How to beat IgA nephropathy?
Signs and symptoms
- Severe flank/abdominal pain
- High blood pressure
- Hematuria (gross, frank, microscopic)
- Compromised immune system
- Edema in hands and feet
- Cola- or tea-colored urine
What is the cause of IgA nephropathy?
IgA nephropathy, or Berger’s disease, is a kidney disease caused by a buildup of abnormal IgA antibody. Over time, it leads to kidney damage or end-stage renal disease (ESRD) — kidney failure. Symptoms include hematuria, or blood in your urine. Medication can slow the disease’s progress.
Why do you get IgA nephropathy?
- Sex. In North America and Western Europe, IgA nephropathy affects at least twice as many men as it does women.
- Ethnicity. IgA nephropathy is more common in whites and Asians than it is in blacks.
- Age. IgA nephropathy most often develops between the late teens and late 30s.
- Family history. ...
What does IgA nephropathy stand for?
Immunoglobulin A Nephropathy, called IgAN for short, or Berger’s disease, is a condition that damages the glomeruli inside your kidneys and can cause kidney disease. What causes IgA Nephropathy? The causes of IgAN are not well understood. IgAN is not just a kidney disease.
What is the ICD-10 code for diabetic nephropathy?
ICD-10-CM Code for Type 2 diabetes mellitus with diabetic nephropathy E11. 21.
What is the ICD-10 code for Chronic renal disease?
9.
What is this code N18 9?
9: Chronic kidney disease, unspecified.
What is the ICD-10 code for elevated renal function?
ICD-10-CM Code for Abnormal results of kidney function studies R94. 4.
What is IgA nephropathy?
IgA nephropathy, also known as Berger's disease, is a kidney disease that occurs when IgA deposits build up in the kidneys, causing inflammation that damages kidney tissues. IgA is an antibody—a protein made by the immune system to protect the body from foreign substances such as bacteria or viruses.
What is the ICD-10 code for nephropathy?
Nephropathy induced by unspecified drug, medicament or biological substance. N14. 2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM N14.
What is the difference between ICD-10 code N18 31 and N18 32?
N18. 31- Chronic Kidney Disease- stage 3a. N18. 32- Chronic Kidney Disease- stage 3b.
Can you code nephropathy and CKD?
Do not assign a code for hypertensive CKD, as the hypertension would be coded separately. In addition, it would be redundant to assign codes for both diabetic nephropathy (E11. 21) and diabetic chronic kidney disease (E11. 22) as diabetic chronic kidney disease is a more specific condition."
When do you code Z99 2?
Z99. 2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What does diagnosis code R79 89 mean?
ICD-10 code R79. 89 for Other specified abnormal findings of blood chemistry is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
Is renal insufficiency the same as CKD?
Yes. In common usage, chronic kidney disease (CKD) and chronic renal failure are generally the same. "Failure" is generally reserved for Stage 5 CKD, but the terms are interchangeable.
What does elevated kidney function mean?
A higher than normal level may be due to: Blocked urinary tract. Kidney problems, such as kidney damage or failure, infection, or reduced blood flow. Loss of body fluid (dehydration) Muscle problems, such as breakdown of muscle fibers (rhabdomyolysis)
When will the ICd 10 D80.2 be released?
The 2022 edition of ICD-10-CM D80.2 became effective on October 1, 2021.
What is D50-D89?
D50-D89 Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism
What is IgA in nephropathy?
