How to stop lactic acidosis in 4 steps?
Oct 01, 2021 · ICD-10-CM R65.21 is grouped within Diagnostic Related Group (s) (MS-DRG v39.0): 870 Septicemia or severe sepsis with mv >96 hours 871 Septicemia or severe sepsis without mv >96 hours with mcc 872 Septicemia or severe sepsis without mv >96 hours without mcc Convert R65.21 to ICD-9-CM Code History
What is lactic acid level indicates sepsis?
May 30, 2019 · Remember, there is no separate code in ICD-10 for “lactic acidosis.”. You simply get the generic “acidosis” code here with no differentiation as to type. From a coding standpoint, ICD-10 code A41.x series do not have Excludes 1 notes for acidosis and the acidosis E codes do not have Excludes 1 notes for sepsis.
Why is lactic acid elevated in sepsis?
Oct 01, 2021 · R65.20 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R65.20 became effective on October 1, 2021. This is the American ICD-10-CM version of R65.20 - other international versions of ICD-10 R65.20 may differ. Applicable To Severe sepsis NOS
What happens when lactate levels are high?
Oct 01, 2021 · E87.2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM E87.2 became effective on October 1, 2021. This is the American ICD-10-CM version of E87.2 - other international versions of ICD-10 E87.2 may differ. Applicable To Acidosis NOS Lactic acidosis
Can lactic acidosis be coded with sepsis?
If the lactic acidosis is due to an unrelated event in tandem with sepsis such as respiratory failure, severe anemia, asphyxia, limb ischemia, poisoning, hemorrhage, alcohol, etc., then it would be separately reportable as a “multifactorial” metabolic event, but only if documented as such.May 30, 2019
What is lactic acidosis sepsis?
Lactic acidosis in sepsis and septic shock has traditionally been explained as a result of tissue hypoxia when whole-body oxygen delivery fails to meet whole-body oxygen requirements (Fig 2).
What is the ICD 10 for elevated lactic acid?
R74.02Elevation of levels of lactic acid dehydrogenase [LDH] R74. 02 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
Is lactic acidosis the same as sepsis?
Lactic acidosis is a common finding in critically ill patients during severe sepsis/septic shock, and a powerful predictor of mortality.
What is severe metabolic acidosis?
The buildup of acid in the body due to kidney disease or kidney failure is called metabolic acidosis. When your body fluids contain too much acid, it means that your body is either not getting rid of enough acid, is making too much acid, or cannot balance the acid in your body.
What is the ICD 10 code for sepsis?
A41.9Septicemia – There is NO code for septicemia in ICD-10. Instead, you're directed to a combination 'A' code for sepsis to indicate the underlying infection, such A41. 9 (Sepsis, unspecified organism) for septicemia with no further detail.
Is LDH the same as lactic acid?
What is a lactate dehydrogenase (LDH) test? This test measures the level of lactate dehydrogenase (LDH), also known as lactic acid dehydrogenase, in your blood or sometimes in other body fluids. LDH is a type of protein, known as an enzyme. LDH plays an important role in making your body's energy.Dec 17, 2020
What is the ICD 10 code for elevated uric acid?
Hyperuricemia without signs of inflammatory arthritis and tophaceous disease. E79. 0 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is metabolic acidosis?
A disorder characterized by abnormally high acidity (high hydrogen-ion concentration) of the blood and other body tissues. A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up.
What is acid base imbalance?
Acid base imbalance resulting from an accumulation of carbon dioxide secondary to hypoventilation. Acidosis caused by accumulation of lactic acid more rapidly than it can be metabolized. It may occur spontaneously or in association with diseases such as diabetes mellitus, leukemia, or liver failure.
What is a type 1 exclude note?
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as E87.2. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What is the blood level of lactate?
Hyperlactatemia is a blood level of lactate from 2 to 4 mmol/L. Lactic acidosis is defined as lactate level > 4 mmol/L. There is often acidemia, which means the blood measures acidic (relative to normal pH of 7.4) with a pH < 7.35, but if compensatory mechanisms are not overwhelmed, the pH may be closer to normal.
What causes lactic acidosis?
Lactic acidosis develops when there is increased production of lactate, decreased clearance, or a combination of both. The most common cause is the shock state. It can also result from impaired hepatic function, like in cirrhosis, or from regional ischemia, drugs and toxins, or from inborn errors of metabolism.
What is the pH of a molecule?
Normal body pH is 7.4. Those charged particles can interact chemically with other particles. The companion portion of the molecule to the hydrogen ion is called the conjugate base. Since the hydrogen ion is positively charged, the other portion is the anion; it is negatively charged.
