What are the stages of PTTD?
There are four posterior tibial tendon dysfunction stages:Stage I: The tendon is injured but otherwise intact.Stage II: The tendon is torn (ruptured) or not working properly. The foot is deformed.Stage III: The foot is significantly deformed. ... Stage IV: There are degenerative changes to the ankle joint.
What is posterior tibial tendon dysfunction PTTD?
Posterior tibial tendon dysfunction (PTTD) represents an acquired, progressive disease of the foot and ankle that is seen commonly in middle-aged patients. It is the most common cause of adult acquired flatfoot deformity. Treatments involve conservative and surgical options depending on the severity of the disease.
What is PTTD of the ankle?
Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch. This results in flattening of the foot. PTTD is often called adult acquired flatfoot because it is the most common type of flatfoot developed during adulthood.
What does PTTD mean?
Posterior tibial tendon dysfunction is one of the most common problems of the foot and ankle. It occurs when the posterior tibial tendon becomes inflamed or torn. As a result, the tendon may not be able to provide stability and support for the arch of the foot, resulting in flatfoot.
How is posterior tibial tendon dysfunction diagnosed?
One of the most sensitive tests for posterior tibial tendon dysfunction is the single limb heel rise. To perform this test, the patient uses their arms to balance themselves against the wall. The patient will then lift the opposite foot off the ground and attempt to rise onto the toes of the affected foot.
Is PTTD always progressive?
The degeneration of the posterior tibial tendon that connects to the calf muscles and the bones of the foot weakens the arch and causes it to collapse. PTTD is progressive, so an early diagnosis is important to receive successful conservative treatment.
Are plantar fasciitis and posterior tibial tendonitis related?
Biomechanical Assessment The patient presented with extremely tight calf muscles which is a cause of tibialis posterior tendonitis, and is also a common cause of plantar fasciitis.
Is the posterior tibial tendon a flexor or extensor?
Because the tibialis posterior (TP) originates from the posterior compartment of the lower leg, the tibialis posterior is also a secondary plantar flexor of the foot along with the gastrocnemius, soleus, and plantaris muscles.
What causes posterior tibial tendonitis?
What causes Posterior Tibial Tendonitis? Posterior tibial tendon dysfunction often happens due to repetitive overuse. Dancers and athletes who play high impact sports are at risk due to the stress they place on this tendon. An acute injury, such as a fall or collision, can also tear the posterior tibial tendon.
Can you get posterior tibial tendonitis in both feet?
Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse, especially if it isn't treated early.
What is anterior tibial tendonitis?
Anterior tibialis tendonitis is an injury of the anterior tibialis tendon in the front of the ankle where it meets the foot. The tendon is important in pulling the foot up (dorsiflexion), lifting the foot off the ground while running, and in turning the foot inward (inversion).
Does PTTD ever go away?
Will Posterior Tibial Tendonitis Go Away? It can take between 6 to 9 months (or longer) for your posterior tibial tendonitis symptoms to improve and your tendon to heal.
How long does PTTD take to heal?
Posterior tibial tendon dysfunction generally takes 6-8 weeks to improve and early activity on a healing tendon can result in a set back in recovery. Non-compliance can double the recovery time and can be very frustrating for patients. Posterior tibial tendon dysfunction is a progressive condition.
Is it OK to walk with posterior tibial tendonitis?
The initial treatment of posterior tibial tendonitis is rest so that the tendon can heal. 4 Unfortunately, even normal walking may get in the way of allowing the tendon to heal adequately. In these cases, you must stop using the ankle to allow it to rest.
What happens if posterior tibial tendonitis goes untreated?
Left untreated, posterior tibial tendon dysfunction may lead to an extremely flatfoot and arthritis in the foot and ankle. Pain can increase and spread to the outer side of the ankle. Pain from this condition may increase limitations on walking, running, or other activities.
Can you walk with PTTD?
Posterior tibial tendon dysfunction (PTT) makes the inner part of your foot or ankle hurt. The pain can make it harder for you to walk or run. Working with a physical therapist can help make the pain better so you can get back to your usual activities.
What is the test for PTTD?
A common test to evaluate PTTD is the 'too many toes sign'. The 'too many toes sign' is a test used to measure abduction (deviation away from the midline of the body) of the forefoot. With damage to the posterior tibial tendon, the forefoot will abduct or move out in relationship to the rest of the foot.
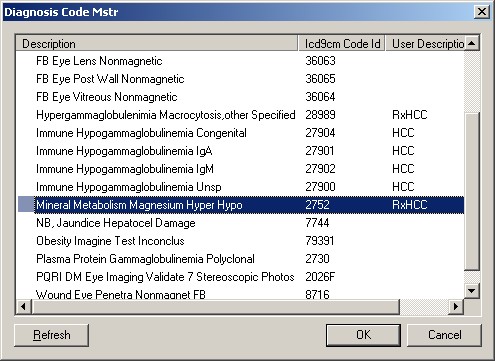
What is the code for synovial disorder?
