What are the signs and symptoms of respiratory acidosis?
These are the most common symptoms associated with respiratory acidosis: 1
- Sleepiness
- Fatigue
- Lethargy
- Confusion
- Coma
- Anxiety
- Psychosis
- Headaches
- Shortness of breath
- Tremors (manifest as shaking or jerking muscle movements)
What is the cause of respiratory acidosis?
What Is Respiratory Acidosis?
- Causes. The blood becomes so acidic that the increase of carbon dioxide in your body triggers your kidneys to produce more acidic hydrogen and ammonium to absorb the bicarbonate.
- Symptoms. Usually, respiratory acidosis is a symptom of another underlying condition. ...
- Testing for Respiratory Acidosis. ...
- Prevention. ...
What is the cause of severe acute respiratory syndrome?
- Headache
- Overall feeling of discomfort
- Body aches and chills
- Sore throat
- Cough
- Pneumonia
- Difficulty breathing
- Shortness of breath
- Hypoxia (insufficient oxygen in the blood)
- Diarrhea (for 10 to 20 percent of patients)
What are symptoms of acute respiratory distress?
Symptoms of ARDS can include:
- severe shortness of breath
- rapid, shallow breathing
- tiredness, drowsiness or confusion
- feeling faint

What is the respiratory acidosis?
Respiratory acidosis is a condition that occurs when the lungs cannot remove all of the carbon dioxide the body produces. This causes body fluids, especially the blood, to become too acidic.
Is metabolic acidosis the same as respiratory acidosis?
The pCO2 determines whether an acidosis is respiratory or metabolic in origin. For a respiratory acidosis, the pCO2 is greater than 40 to 45 due to decreased ventilation. Metabolic acidosis is due to alterations in bicarbonate, so the pCO2 is less than 40 since it is not the cause of the primary acid-base disturbance.
What is the ICD-10 code for respiratory alkalosis?
ICD-10-CM Code for Alkalosis E87. 3.
What is the ICD-10-CM code for lactic acidosis?
2 - Acidosis is a sample topic from the ICD-10-CM. To view other topics, please log in or purchase a subscription. ICD-10-CM 2022 Coding Guide™ from Unbound Medicine.
What is the difference between respiratory acidosis and respiratory alkalosis?
Respiratory alkalosis occurs when you breathe too fast or too deep and carbon dioxide levels drop too low. This causes the pH of the blood to rise and become too alkaline. When the blood becomes too acidic, respiratory acidosis occurs.
Is COPD respiratory acidosis or alkalosis?
COPD is one of the main causes of respiratory acidosis.
What is ICD-10 code R99?
ICD-10 code: R99 Other ill-defined and unspecified causes of mortality.
What is the ICD-10 code for acute respiratory failure?
00 for Acute respiratory failure, unspecified whether with hypoxia or hypercapnia is a medical classification as listed by WHO under the range - Diseases of the respiratory system .
What causes alkalosis in the blood?
Alkalosis is excessive blood alkalinity caused by an overabundance of bicarbonate in the blood or a loss of acid from the blood (metabolic alkalosis), or by a low level of carbon dioxide in the blood that results from rapid or deep breathing (respiratory alkalosis).
Is respiratory acidosis integral to respiratory failure?
Since respiratory failure can be hypoxic, hypercapnic, or both, acidosis is not an integral portion of the ICD-10 code for unspecified respiratory failure, but it would be an integral part of the ICD-10 code for hypercapnic respiratory failure.
How do you code elevated lactic acid?
ICD-10-CM Code for Elevation of levels of lactic acid dehydrogenase [LDH] R74. 02.
What is severe metabolic acidosis?
Metabolic acidosis develops when too much acid is produced in the body. It can also occur when the kidneys cannot remove enough acid from the body.
What are the two main types of acidosis?
The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up. A state due to excess retention of carbon dioxide in the body. Acid base imbalance resulting from an accumulation of carbon dioxide secondary to hypoventilation.
What is metabolic acidosis?
A disorder characterized by abnormally high acidity (high hydrogen-ion concentration) of the blood and other body tissues. A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up.
What causes excessive carbon dioxide retention in the body?
Increased acidity in the blood secondary to acid base imbalance. Causes include diabetes, kidney failure and shock. Metabolic acidosis characterized by the accumulation of lactate in the body.
Can acidosis be caused by lactic acid?
It may occur spontaneously or in association with diseases such as diabetes mellitus, leukemia, or liver failure. Acidosis caused by accumulation of lactic acid more rapidly than it can be metabolized; may occur spontaneously or in association with diseases such as diabetes mellitus, leukemia, or liver failure.