Who is Erica Remer?
She was a physician advisor of a large multi-hospital system for four years before transitioning to independent consulting in July 2016. Her passion is educating CDI specialists, coders, and healthcare providers with engaging, case-based presentations on documentation, CDI, and denials management topics. She has written numerous articles and serves as the co-host of Talk Ten Tuesdays, a weekly national podcast. Dr. Remer is a member of the ICD10monitor editorial board, a former member of the ACDIS Advisory Board, and the board of directors of the American College of Physician Advisors.
What is the brain's energy source?
The brain preferentially uses glucose. Glucose is broken down into a compound called pyruvate, releasing some energy. Pyruvate can either be completely metabolized oxidatively down to lots of energy, carbon dioxide, and water, or anaerobically metabolized to lactate, releasing less energy.
What causes low pH in blood?
Lactic acidosis is typically the result of an underlying acute or chronic medical condition, medication, or poisoning. The symptoms are generally attributable to these underlying causes, but may include nausea, vomiting, rapid deep breathing, and generalised weakness. The diagnosis is made on biochemical analysis of blood (often initially on arterial blood gas samples), and once confirmed, generally prompts an investigation to establish the underlying cause to treat the acidosis. In some situations, hemofiltration (purification of the blood) is temporarily required. In rare chronic forms of lactic acidosis caused by mitochondrial disease, a specific diet or dichloroacetate may be used. The prognosis of lactic acidosis depends largely on the underlying cause; in some situations (such as severe infections), it indicates an increased risk of death. Classification The Cohen-Woods classification categorizes causes of lactic acidosis as: [1] Type A: Decreased tissue oxygenation (e.g., from decreased blood flow) Type B B1: Underlying diseases (sometimes causing type A) B2: Medication or intoxication B3: Inborn error of metabolism Signs and symptoms Lactic acidosis is commonly found in people who are unwell, such as those with severe heart and/or lung disease, a severe infection with sepsis, the systemic inflammatory response syndrome due to another cause, severe physical trauma, or severe depletion of body fluids. [2] Symptoms in humans include all those of typical m Continue reading >>
What is the ICd 10 code for genitourinary system disease?
N00-N99 Diseases of the genitourinary system N25-N29 Other disorders of kidney and ureter N25- Disorders resulting from impaired renal tubular function Other disorders resulting from impaired renal tubular function N25.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Oth disorders resulting from impaired renal tubular function The 2018 edition of ICD-10-CM N25.89 became effective on October 1, 2017. This is the American ICD-10-CM version of N25.89 - other international versions of ICD-10 N25.89 may differ. The following code (s) above N25.89 contain annotation back-references In this context, annotation back-references refer to codes that contain: certain conditions originating in the perinatal period ( P04 - P96 ) certain infectious and parasitic diseases ( A00-B99 ) complications of pregnancy, childbirth and the puerperium ( O00-O9A ) congenital malformations, deformations and chromosomal abnormalities ( Q00-Q99 ) endocrine, nutritional and metabolic diseases ( E00 - E88 ) injury, poisoning and certain other consequences of external causes ( S00-T88 ) symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified ( R00 - R94 ) disorders of kidney and ureter with urolithiasis ( N20-N23 ) Hyperkalemic distal renal tubular acidosis Metabolic acidosis, nag, acidifying salts Metabolic acidosis, normal anion gap (nag) A group of genetic disorders of the kidney tubules characterized by the accumulation of metabolically produced acids with elevated plasma chloride, hyperchloremic metabolic acidosis. Defective renal acidification of urine (proximal tubules) or low renal acid excretion (distal tubules) can lead to complications such as hypokalemia, hypercalcinuria with nephr Continue reading >>
What is a type 1 exclude note?
A type 1 Excludes note is a pure excludes. It means 'NOT CODED HERE!' An Excludes1 note indicates that the code excluded should never be used at the same time as the code above the Excludes1 note. An Excludes1 is used when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition. A type 2 Excludes note represents 'Not included here'. An Excludes2 note indicates that the condition excluded is not part of the condition it is excluded from but a patient may have both conditions at the same time. When an Excludes2 note appears under a code it is acceptable to use both the code and the excluded code together. A code also note instructs that 2 codes may be required to fully describe a condition but the sequencing of the two codes is discretionary, depending on the severity of the conditions and the reason for the encounter. Certain conditions have both an underlying etiology and multiple body system manifestations due to the underlying etiology. For such conditions the ICD-10-CM has a coding convention that requires the underlying condition be sequenced first followed by the manifestation. Wherever such a combination exists there is a 'use additional code' note at the etiology code, and a 'code first' note at the manifestation code. These instructional notes indicate the proper sequencing order of the codes, etiology followed by manifestation. In most cases the manifestation codes will have in the code title, 'in diseases classified elsewhere.' Codes with this title area component of the etiology / manifestation convention. The code title indicates that it is a manifestation code. 'In disease Continue reading >>
What is AAPC coder complete?
