocaine to aspirin — are known to cause noncardiogenic pulmonary edema.
What is flash edema?
What is Acute (Flash) Pulmonary Edema? Acute pulmonary edema is the rapid accumulation of fluid within the tissue and space around the air sacs of the lung (lung interstitium). When this fluid collects in the air sacs in the lungs it is difficult to breathe. Acute pulmonary edema occurs suddenly and is life threatening.
What is treatment for pulmonary edema?
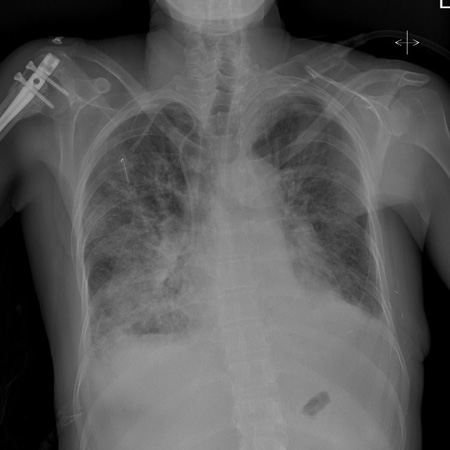
- Chest X-ray. ...
- Chest CT. ...
- Pulse oximetry. ...
- Arterial blood gas test. ...
- B-type natriuretic peptide (BNP) blood test. ...
- Other blood tests. ...
- Electrocardiogram (ECG or EKG). ...
- Echocardiogram. ...
- Cardiac catheterization and coronary angiogram. ...
- Ultrasound of the lungs. ...
What is flash pulmonary edema ICD-10?
J81. 0 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM J81.
Is flash pulmonary edema acute?
Abstract. Flash pulmonary edema (FPE) is a general clinical term used to describe a particularly dramatic form of acute decompensated heart failure.
Can you code pulmonary edema with CHF?
Some ICD-10-CM codes you may use for CHF and/or acute pulmonary edema include, but are not limited to: I50. 21, acute systolic (congestive) heart failure. I50.
Can PE cause flash pulmonary edema?
Acute pulmonary oedema is a well-described complication of pulmonary embolism. However, the relationship between these two conditions is not widely appreciated by physicians and the diagnosis of an underlying pulmonary embolism in patients with pulmonary oedema may well be missed.
What is the cause of flash pulmonary edema?
Flash pulmonary edema is caused by abrupt physiologic derangement such as a sudden increase in blood pressure, acute myocardial ischemia, acute myocarditis, acute valve dysfunction (e.g., mitral regurgitation), or arrhythmia.
How is flash pulmonary edema diagnosed?
A chest X-ray can confirm the diagnosis of pulmonary edema and exclude other possible causes of shortness of breath. It's usually the first test done when a health care provider suspects pulmonary edema. Chest computerized tomography (CT) scan. A chest CT scan gives more details about the condition of the lungs.
What is an acute pulmonary edema?
Acute pulmonary oedema is a medical emergency which requires immediate management. 1. It is characterised by dyspnoea and hypoxia secondary to fluid accumulation in the lungs which impairs gas exchange and lung compliance.
What code number is obtained for acute pulmonary edema?
J81. 0 - Acute pulmonary edema. ICD-10-CM.
Do you code fluid overload with CHF?
With respect to fluid overload and CCF, Coding Matters Volume 7 No 3 under Congestive heart failure advises it is not necessary to code fluid overload in a patient with CHF.
What is the difference between pulmonary embolism and pulmonary edema?
Blood clot in the lungs (pulmonary embolism). A blood clot moving from the blood vessels in the legs to the lungs can cause pulmonary edema.
What happens during flash pulmonary edema?
Based on Mr. Green's signs and symptoms, you suspect flash pulmonary edema, a life-threatening condition that occurs when fluid suddenly shifts from the pulmonary vasculature into the lung interstitium and alveoli. Pulmonary edema can be caused by pneumonia, MI, trauma, or inhalation of toxic chemicals.