What is the name of the condition in which the blood is too acidic?
A condition in which the blood is too acidic. It may be caused by severe illness or sepsis (bacteria in the bloodstream). A disorder characterized by abnormally high acidity (high hydrogen-ion concentration) of the blood and other body tissues. A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up. A state due to excess retention of carbon dioxide in the body. Acid base imbalance resulting from an accumulation of carbon dioxide secondary to hypoventilation. Acidosis caused by accumulation of lactic acid more rapidly than it can be metabolized. It may occur spontaneously or in association with diseases such as diabetes mellitus, leukemia, or liver failure. Acidosis caused by accumulation of lactic acid more rapidly than it can be metabolized; may occur spontaneously or in association with diseases such as diabetes mellitus, leukemia, or liver failure. An abnormal increase in the acidity of the body's fluids An abnormally high acidity (excess hydrogen-ion concentration) of the blood and other body tissues. An abnormally high acidity of the blood and other body tissues. Acidosis can be either respiratory or metabolic. Excess retention of carbon dioxide in the body resulting from ventilatory impairment. Increased acidity in the blood secondary to acid base imbalance. Causes include diabetes, kidney failure and shock. Metabolic acidosis characterized by the accumulation of lactate in the body. It is caused by tissue hypoxia. Pathologic condition resulting from accumulation of acid or depletion of the alkaline reserve (bicarbonate) content of the blood and body tissues, and characterized by an increase in hydrogen ion concentration (decrease in ph). Respi Continue reading >>
What is the ICD-10-CM/PCS MS-DRGv28?
Draft ICD-10-CM/PCS MS-DRGv28 Definitions Manual Newborn (suspected to be) affected by maternal hypertensive disorders Newborn (suspected to be) affected by maternal renal and urinary tract diseases Newborn (suspected to be) affected by maternal infectious and parasitic diseases Newborn (suspected to be) affected by other maternal circulatory and respiratory diseases Newborn ( suspected to be) affected by maternal nutritional disorders Newborn (suspected to be) affected by maternal injury Newborn (suspected to be) affected by surgical procedure on mother Newborn (suspected to be) affected by other medical procedures on mother, not elsewhere classified Newborn (suspected to be) affected by periodontal disease in mother Newborn (suspected to be) affected by other maternal conditions Newborn (suspected to be) affected by unspecified maternal condition Newborn (suspected to be) affected by incompetent cervix Newborn (suspected to be) affected by premature rupture of membranes Newborn (suspected to be) affected by oligohydramnios Newborn (suspected to be) affected by polyhydramnios Newborn (suspected to be) affected by ectopic pregnancy Newborn (suspected to be) affected by multiple pregnancy Newborn (suspected to be) affected by maternal death Newborn (suspected to be) affected by malpresentation before labor Newborn (suspected to be) affected by other maternal complications of pregnancy Newborn (suspected to be) affected by maternal complication of pregnancy, unspecified Newborn (suspected to be) affected by placenta previa Newborn (suspected to be) affected by other forms of placental separation and hemorrhage Newborn (suspected to be) affected by unspecified morphological and functional abnormalities of placenta Newborn (suspected to be) affected by other morphological a Continue reading >>
What is respiratory failure?
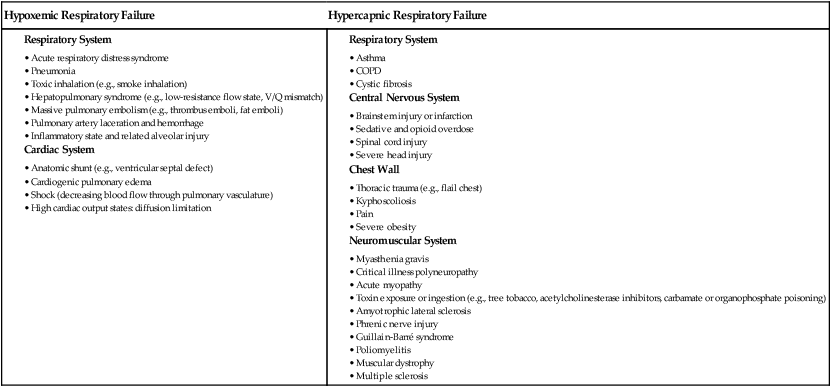
Some issues include: Distinction between, and clinical diagnostic criteria for, acute and chronic respiratory failure Recognition of an acute exacerbation of chronic respiratory failure Classification of acute respiratory failure as hypoxemic or hypercapnic Identification of respiratory failure as a post-procedural complication Necessity of precise diagnostic terminology for the correct coding of acute and chronic respiratory failure Numerous clinical and non-clinical consequences of documenting the diagnoses of acute and chronic respiratory failure Respiratory failure is commonly defined as respiratory dysfunction resulting in abnormalities of oxygenation and/ or carbon dioxide (CO2) elimination and is classified as either hypoxemic (type I) or hypercapnic (type II), or a combination of both. These distinctions are clinically important and have diagnostic and therapeutic implications, but current coding rules consider them non-essential terms that do not affect the code assigned. Physicians won't be required to use them with ICD-10, either, though the coding system will allow for these distinctions. Respiratory failure occurs frequently in association with chronic obstructive pulmonary disease (COPD), heart failure, pneumonia, and sepsis and after cardiac arrest. The correct diagnosis is essential to accurately portray a patient's severity of illness and influences quality scores, performance indicators, clinical outcome measures and hospital revenue. Even chronic respiratory failure contributes to severity classification. However, non-specific terms (such as hypoxia, severe dyspnea, respiratory insufficiency or distress) result in the assignment of codes that do not reflect any significant res Continue reading >>
What is AAPC coder complete?