AAPC Coder Complete provides all the coding and reimbursement tools needed for inpatient coders, outpatient coders and CDI experts. Quickly view the OPPS fee schedules for freestanding ASCs and hospital based outpatient services in one place. For each CPT code, you can identify the applicable modifiers, status indicators and payment indicators. For procedures that require devices, you can view if there is a credit adjustment policy for the device. Avoid bundling and determine proper modifier use by using the OPPS CCI checker for up to 25 codes at one time. The cross-reference tools allow you to forward and backward map CPT to ICD-9-CM Volume 1 and 3, ICD-9-CM Volume 1 to ICD-10-CM and ICD-9-CM Volume 1 to the appropriate DRG options. Easily identity the DRG options, including CC and MCC, for each ICD-9-CM Volume 1 code. APC look up provides necessary detail on one page including long descriptor, payment and coverage info and more. CPT Assistant is the official word from the AMA on proper CPT code usage. AAPC Coder's Code Connect add-on allows you to search all CPT Assistant articles from 1990 to present by CPT code to narrow the options to only related articles for quick coding guidance. The HCPCS Coding Clinic delivers the official guidance published quarterly by the American Hospital Association (AHA) Central Office on correct HCPCS level II code usage. Each issue offers consistent and accurate advice for the proper use of HCPCS and includes information on HCPCS reporting for hospitals HCPCS Level 1 (CPT) and Level II codes, the latest code assignments from emerging technologies, and real examples. Continue reading >>
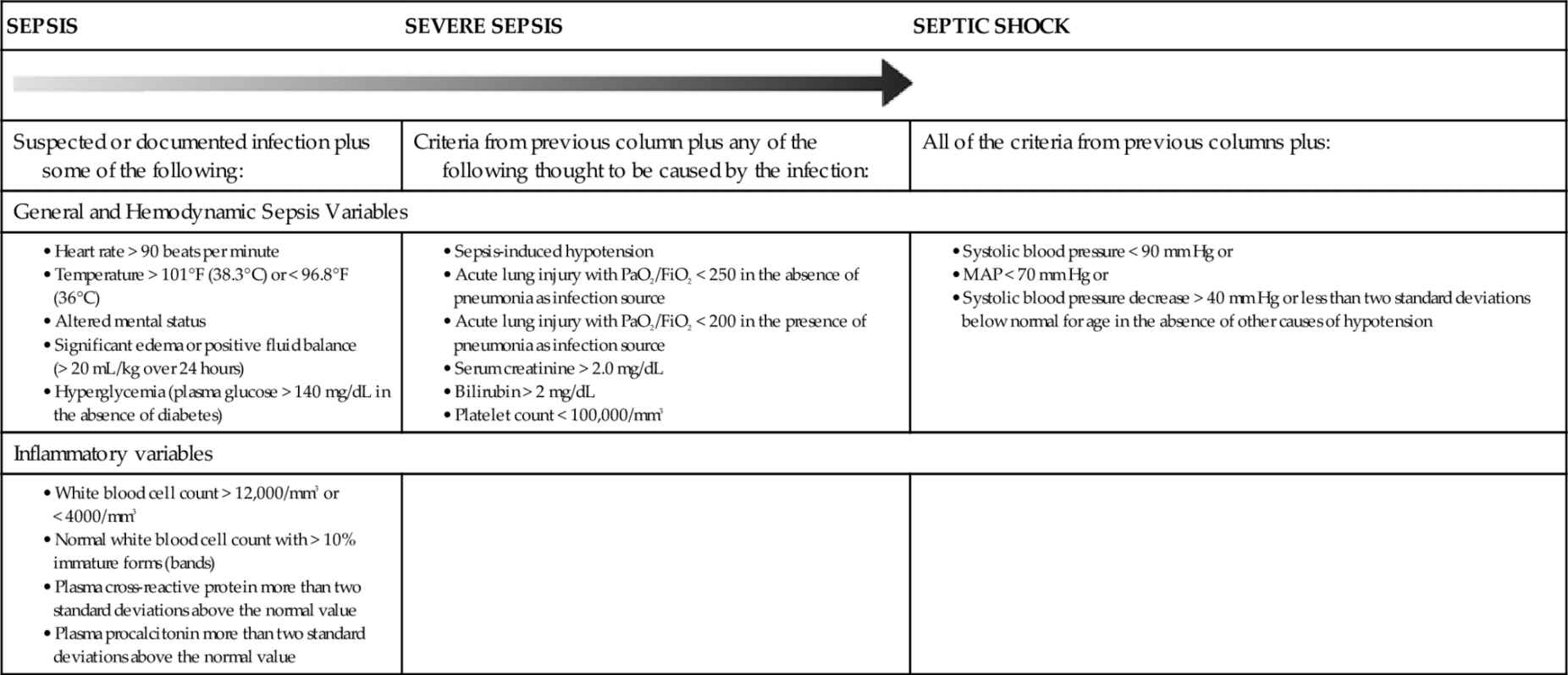
What is the life threatening condition that occurs when the body’s response to an infection damages its own tissues?
