What is ICD - 9 code for severe back pain?
Chronic Back Pain ICD 9 Code Billable Medical Code for Chronic Pain Syndrome Diagnosis Code for Reimbursement Claim: ICD-9-CM 338.4 Code will be replaced by October 2015 and relabeled as ICD-10-CM 338.4. Known As
When to code chronic pain?
For general ICD 9 code for back pain, one always code for 724.5 and for ICD 10 the code is M54.9 which states a backache unspecified. Since the back pain doesn't specify whether it occurs in the lumbar or thoracic region we tend to code unspecified code for back pain to be on safer side.
What is ICD 9 diagnosis?
Mar 31, 2020 · The ICD-9-CM codes for chronic pain include: 338.21, chronic pain due to trauma. In ICD-10-CM, coders will report G89. 338.22, chronic post-thoracotomy pain. In ICD-10-CM, coders will report G89. 338.28, other chronic postoperative pain.
What is the diagnosis code for lower back pain?
ICD-9-CM Diagnosis Code 338.2 : Chronic pain Chronic pain 2015 Non-Billable Code There are 4 ICD-9-CM codes below 338.2 that define this diagnosis in greater detail. Do not use this code on a reimbursement claim. Clinical Information Aching sensation that persists for …
How do you code chronic back pain?
5 – Low Back Pain. ICD-Code M54. 5 is a billable ICD-10 code used for healthcare diagnosis reimbursement of chronic low back pain. Its corresponding ICD-9 code is 724.2.
What is the ICD-9 code for chronic pain?
ICD-9 Code 338.4 -Chronic pain syndrome- Codify by AAPC.
What is the ICD-10 code for back pain?
M54.9ICD 10 Code For Back Pain Unspecified. Whether back pain is unspecified or not otherwise classified, both conditions are used alternatively in the ICD 10 coding system, TheICD 10 Code For Back Pain Unspecified is M54. 9.
What is the ICD-10 code for unspecified chronic pain?
R52 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R52 became effective on October 1, 2021. This is the American ICD-10-CM version of R52 - other international versions of ICD-10 R52 may differ.
What is considered as chronic pain?
Chronic pain is long standing pain that persists beyond the usual recovery period or occurs along with a chronic health condition, such as arthritis. Chronic pain may be "on" and "off" or continuous.
What is the ICD 9 code for pain?
ICD-9-CM (2007 Version) “PAIN (338)” Codes.
What is ICD-10 code for thoracic back pain?
ICD-10 code: M54. 6 Pain in thoracic spine - gesund.bund.de.
What is the ICD-10 code for chronic?
Chronic Disease Death MICA - ICD-10 CodesCause of DeathICD-10 code(s)Other chronic liver disease and cirrhosisK73 - K74Chronic Obstructive Pulmonary Disease (COPD) excluding AsthmaJ40 – J47Bronchitis, chronic and unspecifiedJ40 - J42EmphysemaJ4365 more rows
How do you code pain management?
If the encounter is for pain control or pain management, assign the category 338 code followed by the specific site of pain. For example, an encounter for pain management for acute neck pain from trauma would be coded to 338.11 and 723.1.
What is the ICD-10 code for generalized pain?
ICD-10-CM Code for Myalgia M79. 1.
What is the medical term for back pain?
Low back pain, backache, lumbago or lumbar pain is a common disorder involving the muscles and bones of the back. Low back pain is often abbreviated as LBP.
How long does back pain last?
Acute back pain comes on suddenly and usually lasts from a few days to a few weeks. The clinical definition of back pain is: A backache (back pain) is a disorder characterized by marked discomfort sensation in the back region. Back pain is called chronic if it lasts for more than three months. It can be an acute or chronic pain located in ...
Where is back pain located?
It can be an acute or chronic pain located in the posterior regions of the thorax, lumbosacral region, or the adjacent regions. Most back pain leaves all alone, however, it might take a little while. Assuming control over-the-counter pain relievers and resting can offer assistance.
What is the ICd 9 code for back pain?
ICD-9CM codes are used in medical billing and coding to describe diseases, injuries, symptoms and conditions. ICD-9CM 724.5 for backpain is one of the thousands of ICD-9 codes used in healthcare documentation.
How long can you stay in bed with back pain?
Be that as it may, staying in bed for more than 1 or 2 days can aggravate it. In the event that your back pain is serious or doesn't enhance following three days, you ought to call your medicinal services supplier.
