What is the ICD 10 code for ulcer of the heel?
Pressure ulcer of unspecified heel, unspecified stage. L89.609 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2018/2019 edition of ICD-10-CM L89.609 became effective on October 1, 2018.
What is the ICD 10 code for pressure ulcer?
Ulcer, ulcerated, ulcerating, ulceration, ulcerative pressure (pressure area) L89.9- ICD-10-CM Diagnosis Code L89.9-. Pressure ulcer of unspecified site 2016 2017 2018 2019 2020 Non-Billable/Non-Specific Code. stage 1 (healing) (pre-ulcer skin changes limited to persistent focal edema) heel L89.6-.
Is Stage 3 necrotic decubitus ulcer of left heel associated with diabetes?
The provider's final diagnostic statement states, "stage 3 necrotic decubitus ulcer of left heel associated with diabetic neuropathy and peripheral vascular disease." Because the provider documented an association between diabetes and a decubitus ulcer, which condition would be sequenced as the principal diagnosis?
What is the ICD 10 code for ulcer of the cervix?
decubitus (trophic) ulcer of cervix (uteri) (. ICD-10-CM Diagnosis Code N86. Erosion and ectropion of cervix uteri. 2016 2017 2018 2019 2020 2021 Billable/Specific Code Female Dx. Applicable To.
What is the ICD-10 code for right heel Pressure ulcer?
ICD-10 Code for Pressure ulcer of right heel, unstageable- L89. 610- Codify by AAPC.
What is the ICD-10 code for Pressure ulcer left heel?
ICD-10 code L89. 62 for Pressure ulcer of left heel is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
What is the ICD-10 code for right heel wound?
ICD-10-CM Code for Unspecified open wound, right foot S91. 301.
What is the correct code for a Stage 2 Pressure ulcer of the right heel?
612.
Can you get a Pressure ulcer on your heel?
Heel pressure ulcers are caused by factors such as pressure, shear and friction and the vulnerability of the heel to pressure damage is increased by immobility, the patient's skin status, the presence of previous pressure ulcers and/or scar tissue, and suboptimal tissue perfusion.
What does a heel ulcer look like?
A foot ulcer can be shallow or deep. When it starts, it looks like a red crater or dimple on the skin. If it becomes infected, it can develop drainage, pus, or a bad odor. If you have nerve damage in your feet, then you won't notice the pain of a small stone, too tight shoes, or the formation of a foot ulcer.
What is a calcaneal ulcer?
Calcaneal wounds usually develop as a result of direct injury to the heel of the foot, obesity (continual pressure on the same area of the foot causes the ulcer to form) or diabetic complications.
How do you code a foot ulcer?
Of these options, the most commonly used codes for diabetic foot ulcers are E10. 621 (Type 1 diabetes mellitus with foot ulcer) and E11. 621 (Type 2 diabetes mellitus with foot ulcer). “Code first” indicates that an additional code is required, and it must be listed first.
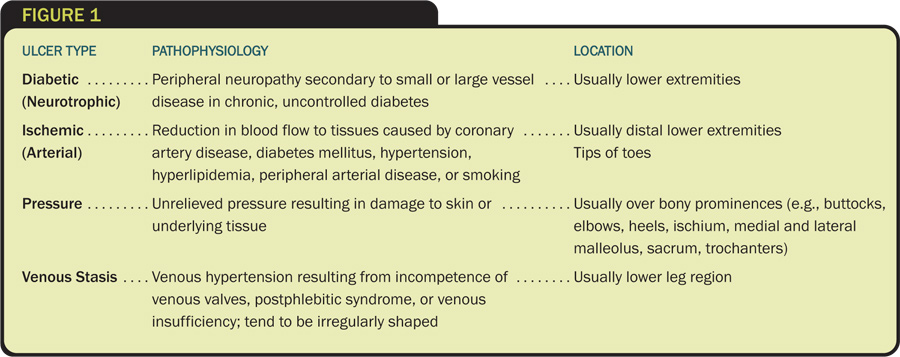
What is the difference between pressure ulcer and non-pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
What is the ICD-10 code for Pressure ulcer stage 2?
Pressure ulcer of unspecified site, stage 2 L89. 92 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L89. 92 became effective on October 1, 2021.
What is a Stage 1 Pressure ulcer?
Stage 1 pressure injuries are characterized by superficial reddening of the skin (or red, blue or purple hues in darkly pigmented skin) that when pressed does not turn white (non-blanchable erythema). If the cause of the injury is not relieved, these will progress and form proper ulcers.
What is the ICD-10 code for wound care?
This article addresses the CPT/HCPCS and ICD-10 codes associated with L37228 Wound Care policy.
How do you code a healing pressure ulcer?
A healed ulcer, on the other hand, does not need a code because it is an event that happened in the past, not a current event. Knowing where the treatment is for the ulcer will help you to determine if an ICD-10-CM code is needed or if you need more specificity on the ulcer's stage.
What are the characteristics of a Stage 2 wound?
