What is the diagnosis code for low back pain?
- BILLABLE CODE - Use M54.50 for Low back pain, unspecified
- BILLABLE CODE - Use M54.51 for Vertebrogenic low back pain
- BILLABLE CODE - Use M54.59 for Other low back pain
What is considered chronic low back pain?
Types of Back Pain: Acute Pain, Chronic Pain, and Neuropathic Pain
- Acute Pain Usually Lasts a Short Time. Pain that lasts less than 3 to 6 months, or pain directly related to tissue damage, is called acute pain.
- Chronic Pain Continues After Tissue Heals. ...
- Neuropathic Pain Has Distinct Symptoms. ...
What is the ICD 10 code for severe pain?
What is the ICD 10 code for severe pain? Pain, unspecified . R52 is a billable /specific ICD -10- CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for low back pain?
M54.5 is a non-billable ICD-10 code for Low back pain. It should not be used for HIPAA-covered transactions as a more specific code is available to choose from below. lumbago due to intervertebral disc displacement ( M51.2 -) A more specific code should be selected.
What is the diagnosis code for low back pain?
5: Low back pain.
What is the ICD-10 code for unspecified back pain?
ICD-10-CM Code for Dorsalgia, unspecified M54. 9.
What is the diagnosis code for chronic pain?
ICD-10 Code for Chronic pain syndrome- G89. 4- Codify by AAPC.
What is chronic low back pain?
Chronic back pain is defined as pain that continues for 12 weeks or longer, even after an initial injury or underlying cause of acute low back pain has been treated. About 20 percent of people affected by acute low back pain develop chronic low back pain with persistent symptoms at one year.
How do you code acute on chronic pain?
Category G89 includes codes for acute pain, chronic pain, and neoplasm-related pain, as well as codes for two pain syndromes. In order for you to assign these codes, the physician must document that the pain is acute, chronic, or neoplasm-related.
What is the ICD-10 code for acute right sided low back pain without sciatica?
41.
Can chronic pain be a primary diagnosis?
Only report pain diagnosis codes from the G89 category as the primary diagnosis when: The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or. The reason for the service is for pain control or pain management.
What is the ICD-10 code for pain?
ICD-10 code R52 for Pain, unspecified is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD-10 code for pain management?
The 2022 edition of ICD-10-CM G89. 18 became effective on October 1, 2021. This is the American ICD-10-CM version of G89.
What is the difference between acute and chronic lower back pain?
Acute back pain develops suddenly, often as a consequence of an identifiable injury. It can resolve within a matter of days, but may last up to six weeks. Chronic pain tends to develop more gradually over time, and it may become progressively worse.
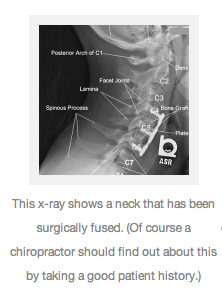
How is chronic back pain diagnosed?
Diagnosis. The doctor needs to decide if the pain comes from bones, muscles, nerves or an organ. The doctor will take a careful history and perform a physical examination. Imaging procedures to help identify where the pain is coming from include X-rays, bone scans, CT scan and MRI.
What is chronic LBA?
Low backache (LBA) is a common medical disorder, and 60%–80% of adults develop LBA sometime in their lifetime. It is the fifth most common cause to visit physician in the USA. [1,2] Chronic LBA (CLBA) is considered if continuous or fluctuating LBA continues for >3 months.
What is the term for pain in the lower back?
Sciatica – Pain which radiates down to one or both the legs from the lower back caused due to compression of the sciatic nerve by a herniated disk or a bone spur. Lumbago- The medical term for low back pain.
How long does back pain last?
Chronic back pain – Back pain is said to be chronic if it is a constant nagging pain usually lasting for more than 3-6 months duration, which begins to affect the daily routine of the person.
What is the longest region of the spine?
Cervicothoracic region – The region connecting the cervical and thoracic regions of the spine (C7-T1). Thoracic region – The longest region of the spine which extends from the base of the neck to the abdomen. It comprises of 12 vertebrae (T1 to T12).
Which region of the spine is curved slightly inwards and made of 5 vertebrae?
Lumbar region – The lower back region of the spine which is curved slightly inwards and made of 5 vertebrae (L1-L5). Lumbosacral region – The region connecting the last lumbar vertebrae to the sacrum which is made of 5 bones fused together.
Is back pain a symptom of a disease?
Back pain being a symptom of an underlying disease in most cases is coded only in the absence of a confirmed diagnosis of an underlying condition like intervertebral disc disorders, traumatic disc fracture, muscle strain etc..
Popular Posts:
- 1. icd 10 code for bilateral renal cyst
- 2. icd-10 code for malignant pericardial effusion
- 3. icd 10 code for trauma headache
- 4. icd 10 code for left foot surgical wound
- 5. icd 10 code for low platelet count
- 6. icd code for addenpathy
- 7. icd 10 code for decreased hdl
- 8. icd 10 cm code for worried well
- 9. icd 10 code for cmp screening picd
- 10. icd 10c cm code for elective induction of labor