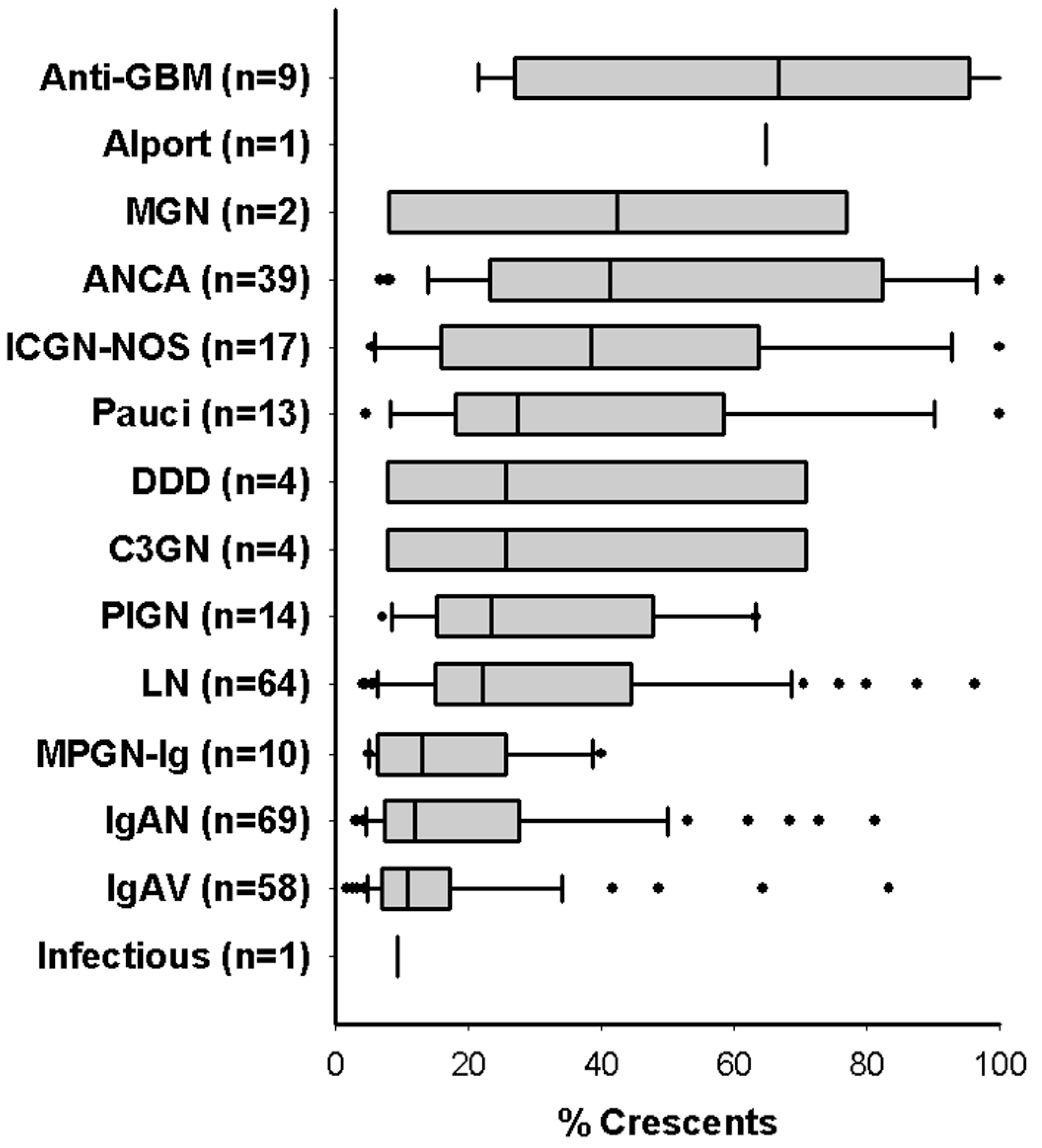
Immunoglobulin A (IgA) nephropathy: dominant or codominant mesangial IgA deposits in the absence of systemic diseases
What is S1P in kidneys?
S1 with podocyte hypertrophy and tip lesions (S1p): associated to higher proteinuria/24 h and worse renal survival in patients not treated with steroids ( Kidney Int 2017;91:235 )
How many glomeruli are in the renal cortex?
Specimen: A core of renal cortex containing up to 28 glomeruli in the planes of section.
Is nephropathy an IgA?
Comment: There is an IgA nephropathy with diffuse mesangial hypercellularity and focal segmental glomerulosclerosis with podocytopathic features. There is severe chronic tubulointerstitial damage. Oxford classification: M1 E0 S1p T2 C0.
What is IGA nephropathy?