At stage 2, the skin breaks open, wears away, or forms an ulcer, which is usually tender and painful. The sore expands into deeper layers of the skin. It can look like a scrape (abrasion), blister, or a shallow crater in the skin. Sometimes this stage looks like a blister filled with clear fluid.
What is the correct code for a stage 4 pressure ulcer of the left ankle?
Pressure ulcer of left ankle, stage 4 L89. 524 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L89. 524 became effective on October 1, 2021.
When the pressure ulcer stage is not documented how should the stage be coded?
When there is no documentation regarding the stage of the pressure ulcer, assign the appropriate code for unspecified stage (L89. 009).
What is an unstageable ulcer?
An unstageable ulcer is when the base of the ulcer is covered in eschar or slough so much that it cannot be determined how deep the ulcer is. This diagnosis is determined based on the clinical documentation. This code should not be used if the stage is not documented.
What is the sequence of a pressure ulcer?
The sequence depends on the pressure ulcer being treated. If all the pressure ulcers are being treated, sequence the code for the most severe pressure ulcer first. Example: A patient with a stage 3 pressure ulcer on her left heel and a stage 2 pressure ulcer of her left hip is scheduled for debridement.
What is pressure ulcer?
Pressure ulcers are areas of damaged skin and tissue developing as a result of compromised circulation. When a patient stays in one position without movement, the weight of the bones against the skin inhibits circulation and causes an ulceration of the tissue. Pressure ulcers usually form near the heaviest bones (buttocks, hips, and heels).
Where do pressure ulcers form?
Pressure ulcers usually form near the heaviest bones (buttocks, hips, and heels). There are stages of pressure ulcers that identify the extent of the tissue damage. Stage 1—Persistent focal erythema. Stage 2—Partial thickness skin loss involving epidermis, dermis, or both.
Can a pressure ulcer get worse?
If the pressure ulcer is healed completely , a code is not reported for the pressure ulcer. There are some cases where the pressure ulcer will get worse during the course of the admission. For example, the patient is admitted for treatment of a stage 2 ulcer that progresses to stage 3.
Who is John Verhovshek?
John Verhovshek, MA, CPC, is a contributing editor at AAPC. He has been covering medical coding and billing, healthcare policy, and the business of medicine since 1999. He is an alumnus of York College of Pennsylvania and Clemson University.
What percentage of diabetics have neuropathy?
After 10 years, ~90 percent of Type 1 and Type 2 diabetics have some degree of neuropathy, most commonly affecting the feet and legs, and 90 percent of diabetic foot ulcers have diabetic neuropathy as a contributing factor. If the diabetic doesn’t recognize discomfort due to nerve impairment, they may not adjust their shoes ...
What causes diabetic foot ulcers?
A “diabetic foot ulcer,” which is caused exclusively by hyperglycemia, in the absence of neuropathy or ischemia, is a rarity. That term almost always refers to an ulcer on the foot of a diabetic that derives from neuro/ischemic etiology, as opposed to being strictly and principally due to pressure injury.
What happens when blood sugar is low?
Poorly controlled blood sugars weaken the small blood vessel walls and predispose patients to arteriosclerosis. This impairs the circulation and causes ischemia of the soft tissues, especially of the lower extremities. Many diabetics have both diabetic peripheral neuropathy and angiopathy.
Why do diabetics get ulcers?
The American Podiatric Medical Association adds that “ (diabetic foot) ulcers form due to a combination of factors , such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes .”. They go on to note that “vascular disease can complicate a foot ulcer, ...
What is the L89 code for a pressure ulcer?
Pressure injuries with skin breakdown are considered pressure ulcers. An additional L89 code specifies the stage (depth of tissue injury) and the anatomical site. Pressure ulcers form in sites that experience shear or pressure, typically in tissue overlying bony prominences such as elbows, the sacrum, hips, or heels.
Why are pressure ulcers considered a patient safety indicator?
Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
What is the most common site of ulceration?
The plantar surface is the most common site of ulceration, especially at areas of bony prominence.”.
Why was gangrenous pressure ulcer admitted?
The primary reason for the admission was for treatment of the gangrenous pressure ulcer. This was not a diabetic ulcer. Diabetic ulcers typically involve the foot and toes. Pressure ulcers develop in tissue near bony prominences, such as the elbows, tailbone, greater trochanters, or heels.
Does diabetes mellitus cause pressure ulcers?
Although diabetes mellitus may increase the risk of pressure ulcers because of its association with neuropathy and angiopathy, ICD- 10-CM doesn’t classify pressure ulcers the same way as diabetic ulcers.

Popular Posts:
- 1. what is the icd 10 code for complication of double lung transplant
- 2. icd 10 code for scattered breast calcifications
- 3. icd 10 code for endocardial cushion defect
- 4. icd 10 cm code for renal turular necrosis
- 5. icd-10-cm code for chronic gouty arthritis of the right hip
- 6. icd 10 code for neurogenic pain
- 7. icd 10 code for dysgenesis of the corpus callosum
- 8. icd 9 code for lipid disorder abnornal lp
- 9. icd 10 code for vaginal vault prolapse
- 10. icd 10 cm code for acute respiratory failure due to severe viral sepsis