How long does flash pulmonary edema last?
A blocked upper airway causes negative pressure in the lungs from trying to breathe through the blockage. With treatment, most people with this type of pulmonary edema recover in about 24 hours.
What is acute pulmonary oedema?
Acute pulmonary oedema is a medical emergency which requires immediate management. 1. It is characterised by dyspnoea and hypoxia secondary to fluid accumulation in the lungs which impairs gas exchange and lung compliance. 2.
Is flash pulmonary edema hypertensive emergency?
Often, "flash" pulmonary edema is related to a sudden rise in left-sided intracardiac filling pressures in the setting of hypertensive emergency, acute ischemia, new onset tachyarrhythmia, or obstructive valvular disease.
What causes pulmonary edema?
A buildup of fluid in the alveoli (air spaces) in the lungs. This keeps oxygen from getting into the blood. Pulmonary edema is usually caused by heart problems, but it can also be caused by high blood pressure, pneumonia, certain toxins and medicines, or living at a high altitude. Symptoms include coughing, shortness of breath, and trouble exercising.
What is the term for excessive accumulation of fluid in the lung?
Excessive accumulation of extravascular fluid in the lung, an indication of a serious underlying disease or disorder. Pulmonary edema prevents efficient pulmonary gas exchange in the pulmonary alveoli, and can be life-threatening.
When will the ICD-10 J81 be released?
The 2022 edition of ICD-10-CM J81 became effective on October 1, 2021.
What are the mechanisms of non-cardiogenic pulmonary edema?
Mechanisms for non-cardiogenic pulmonary edema include an increased capillary permeability and changes in pressure gradients within the pulmonary vasculature causing inflammation.
Is linking language required for pulmonary edema?
Although linking language is not required, it is best practice to link the etiology to acute pulmonary edema, leaving no question about its underlying cause and providers should be educated as such.
Can pulmonary edema be sudden?
The onset of acute pulmonary edema often has a sudden onset, but it can be gradual as well. A patient with acute pulmonary edema typically demonstrates a variety of symptoms such as shortness of breath, especially while lying flat or with activity, wheezing, bilateral infiltrates on chest x-ray, a feeling of drowning, tachypnea, tachycardia, dizziness, restlessness, anxiety/agitation, frothy and/or pink tinged sputum, cyanosis and a variety of additional symptoms based on the underlying etiology.
What are the mechanisms of non-cardiogenic pulmonary edema?
Mechanisms for non-cardiogenic pulmonary edema include an increased capillary permeability and changes in pressure gradients within the pulmonary vasculature causing inflammation.
Is linking language required for pulmonary edema?
If the documentation is unclear, clarification would be needed. Although linking language is not required, it is best practice to link the etiology to acute pulmonary edema, leaving no question about its underlying cause and providers should be educated as such.
Is pulmonary edema a cardiogenic etiology?
Therefore, acute pulmonary edema that has a cardiogenic etiology is not coded separately.
Can pulmonary edema be sudden?
The onset of acute pulmonary edema often has a sudden onset, but it can be gradual as well. A patient with acute pulmonary edema typically demonstrates a variety of symptoms such as shortness of breath, especially while lying flat or with activity, wheezing, bilateral infiltrates on chest x-ray, a feeling of drowning, tachypnea, tachycardia, dizziness, restlessness, anxiety/agitation, frothy and/or pink tinged sputum, cyanosis and a variety of additional symptoms based on the underlying etiology.

Popular Posts:
- 1. icd 10 code for arthritis right hip
- 2. icd 10 code written on prescription for controlled substance in florida
- 3. icd 10 code for long term use of testosterone
- 4. icd 10 code for chronic bilateral knee osteoarthritis
- 5. icd 10 code for a camel toe
- 6. correct icd 10 code for correct code(s) for hypertension and chronic renal disease
- 7. icd 10 cm code for viral uri
- 8. icd 9 code for periprosthetic infection
- 9. icd 10 code for prostate cancer with bone mets
- 10. icd 10 code for monocytic leukemia