The most appropriate code that I could come up with is 727.9, " Unspecified disorder of synovium, tendon, and bursa ".
Can PTTD recur?
If Stage I patients return to low heels without arch support, PTTD will recur. Stage II patients, or Stage I patients that do not respond to rest and support, require surgical correction to stabilize the subtalar joint prior to further damage to the posterior tibial tendon.
What is the ICd 10 code for tendinitis of the left leg?
M76.822 is a valid billable ICD-10 diagnosis code for Posterior tibial tendinitis, left leg . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
Do you include decimal points in ICD-10?
DO NOT include the decimal point when electronically filing claims as it may be rejected. Some clearinghouses may remove it for you but to avoid having a rejected claim due to an invalid ICD-10 code, do not include the decimal point when submitting claims electronically.
What is PTTD in medical terms?
PTTD is a progressive and debilitating disorder, which can be detrimental to patients due to limitations in mobility, significant pain, and weakness.
What is the difference between a stage 1 and stage 2 tibial tendon?
Stage I: Posterior tibial tendon intact and inflamed, no deformity, mild swelling. Stage II: Posterior tibial tendon dysfunctional, acquired pes planus but passively correctable, commonly unable to perform a heel raise. Stage III: Degenerative changes in the subtalar joint and the deformity is fixed.
What are the risk factors for tibial tendon dysfunction?
Risk factors for the disease include hypertension, obesity, diabetes, previous trauma, or steroid exposure. Posterior tibial tendon dysfunction (PTTD) is a progressive condition that can be classified into four stages . In the early stages, there may be pain, the area may be red, warm and swollen. There are not usually symptoms during gait ...
What is posterior tendon dysfunction?
Posterior tibial tendon dysfunction is a progressive disorder that will continue to deteriorate without treatment. Early detection and intervention will help to slow progression. Patients provided with custom orthotics and rehabilitation have been shown to have significant improvement.
Where does the tibialis posterior originate?
Tibialis posterior originates from the posterolateral tibia, posteromedial fibula and interosseous membrane. It runs through the deep posterior compartment of the leg and its tendon passes behind the medial malleolus. Blood supply to the tendon is poorest in this area and is the most common site for rupture.
Does posterior tibial tendon dysfunction affect quality of life?
Clear evidence exists that suggests that the quality of life for patients with posterior tibial tendon dysfunction is significantly affected. Evidence suggests that early conservative intervention can significantly improve quality of life regarding disability, function, and pain. All Stages initially:
Can a physiotherapist palpate the posterior tibial tendon?
The physiotherapist can palpate the posterior tibial tendon from above the medial malleolus to its insertion, to control the integrity and assess possible pain and swelling that are common for the first stages of PTTD. In the later stages, the deformity can progress and pes planus may be visible.
What is the ICd 10 code for pressure ulcers?
ICD-10-CM codes for pressure ulcers, located in Category L89, are combination codes that identify the site, stage and (in most cases) the laterality of the ulcer. Possible stages are 1-4 and unstageable.
What is stage 2 skin loss?
Stage 2: An abrasion, blister and partial thickness skin loss involving the dermis and epidermis
What is a non-pressure ulcer?
Non-pressure chronic ulcers are similar to pressure ulcers in that they require documentation of the site, severity and laterality. Category L97 and L98 are for non-pressure ulcers, and have an instructional note to code first any associated underlying condition, such as: The severity of the ulcers is described as:
What is unstageable in medical terms?
Unstageable: Based on clinical documentation the stage cannot be determined clinically (e.g., the wound is covered with eschar) or for ulcers documented as deep tissue injury without evidence of trauma.
What stage of ulcers are there on the elbow?
The pressure ulcers on the elbows are documented as partial thickness into the dermis, which supports stage 2 (stated to be healing or abrasion, blister, partial thickness skin loss involving epidermis and/or dermis)—which again matches the physician documentation.
What is CPR coding corner?
CPR’s “Coding Corner” focuses on coding, compliance and documentation issues relating specifically to physician billing. This month’s tip comes from Peggy Silley, the Director of ICD-10 Development and Training for AAPC, a training and credentialing association for the business side of health care.
Popular Posts:
- 1. icd-10 code for adrenal cyst
- 2. icd 10 code for exposure to cleaning product
- 3. icd 10 code for abnormal kub
- 4. icd 10 code for mood dysregulation disorder
- 5. icd-10-cm code for glucose intolerance
- 6. icd 9 code for bip
- 7. icd 10 code for foreign body in right index finger
- 8. icd-10 code for carotid stenosis
- 9. icd 10 code for onychomycosis of toenails
- 10. icd-10 code for history of drug use