AAPC Coder Complete provides all the coding and reimbursement tools needed for inpatient coders, outpatient coders and CDI experts. Quickly view the OPPS fee schedules for freestanding ASCs and hospital based outpatient services in one place. For each CPT code, you can identify the applicable modifiers, status indicators and payment indicators. For procedures that require devices, you can view if there is a credit adjustment policy for the device. Avoid bundling and determine proper modifier use by using the OPPS CCI checker for up to 25 codes at one time. The cross-reference tools allow you to forward and backward map CPT to ICD-9-CM Volume 1 and 3, ICD-9-CM Volume 1 to ICD-10-CM and ICD-9-CM Volume 1 to the appropriate DRG options. Easily identity the DRG options, including CC and MCC, for each ICD-9-CM Volume 1 code. APC look up provides necessary detail on one page including long descriptor, payment and coverage info and more. CPT Assistant is the official word from the AMA on proper CPT code usage. AAPC Coder's Code Connect add-on allows you to search all CPT Assistant articles from 1990 to present by CPT code to narrow the options to only related articles for quick coding guidance. The HCPCS Coding Clinic delivers the official guidance published quarterly by the American Hospital Association (AHA) Central Office on correct HCPCS level II code usage. Each issue offers consistent and accurate advice for the proper use of HCPCS and includes information on HCPCS reporting for hospitals HCPCS Level 1 (CPT) and Level II codes, the latest code assignments from emerging technologies, and real examples. Continue reading >>
What is the ICd 10 code for acidosis?
E87.2 is a valid billable ICD-10 diagnosis code for Acidosis . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
Do you include decimal points in ICD-10?
DO NOT include the decimal point when electronically filing claims as it may be rejected. Some clearinghouses may remove it for you but to avoid having a rejected claim due to an invalid ICD-10 code, do not include the decimal point when submitting claims electronically. See also: Acarbia E87.2. Acid.
What causes lactic acidosis?
Lactic acidosis develops when there is increased production of lactate, decreased clearance, or a combination of both. The most common cause is the shock state. It can also result from impaired hepatic function, like in cirrhosis, or from regional ischemia, drugs and toxins, or from inborn errors of metabolism.
Is E87.2 a condition?
If the condition indexes under a general term coded at E87.2, like acidosis or acidemia, it is integral to it. Examples are renal tubular acidosis or propionic acidemia. They code to different codes, but they are indexed below E87.2. Genetic disorders of metabolism can have variable manifestations.
Is acidemia an inherent disease?
Genetic disorders of metabolism can have variable manifestations. If acidemia is part of the name of the condition and the condition is indexed below E87.2, acidosis should be considered inherent. Other inborn errors, however, may have lactic acidosis as a component.
Popular Posts:
- 1. icd 9 code for ophthalmology
- 2. icd 10 code for basal cell carcinoma of neck
- 3. icd 10 code for non alcoholic hepatic
- 4. icd 10 code for neoplasm skin forehead
- 5. assign an icd-10 code for congenital interstitial emphysema
- 6. icd 10 code for postoperative right wrist
- 7. icd 10 code for i95.9
- 8. 2018 icd 10 cm code for diffuse lymph node adenopathy
- 9. icd 10 code for diverticular disease of sigmoid colon
- 10. icd 10 code for left leg above knee amputation