What is the ICd 10 code for angina?
Is Z86.79 a POA?
Is diagnosis present at time of inpatient admission?
About this website
How do you code syncope history?
Syncope is in the ICD-10 coding system coded as R55. 9 (syncope and collapse).
What is diagnosis code Z86 79?
ICD-10 code Z86. 79 for Personal history of other diseases of the circulatory system is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the 2021 ICD-10 code for syncope?
R55 - Syncope and collapse | ICD-10-CM.
What is the ICD-10 code for syncopal episodes?
ICD-10 code R55 for Syncope and collapse is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD-10 code for ASHD?
ICD-10 Code for Atherosclerotic heart disease of native coronary artery without angina pectoris- I25. 10- Codify by AAPC.
What is I10 diagnosis?
ICD-Code I10 is a billable ICD-10 code used for healthcare diagnosis reimbursement of Essential (Primary) Hypertension.
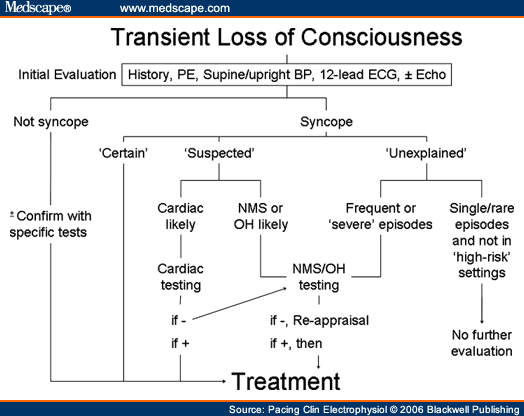
What are the 4 classifications of syncope?
OverviewAutonomic Nervous System (ANS)The ANS automatically controls many functions of the body, such as breathing, blood pressure, heart rate and bladder control. ... Vasovagal syncope (also called cardio-neurogenic syncope)Situational syncope.Postural syncope (also called postural hypotension)Neurologic syncope.More items...•
How do you code loss of consciousness?
Unspecified intracranial injury with loss of consciousness of unspecified duration, initial encounter. S06. 9X9A is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM S06.
Is syncope the same as fainting?
Syncope is a temporary loss of consciousness usually related to insufficient blood flow to the brain. It's also called fainting or "passing out."
What does DX R55 mean?
2022 ICD-10-CM Diagnosis Code R55: Syncope and collapse.
How do you code Presyncope?
ICD-10-CM Diagnosis Code O11 Pre-existing hypertension with pre-eclampsia,... O11. Pre-existing hypertension with pre-eclampsia,... O11. Pre-existing hypertension with pre-eclampsia,... O11. Pre-existing hypertension with pre-eclampsia,... O11. Pre-existing hypertension with pre-eclampsia,...
What is the ICd 10 code for angina?
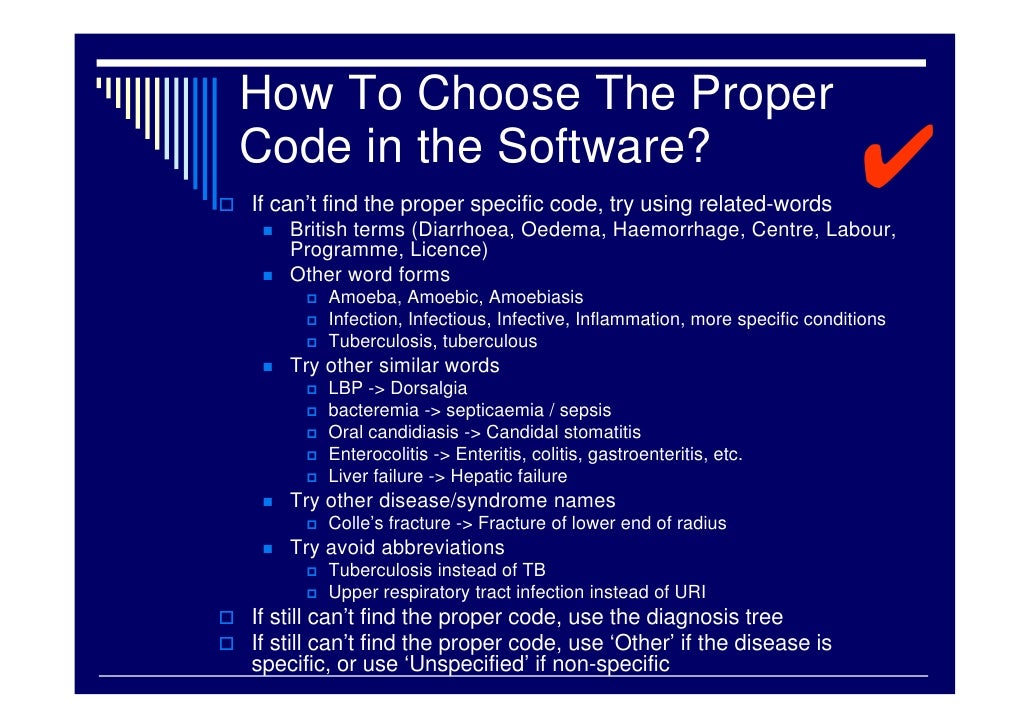
Z86.79 is a billable diagnosis code used to specify a medical diagnosis of personal history of other diseases of the circulatory system. The code Z86.79 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions.#N#The ICD-10-CM code Z86.79 might also be used to specify conditions or terms like attends hypertension monitoring, h/o ventricular fibrillation, h/o: angina in last year, h/o: angina pectoris, h/o: aortic aneurysm , h/o: atrial fibrillation, etc. The code is exempt from present on admission (POA) reporting for inpatient admissions to general acute care hospitals.#N#The code Z86.79 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
Is Z86.79 a POA?