Sepsis is a potentially life-threatening condition that occurs when the body’s response to an infection damages its own tissues. Without timely treatment, sepsis can progress rapidly and lead to tissue damage, organ failure, and then death. Proper coding of sepsis and SIRS requires the coder to understand the stages of sepsis and common documentation issues.
Is septicemia difficult to code?
Sepsis, systemic inflammatory response syndrome (SIRS), and septicemia have historically been difficult to code. Changing terminology, evolving definitions, and guideline updates over the past 20 years have created confusion with coding sepsis.
What is SIRS in the body?
SIRS is an inflammatory state affecting the whole body. It is an exaggerated defense response of the body to a noxious stressor, such as infection or trauma, that triggers an acute inflammatory reaction, which may progress and result in the formation of blood clots, impaired fibrinolysis, and organ failure.
What is the response to sepsis?
Sepsis is an extreme response to infection that develops when the chemicals the immune system releases into the bloodstream to fight infection cause widespread inflammation. This inflammation can lead to blood clots and leaky blood vessels, and without timely treatment, may result in organ dysfunction and then death. Severe cases of sepsis often result from a body-wide infection that spreads through the bloodstream, but sepsis can also be triggered by an infection in the lungs, stomach, kidneys, or bladder. Thus, it is not necessary for blood cultures to be positive to code sepsis (guideline I.C.1.d.1.a.i).
What is septic shock?
Septic shock refers to circulatory failure associated with severe sepsis. It is a life-threatening condition that happens when the exaggerated response to infection leads to dangerously low blood pressure (hypotension). Septic shock is a form of organ failure.
What is systemic infection?
A systemic infection can occur as a complication of a procedure or due to a device, implant, or graft. This includes systemic infections due to postoperative wound infections, infusions, transfusions, therapeutic injections, implanted devices, and transplants.
What are the symptoms of a localized infection?
Documentation issues: A patient with a localized infection usually presents with tachycardia, leukocytosis, tachypnea, and/or fever. These are typical symptoms of any infection. It is up to the clinical judgment of the physician to decide whether the patient has sepsis.
Why is QSOFA important?
This is done to prognosticate and direct transfer to the intensive care setting.
What is the definition of sepsis?
In 2016, the Third International Consensus Definitions for Sepsis and Septic Shock, Sepsis-3, in JAMA defined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.”.
Who is Erica Remer?
She was a physician advisor of a large multi-hospital system for four years before transitioning to independent consulting in July 2016. Her passion is educating CDI specialists, coders, and healthcare providers with engaging, case-based presentations on documentation, CDI, and denials management topics. She has written numerous articles and serves as the co-host of Talk Ten Tuesdays, a weekly national podcast. Dr. Remer is a member of the ICD10monitor editorial board, a former member of the ACDIS Advisory Board, and the board of directors of the American College of Physician Advisors.
What does it mean when your creatinine is high?
When you notice the creatinine has bumped, or the INR is high, what you are thinking is that there is acute renal or liver dysfunction. No one ever diagnoses critical illness polyneuropathy or myopathy, and no one thinks of ileus as an organ dysfunction.

Popular Posts:
- 1. icd 10 code for hepatobiliary cancer
- 2. what is the diagnosis code for diagnosis type icd-10-cm
- 3. icd 10 code for personal history of sudden cardiac arrest
- 4. icd 10 code for foot neuropathy
- 5. icd 10 code for shr
- 6. icd 10 code for philadelphia chromosome negative b cell all
- 7. icd 10 code for obesity hypoventillation syndrome
- 8. icd-10 code for cancer of the posterior wall of nasopharynx
- 9. icd 10 code for medication intolerance
- 10. icd 10 code for cervical strain