Other intervertebral disc degeneration, lumbar region. M51.36 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2019 edition of ICD-10-CM M51.36 became effective on October 1, 2018.
Who is at risk for degenerative disc disease?
Who is at risk of degenerative disc disease? Anyone can experience degenerative disc disease, but several factors increase your risk, including being obese, smoking, experiencing an acute injury (like a fall), or being a woman. How is degenerative disc disease diagnosed?
Do I need surgery for degenerative disc disease?
Surgical treatment is an option in cases of severe, debilitating lumbar degenerative disc disease, and is usually only recommended after at least 6 months of nonsurgical treatment. Most cases of degenerative disc disease can be managed using nonsurgical methods, and do not require surgery for effective pain relief.
Can you use treadmill if you have disc degenerative disease?
You should avoid certain exercises if you have a degenerative disc. Exercise is some of the best medicine for back pain, and it can provide relief for degenerative disc disease. However, the wrong exercise can also exacerbate your condition. Avoid high-impact moves and those that involve heavy lifting at awkward angles.
What would be appropriate ICD-10-CM code for lumbar stenosis?
M48.061 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Spinal stenosis, lumbar region without neurogenic claud.
What is the ICD-10 code for lumbar disc degeneration?
M51. 36 Other intervertebral disc degeneration, lumbar region - ICD-10-CM Diagnosis Codes.
What is the ICD-10 code for degenerative changes?
According to Coding Clinic: “Assign code M16. 0—Bilateral primary osteoarthritis of hip for degenerative changes of hips”. Coding Clinic's rationale is, “ICD-10- CM's Alphabetic Index under “Degeneration, joint disease” instructs “see Osteoarthritis.”
Is degenerative disc disease a diagnosis?
How is degenerative disc disease diagnosed? A diagnosis is based on a medical history and a physical examination, as well as the symptoms and the circumstances where the pain started. Magnetic resonance imaging can show damage to discs, but it alone cannot confirm degenerative disc disease.
Is spinal stenosis and degenerative disc disease the same thing?
Discs often degenerate with age causing vertebrae to sit closer together. This is part of the reason we shrink with age. Degenerative discs can lead to pain via multiple pathways. Spinal stenosis is another condition of the spine where the central canal diameter is reduced much like a pipe that becomes clogged.
What is the ICD-10 code for chronic back pain?
ICD-10 Code M54. 5 for Chronic Low Back Pain | CareCloud.
How do you code degenerative changes in the spine?
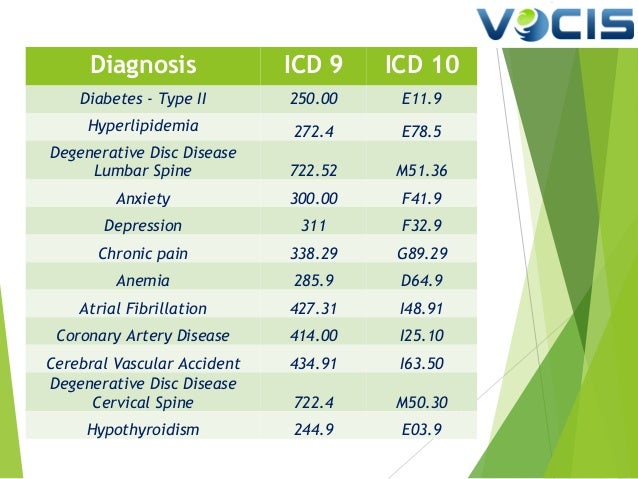
722.4 is the correct code for degenerative disease of the cervical intervertebral disc. 722.51 is the correct diagnosis code for thoracic degenerative disc disease. 722.52 is the accurate diagnosis code for DDD of the lumbar or lumbosacral intervertebral disc.
What is lumbar degenerative disc disease?
Lumbar degenerative disc disease is a condition that sometimes causes low back pain or radiating pain from damaged discs in the spine. A lumbar spinal disc acts as a shock absorber between vertebrae, and allows the joints in the spine to move easily.
What is lumbar disc disease?
Lumbar disk disease may occur when a disc in the low back area of the spine bulges or herniates from between the bony area of the spine. Lumbar disk disease causes lower back pain and leg pain and weakness that is made worse by movement and activity.
What is considered degenerative disc disease?
Simply put, degenerative disc disease refers to symptoms of back or neck pain caused by wear-and-tear on a spinal disc. In some cases, degenerative disc disease also causes weakness, numbness, and hot, shooting pains in the arms or legs (radicular pain).
Is arthritis and degenerative disc disease the same?
Degenerative joint disease is just another name for osteoarthritis, which is the most common type of arthritis – and it occurs when the components of a joint wear down. So whether we call it degenerative joint disease, osteoarthritis, or arthritis, we're really talking about the same condition.
Is degenerative disc disease also arthritis?
Yes. The phrase "degenerative changes" in the spine refers to osteoarthritis of the spine. Osteoarthritis is the most common form of arthritis. Doctors may also refer to it as degenerative arthritis or degenerative joint disease.
How many stages are there to degenerative disc disease?
The Four Stages of Degenerative Disc Disease They can result in pain, degenerative scoliosis, and loss of mobility. These four stages are the Dysfunction Stage, the Dehydration Stage, the Stabilization Stage, and the Collapsing Stage.
What is the T12-L1 code?
Though it is not specifically mentioned, “thoracolumbar” likely only includes T12-L1, and “lumbosacral” probably only refers to the L5-S1 interspace. There is a strange rule for cervical disc disorders indicating that you should code to the most superior level of the disorder.
Is sciatica a code for lumbar radiculopathy?
It is already included in the code. Likewise, don’t code sciatica (M54.3-) if you code for lumbar disc with radiculopathy. It would be redundant. On a side note, lumbar radiculopathy (M54.16) might be used if pain is not yet known to be due a disc, but it radiates from the lumbar spine.
Popular Posts:
- 1. icd 10 code for pus in throat
- 2. what is the icd 10 code for sah
- 3. icd 10 code for stress hyperglycemia
- 4. icd 10 code for osteochondritis dissecans right ankle
- 5. code in icd-10-cm for acute axasia
- 6. icd 10 code for right shoulder impingement
- 7. icd-10 code for left botrytis
- 8. icd 10 code for oa left hip
- 9. icd 10 code for leukorrhea in pregnancy
- 10. icd-10 code for admission for hemodialysis cause of acute renal failure