What is the CPT code for cerumen impaction removal?
| Code | Description |
|---|---|
| 69209 | REMOVAL IMPACTED CERUMEN USING IRRIGATION/LAVAGE, UNILATERAL |
| 69210 | REMOVAL IMPACTED CERUMEN REQUIRING INSTRUMENTATION, UNILATERAL |
| G0268 | REMOVAL OF IMPACTED CERUMEN (ONE OR BOTH EARS) BY PHYSICIAN ON SAME DATE OF SERVICE AS AUDIOLOGIC FUNCTION TESTING |
What is ICD 10 code for cerumen impaction?
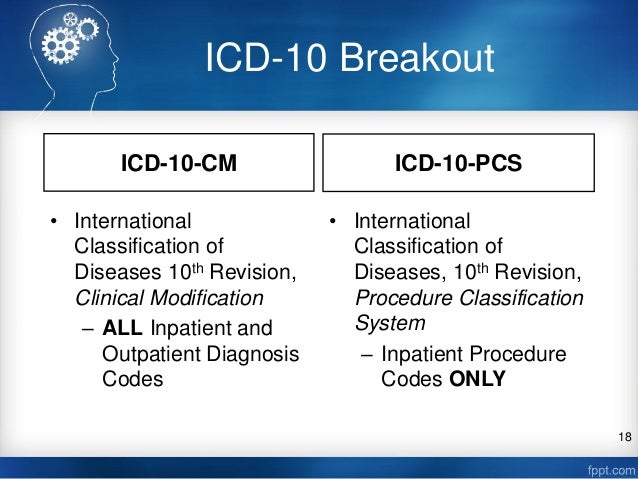
H61. 20 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM H61. 20 became effective on October 1, 2021.
What is the ICD 10 code for ear lavage?
What is the CPT code for ear wax removal?
How do you remove cerumen impaction?
How do you code bilateral cerumen removal?
What cerumen means?
: earwax. Other Words from cerumen Example Sentences Learn More About cerumen.
What is bilateral impacted cerumen?
What are the symptoms of impacted cerumen?
- Hearing loss.
- Earache.
- Sense of ear fullness.
- Itching in the ear.
- Dizziness.
- Ringing in the ears.
- Cough.
What is removal impacted cerumen requiring instrumentation unilateral?
What is the difference between CPT 69209 and 69210?
Can you bill an office visit with cerumen removal?
What modifier is used for non-covered services?
Effective from April 1, 2010, non-covered services should be billed with modifier –GA, -GX, -GY, or –GZ, as appropriate.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
What is the CPT code for cerumen removal?
CPT® guidelines tell us, “For cerumen removal that is not impacted, see E/M service code …” such as new or established office patient (99201-99215), subsequent hospital care (99231-99233), etc. In other words: If the earwax isn’t impacted, removal is included in the documented evaluation and management (E/M) service reported and may not be separately billed.#N#Per the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS), cerumen is impacted if one or more of the following conditions are present: 1 Cerumen impairs the examination of clinically significant portions of the external auditory canal, tympanic membrane, or middle ear condition; 2 Extremely hard, dry, irritative cerumen causes symptoms such as pain, itching, hearing loss, etc.; 3 Cerumen is associated with foul odor, infection, or dermatitis; or 4 Obstructive, copious cerumen cannot be removed without magnification and multiple instrumentations requiring physician skills.
What is the code for earwax removal?
Code 69210 only captures the direct method of earwax removal utilizing curettes, hooks, forceps, and suction. Another less invasive method uses a continuous low pressure flow of liquid (eg, saline water) to gently loosen impacted cerumen and flush it out … Code 69209 enables the irrigation or lavage method of impacted cerumen removal to be separately reported…
What is 69210 bilateral?
