What is debridement of foot ulcer?
Preparation may include:
- physical exam
- measurement of wound
- pain medication (mechanical debridement)
- local or general anesthesia (sharp debridement)
What is treatment for infected ulcers?
Treatment
- Treatment team
- Reducing pressure. The first step in treating a bedsore is reducing the pressure and friction that caused it. ...
- Cleaning and dressing wounds. Care for pressure ulcers depends on how deep the wound is. ...
- Removing damaged tissue. To heal properly, wounds need to be free of damaged, dead or infected tissue. ...
- Other interventions. ...
- Surgery. ...
What is the ICD 10 code for foot ulcer?
Pressure ulcer L89-
- bed sore
- decubitus ulcer
- plaster ulcer
- pressure area
- pressure sore
How to treat infected diabetic foot ulcer?
To be extra careful, we suggest the preventable measures below:
- Take care of any cuts or wounds early before it gets infected
- Wash your feet every other day
- Keep feet dry and moisturized
- Keep toenails trimmed and keep good hygiene
- Change socks everyday
- Wear comfortable shoes
- Never walk barefoot outside
- Avoid alcohol and tobacco use
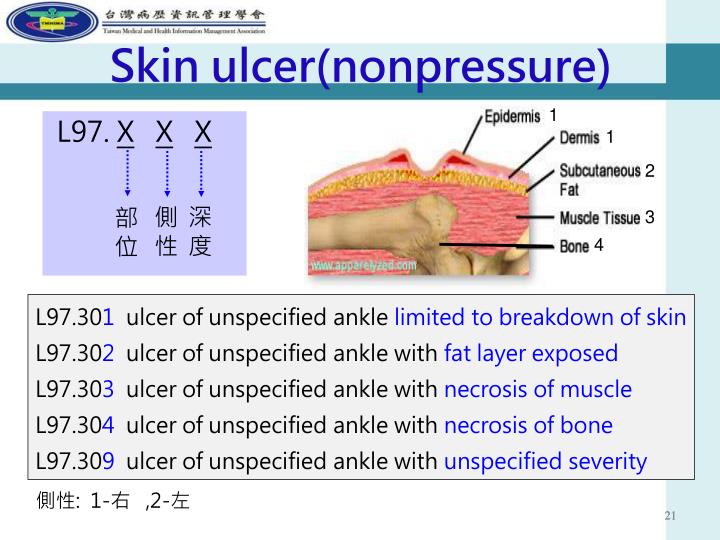
What is the ICD-10 diagnosis code for right foot ulcer?
519 for Non-pressure chronic ulcer of other part of right foot with unspecified severity is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
What is the ICD-10 code for ulcer of foot?
ICD-10-CM Code for Non-pressure chronic ulcer of other part of unspecified foot with unspecified severity L97. 509.
What is the ICD-10 code for right great toe ulcer?
Non-pressure chronic ulcer of other part of right foot limited to breakdown of skin. L97. 511 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L97.
What is the ICD-10 code for left foot ulcer?
ICD-10-CM Code for Non-pressure chronic ulcer of other part of left foot with unspecified severity L97. 529.
How do you code a foot ulcer?
Of these options, the most commonly used codes for diabetic foot ulcers are E10. 621 (Type 1 diabetes mellitus with foot ulcer) and E11. 621 (Type 2 diabetes mellitus with foot ulcer).
What is an ulcer on the foot?
Foot ulcers are open sores or lesions that will not heal or that return over a long period of time. These sores result from the breakdown of the skin and tissues of the feet and ankles and can get infected. Symptoms of foot ulcers can include swelling, burning, and pain.
What is the ICD-10 for diabetic foot ulcer?
ICD-10 code E11. 621 for Type 2 diabetes mellitus with foot ulcer is a medical classification as listed by WHO under the range - Endocrine, nutritional and metabolic diseases .
What is the ICD-10 code for foot care?
Routine foot care, removal and/or trimming of corns, calluses and/or nails, and preventive maintenance in specific medical conditions (procedure code S0390), is considered a non-covered service.
Is a neuropathic ulcer a pressure ulcer?
Neuropathic ulcers occur when a patient with poor neurological function of the peripheral nervous system has pressure points that cause ulceration through the epidermal and dermal tissue layers. This is a common condition in the foot, and occasionally other body parts.
Whats the difference between a pressure ulcer and a diabetic ulcer?
While diabetic patients can get pressure ulcers due to abuse or neglect in a nursing home, diabetic ulcers may appear in areas that are not typically subject to extended pressure—such as the bottoms of the feet when a resident has been lying down. In these cases, a diagnosis of a diabetic ulcer is more apt.
How do you code a venous stasis ulcer?
The stasis ulcer caused by venous insufficiency is captured first with the code for underlying disease (459.81) followed by the code for the location of the ulcer (707.13).
What is the difference between pressure ulcer and non-pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
Popular Posts:
- 1. icd 10 code for right mca stroke
- 2. icd 10 code for cervical stenosis of spinal canal
- 3. icd 10 code for deep vein thrombosis of leg
- 4. icd code for tobacco dependence
- 5. icd 10 cm code for pain syndrome
- 6. icd 10 code for aorta screening
- 7. icd 10 code for l2 burst fracture
- 8. icd-10 code for persistent atrial flutter
- 9. icd 10 cm code for cholelithiasis
- 10. icd 10 code for allergy to wasp sting