What is the diagnosis code for lower back pain?
What are some common causes of lower back pain?
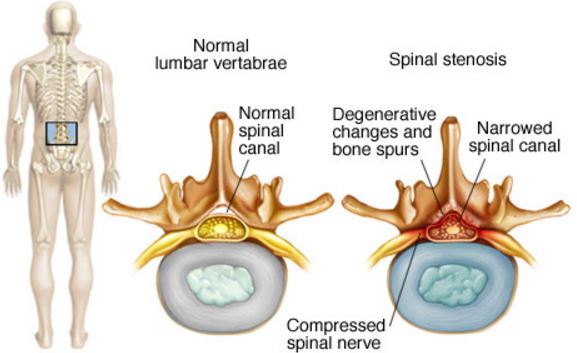
- Arthritis of the Spine. Arthritis of the spine — the slow degeneration of the spinal joints — is the most frequent cause of lower back pain.
- Back Injuries. A bad fall or a car accident can cause a lower back injury. ...
- Herniated Discs. A herniated, or bulging, disc is a disc that has “spilled out” of its lining. ...
What is the ICD 10 code for chronic back pain?
Other chronic pain
- G89.29 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM G89.29 became effective on October 1, 2021.
- This is the American ICD-10-CM version of G89.29 - other international versions of ICD-10 G89.29 may differ.
What is the CPT code for low back pain?
- RF of L5 dorsal primary ramus: 64635
- RF of S1 lateral branches: 64640
- RF of S2 lateral branches: 64640
- RF of S3 lateral branches: 64640
- Fluoroscopic needle guidance (Spinal): 77003 (for the S1-S3 nerve lateral branches, not the L5)
- Note: Use 724.6 (Disorder of the sacrum) and 721.3 (lumbar spondylosis) as the diagnostic codes
How do you code acute on chronic back pain?
- G89.0 Central pain syndrome Chronic Condition.
- G89.11-G89.18 G89.1 Acute pain, not elsewhere classified.
- G89.21-G89.29 G89.2 Chronic pain, not elsewhere classified.
- G89.3 Neoplasm related pain (acute) (chronic) Chronic Condition.
- G89.4 Chronic pain syndrome.
- G89.

What is the ICD-10 code for acute right sided low back pain without sciatica?
41.
What is the ICD-10 code for M54 50?
ICD-10-CM Code for Low back pain, unspecified M54. 50.
What does low back pain M54 5 mean?
5 – Low Back Pain. ICD-Code M54. 5 is a billable ICD-10 code used for healthcare diagnosis reimbursement of chronic low back pain. Its corresponding ICD-9 code is 724.2.
What is the difference between M54 5 and M54 50?
The current code, M54. 5 (Low back pain), will be expanded into three more specific codes: M54. 50 (Low back pain, unspecified)
What does diagnosis M54 16 mean?
M54. 16 - Radiculopathy, lumbar region | ICD-10-CM.
What does diagnosis code M54 9 mean?
9: Dorsalgia, unspecified.
What does diagnosis code M54 2 mean?
ICD-9 Code Transition: 723.1 Code M54. 2 is the diagnosis code used for Cervicalgia (Neck Pain). It is a common problem, with two-thirds of the population having neck pain at some point in their lives.
What diagnosis is M54 17?
17: Radiculopathy Lumbosacral region.
What does Dorsalgia mean in medical terms?
For starters, dorsalgia is severe back pain, which could be coming from different parts of the spine. Depending on the specific section of the spine where the pain is coming from, there are six types of dorsalgia. These are: Cervical. Cervicothoracic.
Is M54 59 valid diagnosis code?
ICD-10 Code for Other low back pain- M54. 59- Codify by AAPC.
What is the code for right flank pain?
Find Flank Under Abdominal in the Index Next to the entry for “Pain, abdominal,” there is the code R10. 9 Unspecified abdominal pain. If “flank pain” is all you have to work with from the documentation, then R10. 9 is the code to use.
Is M54 2 still valid?
M54. 2 is a billable/specific ICD-10-CM code used for Cervicalgia (Neck Pain). The 2021 edition of ICD-10-CM M54. 2 became effective on October 1, 2020.
Is M54 5 still valid?
ICD-10 code M54. 5, low back pain, effective October 1, 2021. That means providers cannot use M54. 5 to specify a diagnosis on or after October 1—and existing patients with the M54.
What is the diagnosis code for low back pain?
M54. 50 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M54.
What is the new ICD code for low back pain?
The Centers for Disease Control and Prevention (CDC) has designated an International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis code specifically for vertebrogenic low back pain. The new diagnosis code – M54. 51 – went into effect on October 1, 2021.
What does Vertebrogenic mean?
Vertebrogenic pain is a distinct type of chronic low back pain caused by damage to vertebral endplates, the interface between the disc and the vertebral body.
What is the term for pain in the lower back?
Sciatica – Pain which radiates down to one or both the legs from the lower back caused due to compression of the sciatic nerve by a herniated disk or a bone spur. Lumbago- The medical term for low back pain.
What is back pain called?
Back pain, medically called Dorsalgia is a very common physical discomfort affecting 8 out of 10 people both young and the old. The pain can be in the cervical, cervicothoracic, thoracic, thoracolumbar, Lumbar or lumbosacral regions. It can be felt as a dull, persistent ache or a sudden sharp pain.
Which region of the spine is curved slightly inwards and made of 5 vertebrae?
Lumbar region – The lower back region of the spine which is curved slightly inwards and made of 5 vertebrae (L1-L5). Lumbosacral region – The region connecting the last lumbar vertebrae to the sacrum which is made of 5 bones fused together.
