What is the procedure code for suture removal?
Tips for coding suture removal:
- Suture removal using general anaesthesia is very rare; hence coder has to verify medical record thoroughly before using CPTs 15850 and 15851
- Avoid typo error when using CPT 99024. This can get easily mistaken with CPT 99204 which is EM visit level code.
- When the suture removal is performed within the global period, it is bundled with the surgery code.
Is removal of sutures covered by Medicare?
this code is not payable by Medicare. If your provider didn't place the sutures, (another provider NOT in his group did) and your provider is removing them - he should be coding an E/M (probably a low level) with the V-code suture removal. AND documentation so support his services of course!
Can You bill for suture removal?
Billing for suture removal depends on several factors. The intermediate and complex repair codes have a global period of 10 days for the surgeon/practice who performed the original repair. Your physician is not in the global period of the physician who performed the repair.
Do I code for suture removal?
There is no specific code for suture removal. If your provider put in the sutures and it is within the global period you use CPT 99024 No charge office visit. Subsequently, question is, where can I get suture removal? Removing staples and sutures is essential for proper wound healing and infection control.
How do I code for suture removal?
If the patient must be placed under general anesthesia to remove the sutures, you may report 15850 Removal of sutures under anesthesia (other than local), same surgeon or 15851 Removal of sutures under anesthesia (other than local), other surgeon.
Can you bill for suture removal?
The ICD-10 for suture removal would be used. If the physician originally placed the sutures it is not separately reportable. There is not a separate code that describes removal of sutures when the removal is not performed under anesthesia.
What is the global period for suture removal?
Billing for suture removal depends on several factors. The intermediate and complex repair codes have a global period of 10 days for the surgeon/practice who performed the original repair. Your physician is not in the global period of the physician who performed the repair.
What is the ICD-10 code for retained suture?
Other mechanical complication of permanent sutures, initial encounter. T85. 692A is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM T85.
Is suture removal included in laceration repair?
Follow-up suture removal is included in the laceration repair fee, but can be billed if the repair was performed elsewhere, such as in the emergency department.
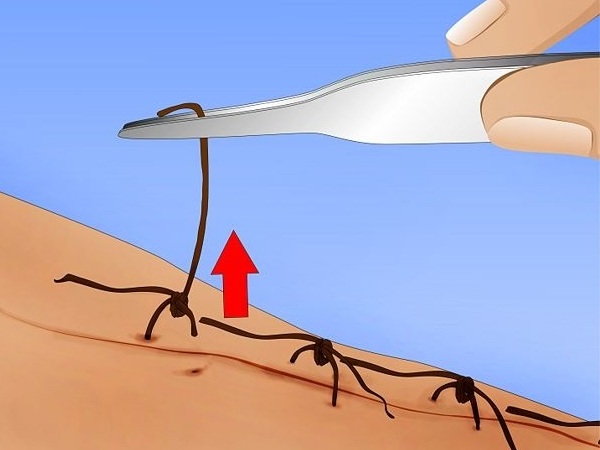
What is suture removal?
Suture removal is determined by how well the wound has healed and the extent of the surgery. Sutures must be left in place long enough to establish wound closure with enough strength to support internal tissues and organs. The health care provider must assess the wound to determine whether or not to remove the sutures.
Can you bill for cerclage removal?
Cerclage removals done in the office with a local anesthetic get billed as part of the level of service. It's just the E&M code.
What is the ICD 10 code for staple removal?
Z48. 02, Encounter for removal of sutures or staples (see ICD-10 Coding for Encounter for Removal of Sutures or Staples (icd10data.com)).
Does Medicare pay for suture removal?
There isn't a dedicated CPT® code for suture removal, and both the American Medical Association (AMA) and the Centers for Medicare & Medicaid Services (CMS) consider suture removal to be an integral part of any procedure that includes suture placement.
What is the ICD-10 code for wound check?
Encounter for change or removal of nonsurgical wound dressing. Z48. 00 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z48.
What is a retained foreign object?
A retained foreign body is a patient safety incident in which a surgical object is accidentally left in a body cavity or operation wound following a procedure (Canadian Patient Safety Institute (CPSI), 2016a).
What is the ICD-10 code for suture granuloma?
ICD-10-CM Diagnosis Code L92 L92.
What is the ICd 10 code for sutures?
Z48.02 is a valid billable ICD-10 diagnosis code for Encounter for removal of sutures . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
Do you include decimal points in ICD-10?
DO NOT include the decimal point when electronically filing claims as it may be rejected. Some clearinghouses may remove it for you but to avoid having a rejected claim due to an invalid ICD-10 code, do not include the decimal point when submitting claims electronically.
What is the CPT code for laceration repair?
If a patient comes for postoperative treatment such as Suture Removal during Global Period of a set of procedures (usually 10 days for minor surgical procedures such as laceration repairs, and 90 days for major surgical procedures), code the visit using CPT Code 99024 , and there will be no problem.
What is the difference between CPT and ICD?
CPT (Current Procedural Terminology) Codes are codes about diseases, health services, and procedures created by AMA (American Medical Association). On the other hand, ICD (International Classification of Diseases) Codes are also codes about diseases, health services, and procedures, but they are created by WHO (World Health Organization).
Can 99211 be billed for doctor service?
The code cannot be billed for doctor service. Also, to bill 99211, a provider should present (even if the person is only in the office and not seeing the patient) when the nurse or the medical assistant performs the service that may be a wound check, a dressing change, or suture removal.
Is suture removal a post operative procedure?
Suture removal is usually a post-operative procedure. Suture removal is a part of a series of procedures under one diagnosis or one health case. However, there are some cases that suture removal is reimbursed separately. CPT Code for Suture Removal can be quite confusing for the health administration staff, the physician, the patient, ...
Can you use Z codes for trauma?
Per coding guidelines, you will not use Z codes for aftercare for injury or trauma, you use the trauma code with the subsequent 7th character. so if the original injury was an open fracture then you use that code , if the injury was a closed fracture, you use that code with the 7th character indicating subsequent encounter.
Can you use Z48.02 aftercare code?
Z48.02 is an aftercare code and as such is not to be used for aftercare for a fracture.

Popular Posts:
- 1. icd 10 code for paresthesia of extremities
- 2. icd-9 code for malignant neoplasm of unspecified renal pelvis
- 3. icd 10 code for s/p hokins
- 4. icd 9 code for punctate keratitis
- 5. icd 10 code for arthritis rheumatoid
- 6. icd 10 code for homocysteine level
- 7. icd 10 code for r0989
- 8. icd 10 code for left hand cruch injury
- 9. what is the icd 10 code for peripheral edema
- 10. icd 10 code for accidental gsw