How to treat back pain?
It might incorporate hot or cool packs, exercise, pharmaceuticals, infusions, reciprocal medicines, and in some cases surgery.
ICD-10 Code: M54.5 – Low Back Pain
ICD-Code M54.5 is a billable ICD-10 code used for healthcare diagnosis reimbursement of chronic low back pain. Its corresponding ICD-9 code is 724.2.
General ICD-10 Information
ICD (International Statistical Classification of Diseases and Related Health problems) is now on its 10th revision. ICD-10 codes are the byproduct of that revision. This medical classification list is generated by the World Health Organization (WHO), and is used to help healthcare providers identify and code health conditions.
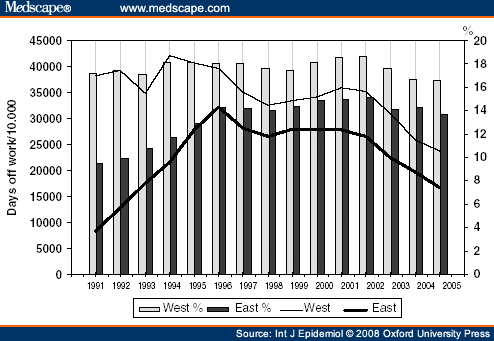
Why do people stay away from work?
Back pain, especially when it is chronic, could be very uncomfortable, reducing a person’s productivity. Chronic back pain could be resultant from several causes including certain medical conditions, injuries, and human activity.
What is the ICd 10 code for back pain?
The ICD 10 code for chronic back pain is M54.5 and it is used for diagnosis purposes. The code was introduced on October 1, 2018. This code is the American version and it is necessary that it is labeled thus. The reason is that there are several other international codes which could cause a conflict if you are not sure of the origin.
Why does my back hurt?
When the bones are porous and brittle, there is a greater risk of fractures. These are among the main causes of chronic back pain. Kidney stones. You could feel pain in your back if you have a kidney infection such as kidney stones. 3.
What causes back pain?
These are the most common causes of strains in the back. Muscle spasms. Strained ligaments or muscles. Damaged discs.
What is the back made of?
The back is made up of a complicated structure built of muscles, tendons, ligaments, bones, and discs. All of these work in tandem to give support to the body and aid movement. Different parts of the spine are cushioned by small structures known as discs. These discs are made of cartilage.
Where is the pain in the back?
In some cases it may be in the upper back while the most common are found in the lower back, sometimes extending to the buttocks and legs. With a little rest or corrective activity, the pain should go away.
What is the ICd 10 code for pain?
The ICD-10-CM Official Guidelines for Coding and Reporting provide extensive notes and instruction for coding pain (category G89). Review these guidelines in full. The following summary identifies key points.#N#When seeking a pain diagnosis, identify as precisely as possible the pain’s location and/or source. If pain is the primary symptom and you know the location, the Alphabetic Index generally will provide all the information you need.#N#Only report pain diagnosis codes from the G89 category as the primary diagnosis when: 1 The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or 2 The reason for the service is for pain control or pain management.
How long does a syringe last?
It can range from mild to severe and may last a few minutes or a few months. Acute pain typically does not last longer than six months and usually disappears when the physician identifies and treats the underlying cause or condition.
How long does chronic pain last?
Chronic pain may last for months or years, and may persist even after the underlying injury has healed or the underlying condition has been treated. There is no specific timeframe identifying when you can define the pain as chronic. Determine the code assignment based on provider documentation.
Who is John Verhovshek?
John Verhovshek, MA, CPC, is a contributing editor at AAPC. He has been covering medical coding and billing, healthcare policy, and the business of medicine since 1999. He is an alumnus of York College of Pennsylvania and Clemson University.

Popular Posts:
- 1. 2019 icd 10 code for leukocytosis
- 2. icd 10 code for screening for sexually transmitted disease
- 3. icd 10 code for motor vehicle accident, hitting a tree.
- 4. icd 10 code for transient leg weakness
- 5. 2018 icd 10 code for abrasion leg
- 6. what is the correct icd 10 code for a klebsiella
- 7. icd 10 code for breathlessness
- 8. icd 9 code for hemiplegia
- 9. icd 10 code for strep b
- 10. icd 10 code for mass in buttock