How long does back pain last?
Chronic back pain – Back pain is said to be chronic if it is a constant nagging pain usually lasting for more than 3-6 months duration, which begins to affect the daily routine of the person.
Which region of the spine extends from the base of the neck to the abdomen?
Thoracic region – The longest region of the spine which extends from the base of the neck to the abdomen. It comprises of 12 vertebrae (T1 to T12).
Is back pain a symptom of a disease?
Back pain being a symptom of an underlying disease in most cases is coded only in the absence of a confirmed diagnosis of an underlying condition like intervertebral disc disorders, traumatic disc fracture, muscle strain etc..
What is the ICd 10 code for back pain?
The ICD 10 code M545 is used to define conditions connected with acute back pain (C & O lumbar pain, C & O back pain, or chronic back pain) or complaints about back pain or facet or joint pain. This code is used in common practice, internal medicine, and orthopedic works to define clinical ideas such as neck pain. Like the billable ICD 10 code, M545 is also used for medical diagnosis and compensation of chronic back pain.
Why does my back hurt?
The main cause of back pain may be an issue with the back itself or a problem with a different part of the body. Degenerative arthritis is a wear and tear method compared with age, injury, or genetic choice. Infection of intervertebral disc space within bones (osteomyelitis) in the abdomen or pelvis or bloodstream.
Can you code lumbar radiculopathy as M5416?
The instruction for ICD 10 CM states that if the problem of pain is known, the code is committed to the underlying diagnosis, not the pain code if the problem is known. For instance, if we encode lumbar radiculopathy as M5416, you can not allow M545 (lumbar pain) to this code. Although we report Radicullopathy as an ICD 10 code, we do not report the code for back pain.
What is the code for lower back pain?
This year, one of the major adjustments that relates to physical therapy practices is the removal of the code M54.5, which is generally used to document lower back pain. Lower back pain is the most common cause of disability in all age groups and accounts for one-fourth to one-third of all causes of disabilities. Lower back pain can be caused by injury, overuse or simply wear and tear on the structures related to normal spine function.
Why was M54.5 removed from the ICd 10?
Both R05 – Cough and R63.3 – Feeding difficulties were also slated for removal. Again, the reason given for removal of these codes is that each is too broad and doesn’t adequately describe a true diagnosis.
Is physical therapy a pain in the back?
There has been a recent development in the lives of providers and front office staff at therapy offices around the country, and to say it has been a pain in the back is to put it mildly. Beginning Oct. 1, one of the most common CMS codes used by physical therapy practices has been removed. This is not a rare occurrence, every year CMS releases a list of changes that are to be made to the Medicare program along with any other changes to the rules and regulations governing healthcare.
Is lower back pain a common complaint?
Lower back pain remains a common complaint for patients seeking treatment from physical therapists across the nation. This change has generated considerable concern among therapists that this move will eliminate payment for many treatments involving lower back pain diagnosis/treatment, including lumbar spine stabilization exercises. Keeping informed about the adjustment to how treatment for lower back pain should be coded though, should prevent any confusion.
Does the ICD-10 manual apply to Medicare?
Though CMS guidance on treatment coding technically only applies to reimburs ement from Medicare and Medicaid, the system has also been adopted by private insurers.
What does it mean when you feel a bad feeling in your back?
Sensation of unpleasant feeling indicating potential or actual damage to some body structure felt in the back.
How long does back pain last?
Acute back pain comes on suddenly and usually lasts from a few days to a few weeks. Back pain is called chronic if it lasts for more than three months. most back pain goes away on its own, though it may take awhile.
How long does it take for back pain to go away?
If your back pain is severe or doesn't improve after three days, you should call your health care provider. You should also get medical attention if you have back pain following an injury.treatment for back pain depends on what kind of pain you have, and what is causing it.
Where is chronic pain located?
Acute or chronic pain located in the posterior regions of the thorax, lumbosacral region, or the adjacent regions.
ICD-10 code M54.5 is soon to be a relic of the past
Last year was a wake up call—in more ways than one. The pandemic forced us to reckon...
ICD-10 code M54.5 is getting the kibosh
Every year, CMS publishes updates to the ICD-10 manual, deleting unnecessary codes, adding new ones, and revising language as-needed. This August, CMS published its latest round of ICD-10 changes—including the deletion of ICD-10 code M54.5, low back pain, effective October 1, 2021.
Providers will need to get specific, using more detailed (and sometimes new) ICD-10 codes to describe low back pain
So, here’s the real question: How the heck can CMS justify deleting such a commonly used code? Well, CMS has explained that it’s deleting M54.5 because it lacks specificity (and we all know how important coding specificity is to ICD-10).
Prepare for payer pushback
When CMS edits the ICD-10 manual, those changes apply to all payers—Medicare, state, and commercial alike. That said, some commercial payers don’t have the best track record when it comes to applying these changes in a timely manner.
Popular Posts:
- 1. icd 10 code for severe left leg pain,
- 2. icd 10 code for elevated mean cell volume
- 3. icd 10 code for diabetic hyperglycemic hyperosmolar syndrome
- 4. icd 10 code for tonic clonic epilepsy
- 5. icd 10 cm code for groin dermatitis
- 6. icd 10 code for myalgia due to statin
- 7. icd 10 cm code for subxiphoid pain
- 8. icd 10 code for allergic reaction to unknown substance
- 9. icd 10 code for ivf conception
- 10. icd 10 cm code for elevated blood pressure.