What is the ICD 10 code for pressure ulcer Stage 3?
Pressure ulcer stage 3 of right lower leg Pressure ulcer stage 3 of toes ICD-10-CM L89.893 is grouped within Diagnostic Related Group (s) (MS-DRG v38.0): 573 Skin graft for skin ulcer or cellulitis with mcc
What is the ICD 10 code for pressure ulcer of right heel?
Pressure ulcer of right heel stage 3 ICD-10-CM L89.613 is grouped within Diagnostic Related Group (s) (MS-DRG v38.0): 573 Skin graft for skin ulcer or cellulitis with mcc 574 Skin graft for skin ulcer or cellulitis with cc
What is the ICD 10 code for a type 2 ulcer?
When a type 2 excludes note appears under a code it is acceptable to use both the code (L89) and the excluded code together. decubitus (trophic) ulcer of cervix (uteri) ( ICD-10-CM Diagnosis Code N86 diabetic ulcers ( ICD-10-CM Diagnosis Code E08.621 non-pressure chronic ulcer of skin ( ICD-10-CM Diagnosis Code L97
What is the ICD 10 code for ulcer of the ankle?
Pressure ulcer of right ankle, stage 3. L89.513 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.

What is the ICD-10 code for stage 3 Pressure ulcer?
Pressure ulcer of unspecified site, stage 3 L89. 93 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L89. 93 became effective on October 1, 2021.
What is the ICD-10 code for stage 3 Pressure ulcer left heel?
ICD-10 code L89. 623 for Pressure ulcer of left heel, stage 3 is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
What is the ICD-10 code for ulcer of foot?
ICD-10-CM Code for Non-pressure chronic ulcer of other part of unspecified foot with unspecified severity L97. 509.
How do you code a foot ulcer?
Of these options, the most commonly used codes for diabetic foot ulcers are E10. 621 (Type 1 diabetes mellitus with foot ulcer) and E11. 621 (Type 2 diabetes mellitus with foot ulcer).
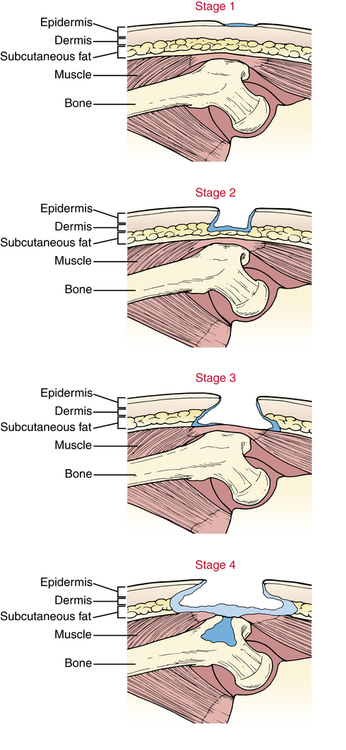
What is a Stage 3 pressure ulcer?
Stage 3 bedsores (also known as stage 3 pressure sores, pressure injuries, or decubitus ulcers) are deep and painful wounds in the skin. They are the third of four bedsore stages. These sores develop when a stage 2 bedsore penetrates past the top layers of skin but has yet not reached muscle or bone.
When coding a pressure ulcer what must be coded?
“Two codes are needed to completely describe a pressure ulcer: A code from subcategory 707.0, Pressure ulcer, to identify the site of the pressure ulcer and a code from subcategory 707.2, Pressure ulcer stages.
What is the ICD-10 diagnosis code for right foot ulcer?
Non-pressure chronic ulcer of other part of right foot with unspecified severity. L97. 519 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L97.
What is an ulcer on the foot?
Foot ulcers are open sores or lesions that will not heal or that return over a long period of time. These sores result from the breakdown of the skin and tissues of the feet and ankles and can get infected. Symptoms of foot ulcers can include swelling, burning, and pain.
What is the ICD-10 code for right foot Pain?
ICD-10 code M79. 671 for Pain in right foot is a medical classification as listed by WHO under the range - Soft tissue disorders .
How are pressure ulcers classified in the ICD?
ICD-10-CM codes for pressure ulcers, located in Category L89, are combination codes that identify the site, stage and (in most cases) the laterality of the ulcer. Possible stages are 1-4 and unstageable.
What is the ICD-10 for diabetic foot ulcer?
ICD-10 code E11. 621 for Type 2 diabetes mellitus with foot ulcer is a medical classification as listed by WHO under the range - Endocrine, nutritional and metabolic diseases .
What is the ICD-10 code for left foot ulcer?
ICD-10-CM Code for Non-pressure chronic ulcer of other part of left foot with unspecified severity L97. 529.
What is non pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
Why are pressure ulcers considered a patient safety indicator?
Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
What causes diabetic foot ulcers?
A “diabetic foot ulcer,” which is caused exclusively by hyperglycemia, in the absence of neuropathy or ischemia, is a rarity. That term almost always refers to an ulcer on the foot of a diabetic that derives from neuro/ischemic etiology, as opposed to being strictly and principally due to pressure injury.
Why do diabetics get ulcers on their feet?
The American Podiatric Medical Association adds that “ (diabetic foot) ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes.” They go on to note that “vascular disease can complicate a foot ulcer, reducing the body’s ability to heal and increasing the risk for an infection.”
What is a malum perforans pedis ulcer?
Neuropathy results in malum perforans pedis (a.k.a. bad perforating foot) ulcers. These are painless, non-necrotic, circular lesions circumscribed by hyperkeratosis. They often overlie a metatarsal head. Ischemic wounds manifest local signs of ischemia such as thin, shiny, hairless skin with pallor and coldness. These are often found at areas of friction and may be painful.
What is pressure injury?
Shear and pressure are the mechanisms that lead to what are known as “pressure injuries.” In 2016, the National Pressure Ulcer Advisory Panel (NPUAP) recommended transitioning to the terminology of “pressure injury” because although underlying tissue may be damaged, overlying skin may appear intact. Pressure injuries with skin breakdown are considered pressure ulcers. An additional L89 code specifies the stage (depth of tissue injury) and the anatomical site.
Why should we specifically carve out pressure ulcers?
Why should we specifically carve out pressure ulcers? Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
Popular Posts:
- 1. what is icd-9 code/ diagnosis r31.0 used for
- 2. icd 10 diagnosis code for memory loss
- 3. icd 10 code for malignant neoplasm of unspecified site of left eye with metastasis
- 4. what is the icd 10 code for femoral artery occlusion
- 5. icd 10 code for infected insect bite left ankle
- 6. icd 10 code for j3301
- 7. icd 10 code for rectal colon cancer
- 8. icd 10 code for acute renal dysfunction
- 9. what is the icd 10 code for ligamentum teres tear
- 10. icd-9 code for breast cyst