Z86.79 is exempt from POA reporting - The Present on Admission (POA) indicator is used for diagnosis codes included in claims involving inpatient admissions to general acute care hospitals. POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement. Review other POA exempt codes here.
Is diagnosis present at time of inpatient admission?
Diagnosis was not present at time of inpatient admission. Documentation insufficient to determine if the condition was present at the time of inpatient admission. Clinically undetermined - unable to clinically determine whether the condition was present at the time of inpatient admission.
What is the ICd code for syncope?
R55 is a billable ICD code used to specify a diagnosis of syncope and collapse. A 'billable code' is detailed enough to be used to specify a medical diagnosis.
What are the symptoms of syncope?
These symptoms may include lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, and feeling warm, among others. Syncope may also be associated with a short episode of muscle twitching.
What is it called when you lose your consciousness?
Syncope , also known as fainting, passing out and swooning, is defined as a short loss of consciousness and muscle strength, characterized by a fast onset, short duration, and spontaneous recovery. It is due to a decrease in blood flow to the entire brain usually from low blood pressure. Some causes have prodromal symptoms before the loss of consciousness occurs. These symptoms may include lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, and feeling warm, among others. Syncope may also be associated with a short episode of muscle twitching. If a person does not completely lose consciousness and muscle strength it is referred to as presyncope. It is recommended that presyncope be treated the same as syncope.
Is syncope the same as presyncope?
If a person does not completely lose consciousness and muscle strength it is referred to as presyncope. It is recommended that presyncope be treated the same as syncope. Specialty:
What is the approximate match between ICd9 and ICd10?
This is the official approximate match mapping between ICD9 and ICD10, as provided by the General Equivalency mapping crosswalk. This means that while there is no exact mapping between this ICD10 code Z86.79 and a single ICD9 code, V12.59 is an approximate match for comparison and conversion purposes.
What is billable code?
Billable codes are sufficient justification for admission to an acute care hospital when used a principal diagnosis. The Center for Medicare & Medicaid Services (CMS) requires medical coders to indicate whether or not a condition was present at the time of admission, in order to properly assign MS-DRG codes.
Is a diagnosis present at time of inpatient admission?
Yes. N. Diagnosis was not present at time of inpatient admission. No. U. Documentation insufficient to determine if the condition was present at the time of inpatient admission. No. W. Clinically undetermined.
What is the ICd 10 code for angina?
Z86.79 is a billable diagnosis code used to specify a medical diagnosis of personal history of other diseases of the circulatory system. The code Z86.79 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions.#N#The ICD-10-CM code Z86.79 might also be used to specify conditions or terms like attends hypertension monitoring, h/o ventricular fibrillation, h/o: angina in last year, h/o: angina pectoris, h/o: aortic aneurysm , h/o: atrial fibrillation, etc. The code is exempt from present on admission (POA) reporting for inpatient admissions to general acute care hospitals.#N#The code Z86.79 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
Is Z86.79 a POA?
Z86.79 is exempt from POA reporting - The Present on Admission (POA) indicator is used for diagnosis codes included in claims involving inpatient admissions to general acute care hospitals. POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement. Review other POA exempt codes here.
Is diagnosis present at time of inpatient admission?
Diagnosis was not present at time of inpatient admission. Documentation insufficient to determine if the condition was present at the time of inpatient admission. Clinically undetermined - unable to clinically determine whether the condition was present at the time of inpatient admission.
Popular Posts:
- 1. icd 9 code for hypotonia unspecified
- 2. icd 10 code for arthrocentesis
- 3. what is the icd 10 code for malunion nasal fracture
- 4. icd-10 code for screening for hip dysplasia
- 5. icd 10 code for hernia of anterior abdominal wall
- 6. icd 10 code for history of corrected congenital heart defect
- 7. icd 10 code for chin laceration
- 8. icd 10 code for heparin
- 9. icd 10 code for spermatic cord thickening
- 10. icd 10 code for encounter for screening for colon cancer