About IGA Nephropathy Foundation. IgA Nephropathy is one of the most common and undetected kidney diseases and occurs when IGA – a protein that helps your body fight infections – settles in the kidneys. This disrupts your kidney’s ability to filter waste and excess water from your blood. Over time, these IGA deposits may cause blood ...
Why do IgA antibodies cause nephropathy?
IgA Nephropathy occurs when abnormal antibody immunoglobulin A’s (IgA) are produced . The exact reason why Abnormal IgA’s are produced is unclear, but genetic factors likely play an important role. The body produces other antibodies (IgG) to attack the IgA antibodies that it no longer recognizes as ‘self’. The IgG antibodies form a complex with the abnormal IgA antibodies and this complex often gets trapped at sites of filtration, specifically the kidneys. As a result, the body’s immune system attacks the abnormal IgA antibodies in the kidney, and affects the kidney’s ability to filter the wastes from your blood and produce healthy urine.
How to treat IgAN?
There is no proven treatment for IgAN. Your doctor’s recommendation as to whether to treat or not probably will be based on three factors: The severity of the lesions, as revealed by the biopsy; The degree of proteinuria (usually proteinuria greater than 2,000 mg/day warrants treatment); The creatinine clearance (if less than 70 ml/min [milliliters per minute], treatment is generally recommended). Doctors usually try to curb the acute inflammation signaled by heavy proteinuria. In severe cases, some employ high intravenous doses of methylprednisolone, a glucocorticoid that is anti-inflammatory and immunosuppressive. This is called "pulse therapy," and it is usually employed for only short periods. In less acute cases, most physicians use oral corticosteroids, like prednisone, which are also anti-inflammatory and which help to stabilize the glomerular basement membrane, making it less permeable to large protein molecules. Prednisone is given either daily or every other day to minimize its toxic side effects. Unfortunately, prednisone does not work in all cases, not is there any proof that it does much more than temporarily slow the disease process. Prednisone (or any corticosteroids) has potentially serious side effects when used long-term (e.g., bone damage and necrosis [tissue death], weakening of arm and leg muscles, peptic ulcers, diabetes or hyperglycemia, increased susceptibility to infection, cataracts, acne, weight gain, manic or even psychotic behavior, and lesser "cosmetic changes" such as a moon face). Its use needs to be thoroughly discussed with your nephrologist. Some doctors report that patients on prednisone seem to feel better than untreated patients, perhaps because prednisone makes them feel "up" and energized. On the other hand, some believe that using prednisone reduces chances of having a natural remission. Because immunosuppressants can reactivate even dormant viruses, transplant candidates are routinely tested for viruses. But IgAN patients in the early stages of the disease are not. Before going on prednisone or any other drug that suppresses the immune system, it is vital that you be tested for tuberculosis and for the possibility of a viral infection. Rather than testing for individual viruses such as Epstein-Barr (EBV), cytomegalovirus (CMV), or various herpes viruses, your doctor may want to order an immunoradiometric assay of alpha-interferon levels in your. An antiviral glycoprotein, alpha-interferon is usually undetectable in the blood of normal individuals; its presence, usually in high concentrations, is a fairly reliable indicator of a viral infection. Also inform your doctor if you’ve never had such diseases as measles or chickenpox or mumps. Immunosuppressive drugs can turn a mild childhood disease into a major threat. Other treatments than prednisone, based on other rationales, have been tried with little or no success. The anti-convulsive drug phenytoin (Dilantin) was found to lower levels of circulating IgA in the blood, but did nothing to alter the course of the disease. Anti-coagulants like warfarin and platelet inhibitors like dipyridamole have been employed, usually in combination with other drugs, because excessive clumping of blood platelets in the glomerular capillaries is suspected of being an accessory in damaging the kidneys. A gluten-free diet, adopted to remove food allergens that might be triggering the body's immune response, had some success but was difficult for many to follow. More recently, a low-antigen diet has shown promise. [See Should I follow a special diet?] Cytoxic drugs used in chemotherapy, like cyclophosphamide (Cytoxan), and drugs used to prevent organ rejection in transplants, such as azathioprine (Imuran) and cyclosporine (Sandimmune), are powerful immune suppressants that carry unacceptable risks for all but the most relentless cases. Unfortunately, the Network has received a number of reports over the years of such drugs being used on children without their parents being fully informed of the potential consequences, such as sterility. If you are not informed of ALL potential side effects of a treatment, there is no such thing as "informed consent." Plasmapheresis [a process in which such blood constituents as red blood cells are separated from the plasma and returned