Both 69209 and 69210 are unilateral procedures . For removal of impacted earwax from both ears, append modifier 50 Bilateral procedure to the appropriate code. In the example above of the 7-year-old child, if irrigation occurred in both ears, appropriate coding is 69209-50.#N#When billing Medicare payers, different bilateral rules apply for 69210. The 2016 Medicare National Physician Fee Schedule Relative Value File assigns 69210 a “2” bilateral indicator. This means, for Medicare payers, the relative value units assigned to 69210 “are already based on the procedure being performed as a bilateral procedure.” In contrast to CPT® instructions, the Centers for Medicare & Medicaid Services (CMS) allows us to report only one unit of 69210 for a bilateral procedure. CMS does allow us to bill a bilateral procedure for cerumen removal by lavage using 69209-50.#N#Finally, note that some payers may stipulate “advanced practitioner skill” is necessary to report removal of impacted earwax (i.e., payers may require that a physician provide 69209, 69210). Query your individual payers to be certain of their requirements.
What is impact cerumen?
The AMA’s CPT® Changes 2016: An Insider’s View confirms, “Impacted cerumen is typically extremely hard and dry and accompanied by pain and itching. Impacted cerumen obstructing the external auditory canal and tympanic membrane can lead to hearing loss.”
Can you bill for wax removal on the same day as audio?
When Wax is removed on the same day as audio services, you can bill G0268 as long as the physician is the one who did the removal.
Can you report 69209?
You may report a single unit of either 69209 or 69210 (never both), per ear treated. As an example of proper reporting for 69209, CPT® Changes 2016: An Insider’s View provides the following:
Can you charge 69210 for irrigation?
Regarding Lee, you can charge 69210 being that you used currette as well as irrigation.
What is the CPT code for removal of impacted cerumen?
A new CPT code, 69209 , provides a specific billing code for removal of impacted cerumen using irrigation/lavage. Like CPT 69210, (removal of impacted cerumen requiring instrumentation, unilateral) 69209 requires that a physician or qualified healthcare professional make the decision to irrigate/lavage.
What is CPT code 69210?
A: The coder would report CPT code 69210 (removal impacted cerumen requiring instrumentation, unilateral) with modifier -50 (bilateral procedure) twice. Alternatively, the coder could report code 69210 twice with modifiers -LT (left side) and -RT (right side).
What is the code for cerumen removal?
Rather, most coders would recommend that code 69210 be reserved for use in situations where the cerumen removal takes significant effort by the physician. This is a situation where many individual payors have set different policies for application of this code, so it is best to check with individual payors for their policy.
What is cerumen impairing?
Visual considerations: Cerumen impairs exam of clinically significant portions of the external auditory canal, tympanic membrane, or middle ear condition.
When to use CPT code 69210?
As CMS cautioned in the Federal Register of June 29, 2006 (page 37233), “It is our understanding that CPT code 69210 is to be used when there is a substantial amount of cerumen in the external ear canal that is very difficult to remove and that impairs the patient’s auditory function. We will continue to monitor the use of this code for the appropriate circumstances.” To stay within the spirit of this definition, it seems best to avoid using this code for situations that only take a minute of the physician’s time to scoop out the wax. Rather, most coders would recommend that code 69210 be reserved for use in situations where the cerumen removal takes significant effort by the physician. This is a situation where many individual payors have set different policies for application of this code, so it is best to check with individual payors for their policy.
Is wax removal included in E/M?
A.A simplistic answer is that removing the wax is simply included in the emergency and management (E/M) code . The actual situation, however, is not quite so straightforward.
Is 69210 an E/M code?
By definition, however, 69210 always involves the diagnosis of impacted cerumen, so it seems reasonable to always attach the code for impacted cerumen ( 380.4) to the code 69210. Of course, the physician documentation should clearly demonstrate the presence of impacted cerumen, as defined above. If you are attempting to code an E/M code in addition ...
Popular Posts:
- 1. icd 10 code for elevated ldh
- 2. icd 10 code for patient was bitten by a brown recluse spider
- 3. icd-10 code for incareraton
- 4. icd 10 code for h/o colon polyps
- 5. what is the icd 9 code for nausea and vomiting
- 6. icd-10 procedure code for craniotomy
- 7. what is the icd 10 code for infant with sepsis due to e.coli
- 8. icd 10 cm code for lip chin laceration
- 9. icd 10 code for diabetes with ulcer foot right
- 10. icd code 10 for sob