to a patient’s system] is widely used in Japan to treat immune-complex mediated diseases like IgAN, but doctors here question its usefulness. Removing immunoglobulins from the blood makes a patient more vulnerable to serious illness. It also removes clotting factor, raising the risk if hemorrhage in the event of injury. On the other hand, in cases of rapidly progressive IgAN, combinations of steroids, cytoxic drugs, and plasmapheresis may be helpful, at least temporarily. Another treatment that has enjoyed a certain vogue is the tonsillectomy. This may help those who are prone to sore throats and infected tonsils, but there is no proof it affects the course of IgAN. Chronically infected tonsils can also be treated by non-surgical means, such as homeopathy. You should discuss with your doctor ALL the potential side effects of any therapy proposed and carefully weight possible risks against possible benefits. There is no real proof that any currently used medical therapy is of any value in treating IgAN, at least among those who do not have the rapidly progressive form. Some have shown promise in ameliorating symptoms. None is curative. In relatively mild cases of IgAN, your doctor may recommend treatment with fish oil high in eicosapentanoic acid [EPA], which has anti-inflammatory properties and which may also lower plasma triglycerides and cholesterol. Results have been mixed, but many doctors believe this can be an effective anti-inflammatory if started early. [See Fish Oil] Fish oil is unlikely to have harmful side effects, but it does have anti-coagulant properties that can exacerbate heavy cases of gross hematuria. Of greater concern is the possibility of heavy metal or dioxin contamination, especially at the "standard" adult dosage of a whopping 12 g/day. You might wish to consider starting with a substantially smaller dose, such as 3 g/day, to see if produces the desired effects of reducing inflammation and proteinuria. Another possibility is to use flaxseed oil or perilla oil as alternatives. From vegetable sources, these oils are free of heavy metal or dioxin contamination, are high in EPA, and are more easily tolerated than fish oil, although you may need to take more of them to acquire the same concentrations of EPA. (A recent Consumer Reports survey of fish oil capsules found none that contained "significant" amounts of mercury, PCBs, or dioxin.) Because it is vital to treat hypertension if that is present initially or develops, your doctor may prescribe anti-hypertensive medication. Uncontrolled hypertension is strongly linked to more rapid progression of IgAN, perhaps because excessive pressures within the kidney strain already damaged glomerular capillaries. Hypertension can often be managed successfully through weight loss, low-fat diet, and regular aerobic exercise; in kidney disease, however, your doctor may have to try several medications before finding the right one. Diuretics are perhaps the least effective in controlling hypertension associated with renal disease. ACE inhibitors like enalapril (Vasotec) or ramipril (Altace) or beta-blockers are usually a better choice. They have been found to reduce the risk of kidney failure when compared to calcium channel blockers also used to control hypertension. Studies suggest that ACE inhibitors, by inhibiting the formation of the hormone angiotensin, help preserve the integrity of the glomerular membranes, making them less permeable and thereby decreasing proteinuria. They may also lessen the scarring of kidney tissue by interfering with the process that stimulates mesangial proliferation [excessive growth of mesangial cells]. Many doctors use ACE. inhibitors prophylactically, administering small doses even before hypertension appears. Dosage must be carefully monitored to avoid hypotension [extremely low blood pressure] and dizziness. The long-term effects of using ACE inhibitors in children are not clear. Patients may develop a chronic cough on the medication and have to switch to another anti-hypertensive drug. Hyperlipidemia is also associated with renal disease, and your doctor may wish to treat that with dietary changes or cholesterol-lowering drugs. It is important to reduce cholesterol levels to prevent heart disease; moreover, high cholesterol levels may aid the progression of IgAN. When lipids accumulate in the kidneys, possibly following injury to the mesangium, they are believed to contribute to scarring of the glomeruli. Again, treatment is a topic to be thoroughly discussed with your doctor. Cholesterol-lowering drugs, such as statins, can have dangerous side effects, including liver damage, memory loss, and rhabdomyolysis [a potentially fatal disease marked by destruction of skeletal muscle]. For a detailed discussion of statin drugs and other traditional means of lowering cholesterol, as well as alternatives to these, see the Life Extension Foundation, "Cholesterol Reduction" ( http://www.lef.org/protocols/prtcl-032.shtml ). The Life Extension Foundation sells nutritional supplements, but their research is thorough and reputable. Redflagsdaily.com, a health-oriented website started by Nicholas Regush, a Canadian journalist specializing in medical and scientific issues, has also explored problems with statins and other drugs; but to access this material requires subscribing the site.
What percentage of end stage renal disease is IgAN?
Others estimate that IgAN is responsible for 10-20% of all end-stage renal disease.
What is IGA in kidneys?
IgA Nephropathy is one of the most common and undetected kidney diseases and occurs when IGA – a protein that helps your body fight infections – settles in the kidneys. This disrupts your kidney’s ability to filter waste and excess water from your blood. Over time, these IGA deposits may cause blood and protein in your urine, high blood pressure and swollen hands and feet. It can appear suddenly or, most often, progresses slowly over many years and can result in end-stage kidney failure. By the time the symptoms of kidney failure occur (swelling in the hands and feet, nausea, fatigue, headaches and sleep problems), total kidney failure is near. When total kidney failure occurs, patients will need dialysis or a kidney transplant.Although the exact cause is unknown we do know that gender, age, ethnicity and family history may increase your chances of developing the disease. IGA Nephropathy is twice as likely to appear in men as women, can occur at any age but most likely strikes people in their 20s and 30s, is more common in Caucasians and Asians then in Blacks and, in certain cases, genetic factors may play a part in contributing to the disease. There is no current cure for IGA Nephropathy. And since the disease varies from one person to another there is no sure way of knowing the course the disease will take. This makes prescribing a specific treatment impossible. What works for one person may have virtually no effect on another. One thing is certain though, that once damaged the kidneys’ cannot be repaired. Since there is no cure, treatments now focus on slowing the progress of the disease and preventing complications. Medications currently being used include high blood pressure medications, immunosuppressants, omega 3 fatty acids and vitamin E supplements. It is estimated that as many as half of those affected with IGA Nephropathy will develop end-stage renal disease. When this occurs there are only two options; hemo dialysis for acute kidney failure and a kidney transplant for those with chronic kidney failure. While a transplant will greatly improve the quality of life, there is one large problem… there aren’t enough kidneys. And if that’s not bad enough, even with a transplant, there are no guarantees that the disease won’t return and infect the new kidney. Research is the answer, the only answer. Research into better understanding the causes of IGA Nephropathy will lead to better diagnosis which will lead to an eventual cure.
What does IgG mean in biology?
The body produces other antibodies (IgG) to attack the IgA antibodies that it no longer recognizes as ‘self’. The IgG antibodies form a complex with the abnormal IgA antibodies and this complex often gets trapped at sites of filtration, specifically the kidneys.
Is IGA more common in Caucasians than in Blacks?
IGA Nephropathy is twice as likely to appear in men as women, can occur at any age but most likely strikes people in their 20s and 30s, is more common in Caucasians and Asians then in Blacks and, in certain cases, genetic factors may play a part in contributing to the disease. There is no current cure for IGA Nephropathy.
Popular Posts:
- 1. icd 10 code for port-a-cath in place
- 2. icd 10 code for steroid induced osteoporosis
- 3. icd 10 code for tooth decay
- 4. icd 10 code for repeat c-section
- 5. icd 9 code for tdap immunization
- 6. icd 10 code for abn mammo
- 7. icd 9 code for abdominal pain from trauma
- 8. icd-9 code for slipping on a slick floor without falling
- 9. icd 10 code for normal postpartum
- 10. icd 9 code for fell playing football